
Anterior segment imaging using non-invasive high-resolution optical coherence tomography
One of the most important developments in the ophthalmology and visual sciences field has been the application of new techniques for imaging the anterior and posterior segment of the eye with non-contact devices. These techniques have been developed quickly considering that are non-invasive and provide high-resolution images of the different parts of the human eye. Definitely, the most spread and used technique for non-contact imaging of the human eye is the optical coherence tomography (OCT). OCT technique was first demonstrated in 1991 by Huang et al. (1). Based on low-coherence interferometry, OCT has become a prominent biomedical imaging technique with micrometric resolution and cross-sectional imaging capabilities, being particularly suitable for ophthalmic and other tissue imaging applications requiring millimetre penetration depth. Thus, OCT is especially useful in Ophthalmology, given the ease with which light reaches the ocular structures in the anterior and posterior segments. The advantage in its application is that the light impinges directly on the tissue, without the need to use any transducer, only requiring an optical medium sufficiently transparent to obtain a detectable signal. As a curiosity, OCT has also been used for various art conservation projects, where it is used to analyse, for instance, the different layers of a painting.
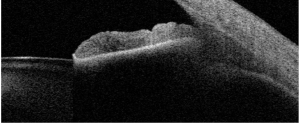
Anterior segment OCT imaging has been used for anatomical evaluation and for clinical diagnosis, but also contact lens fitting and phakic intraocular lens implantation are also two areas that have been benefited from this technology. Mainly, non-contact OCT has been applied for measuring different ocular parameters on the anterior segment. Specifically, corneal thickness (2), anterior chamber depth (ACD) (3), white-to-white (3) and angle assessment (4) have been measured and evaluated under different conditions and populations. In addition to these measurements, other parameters, such as ciliary muscle area and lens thickness or lens curvature have been also determined (Figure 1). Accurate measurements of these parameters in the eye are extremely useful both for clinical diagnosis and applications, and also for basic research to understand how they eye works. This may help to develop future solutions for the aging eye, new optical designs for intraocular lenses, and to understand the emmetropization process in the human eye, for instance.
Then, current and future applications of this powerful technology are welcomed and will appear to show new advances for clinicians. In this sense, it is interesting to comment a recent study published by Goto et al. (5) where a new formula for predicting postoperative ACD with angle-to-angle depth using an anterior segment optical coherence tomographer has been proposed. These authors carried out a retrospective consecutive case series study where 304 eyes (276 patients) implanted with acrylic intraocular lenses were included. They performed an analysis using multiple linear regression considering five preoperative parameters (angle-to-angle depth, angle-to-angle width, preoperative ACD, axial length and corneal power) in two random groups: training and validation sets, both with the same number of eyes. A Tomey optical coherence tomographer (SS-1000, Tomey Corp, Nagoya, Japan) was used in this study to acquire the values of the different anterior segment parameters. In addition, an IOL Master 500 (Carl Zeiss Meditec, Dublin, CA, USA) was used to measure axial length and keratometry. Taking into account these variables the authors developed a new regression formula to predict postoperative ACD, that was checked with the validation set using the coefficient of determination between the measured postoperative ACD and the predicted postoperative ACD, compared with those found using the SRK/T and Haigis formulas.
These authors discussed that this is the first study to investigate angle-to-angle depth as a unique and possibly independent preoperative parameter associated with postoperative intraocular lens position. They concluded that this parameter measured using anterior segment OCT can be a good predictor of postoperative ACD, and the new developed formula can play an important role for intraocular lens calculation. In addition the authors pointed out some limitations in the study, such as the use of only one type of intraocular lens, the use of a semiautomatic image analysis software, and the need to confirm the validity of the derived formula when applied in eyes with severe myopia and severe hyperopia and in eyes with previous corneal refractive surgery.
We believe that the use of non-invasive techniques that provide clinicians and researchers accurate measurements of the different parts of the human eye, in this case from the anterior segment, are extremely useful and can help to improve the derived clinical outcomes.
Acknowledgments
Funding: The authors acknowledge financial support from the Ministerio de Economía y Competitivad (Research Project SAF2013-44510-R with FEDER Funds).
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by Section Editor Yi Sun, MD (Department of Ophthalmology, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, China).
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.02.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science 1991;254:1178-81. [Crossref] [PubMed]
- Rio-Cristobal A, Martin R. Corneal assessment technologies: current status. Surv Ophthalmol 2014;59:599-614. [Crossref] [PubMed]
- Domínguez-Vicent A, Pérez-Vives C, Ferrer-Blasco T, et al. Device interchangeability on anterior chamber depth and white-to-white measurements: a thorough literature review. Int J Ophthalmol 2016;9:1057-65. [PubMed]
- Wang D, Lin S. New developments in anterior segment optical coherence tomography for glaucoma. Curr Opin Ophthalmol 2016;27:111-7. [Crossref] [PubMed]
- Goto S, Maeda N, Koh S, et al. Prediction of Postoperative Intraocular Lens Position with Angle-to-Angle Depth Using Anterior Segment Optical Coherence Tomography. Ophthalmology 2016;123:2474-80. [Crossref] [PubMed]
Cite this article as: Montés-Micó R, Esteve-Taboada JJ. Anterior segment imaging using non-invasive high-resolution optical coherence tomography. Ann Eye Sci 2017;2:11.


