
RAF near point rule for near point of convergence—a short review
Introduction
RAF near point rule (RNPR) also known as Royal Air Force (RAF) rule is a routinely employed instrument in ophthalmology and optometry practices to measure near point of convergence (NPC) and near point of accommodation (NPA). It is also used as a standard tool for research purpose and to provide therapeutic home-based orthoptic exercises (1,2).The assessment of NPC is an important part of a routine eye examination as it serves as the primary assessment for the diagnosis and management of convergence insufficiency (3-6). Convergence insufficiency is a non-strabismic binocular disorder and a common cause of asthenopic symptoms (7). Convergence insufficiency, affecting about 5% of the global population, may have a negative impact on the health-related quality of life, potentially causing difficulties with reading and associated near work (8,9).
The Convergence Insufficiency Treatment Trial (CITT) group included a receded NPC of 6 cm or more as an important criterion for diagnosis of convergence insufficiency along with an exophoria at near greater than distance by at least 4 prism diopters, and a decreased positive fusional vergence (PFV) at near (10). Most of the optometrists, however, consider NPC as the main factor in making a diagnosis of convergence insufficiency (11). Considering the clinical significance of measuring NPC, understanding the design, procedure, merits and demerits of RNPR can help us in properly measuring the NPC.
A brief history
The RNPR was first mentioned in the literature by J. C. Neely in 1956. It stated that the RNPR was originally developed in the United Kingdom (UK) in the mid-1950s to assess the visual abilities of the individuals conscripted into the US military to carry out routine clerical responsibilities. The instrument was used to assess the visual functions like convergence and accommodation as well as to establish the correlation between distance and near visual acuity (12). After the introduction, its use has widely expanded and continues as a preferred ophthalmic tool. Apart from the UK and Ireland, it is popular in Asia, including Bhutan, India, and Nepal. The RNPR is marketed by Haag-Streit® as RAF binocular gauge.
The design of RNPR
Target drums (Figure 1)
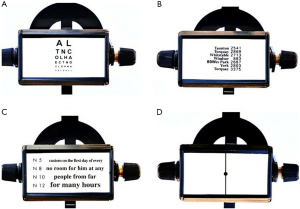
The RNPR consists of a rotating four-sided cubical drum held on a slider. The slider is attached to a square section metal rule. Each of the four sides has different accommodative targets with black prints on a white background which include:
- Side 1: a reduced Snellen chart. The distance Snellen chart is reduced to one-seventeenth of its actual size and is accurate at 35 cm (13). The reduced Snellen chart subtends an angle of 5 min of arc at 35 cm, the same that a distance Snellen chart subtends at 6 m;
- Side 2: a section of the General Post Office (G.P.O) telephone directory. One face consists of a photographed section of the G.P.O telephone directory (c. 1956).
- Side 3: Times Roman typeface. The Faculty of Ophthalmologists [1951] suggested that the standard reading types should be (I) in “Times Roman”; (II) with “standard” spacing; (III) using printing sizes of 5, 6, 8, 10, 12, 14, 18, 24, 36 and 48 points; (IV) recorded for near as S5, S8 and so on (14). Based on these recommendations one face consists of four lines: N5, N8, N10 and N12;
- Side 4: a dot on a line. The fixation target to assess NPC is a small black dot in the centre of a vertical line.
Sides 1, 2 and 3 are used for measurement of NPA and side 4 is used for NPC.
Square rule (Figure 2)

The square rule which holds the drum is 50 cm long. This distance allows the measurement of NPC and NPA of presbyopes who prefer to read at 40 cm or more. Furthermore, it is also easier to determine the angle of 25 degrees from the eyes by a point at the end of a rule 23.3 cm in length (tan 250×50) held at 90 degrees to the end of the rule (12).
The four sides of the square rule are marked differently as; (I) a centimeter scale in 1 cm increment; (II) a corresponding equivalent dioptric scale; (III) expected age scale and; (IV) scale indicating the positions of normal and abnormal convergence.
Cheek rest
The cheek rest of the RNPR (6 cm in length) is attached to one end of the rule. It is made of plastic and has a V-shaped notch in the center to fit the nose. The cheek rest allows the device to be comfortably placed on the subject’s cheek. The housing of the four-sided cubical drum is designed in such a way that the measurements can be read from the rearmost edge of the slider. The cheek rest results in the RNPR being positioned further from the plane of the eyes. This error in measurement is compensated by projecting the target forward by 6 cm (12).
Measurement procedure for NPC
RNPR measures both the subjective and objective NPC (15). Prerequisite for measuring NPC is the binocularity of a patient and a normal room illumination.
To measure the NPC, the dot on the line is the standard target. The examiner holds the ruler and gently places the cheek rest on the inferior orbital margin. NPC is most accurately measured by the RNPR in the depressed position of 45 degrees (16). The clinician asks the patient to focus on the black dot and slowly moves the towards the patient’s eyes at a constant and linear rate of about 1±2 cm per second (17).
The subjective break point is indicated when the patient either reports diplopia or until the slider is stopped by the cheek rest. The recovery is noted when the patient reports one target when the slide is slowly moved back. The objective values of break and recovery to binocularity are noted when the examiner notices that one or both eyes diverge from fixation and when both eyes regain triangulation on the target, respectively. All readings are measured to the nearest 0.5 cm.
Previous studies suggested that the test for NPC should be repeated to obtain a clinically useful information to diagnose convergence insufficiency, but there exists no agreement between the number of times the test should be repeated. Wick [1987] and Mohindra et al. [1980] recommended that the NPC should be repeated 4 to 5 times, while Scheiman et al. [2003] reported that the test should be repeated 10 times to yield significant clinical information (18-20). NPC should be measured 3 times at the beginning of the assessment and twice at the end to check for fatigue (16). Many patients manifest symptoms only after several minutes of near task.
Merits and demerits
The merits—why RNPR?
The RNPR is considered the method of best practice for measuring accommodation and convergence, and forms protocol for eye testing, especially for the RAF and Civil Aviation Authority (21). Clinicians continue to use RNPR because it is easily available and new instruments are not introduced. Furthermore, because of its reproducibility, it is regularly used by researchers to measure convergence and accommodation (7,12,22,23).
There is also no effect of the proximity of the RNPR on the NPC. The study by Hung et al. [1996] reported that the relative proximal accommodation and proximal convergence induced by the use of RNPR were not clinically significant under simulated natural viewing environment (24). It is likely that these advantages make RNPR a preferred instrument.
The demerits of RNPR
The RNPR is designed such that the cheek rest cannot advance closer than 5.5 cm towards the patient’s face and allows the measurement the near point of convergence only up to 5.5 cm. However, many studies suggest that normative values for NPC are less than what could be measured by RNPR. Maples et al. [2007] demonstrated that to differentiate more and less symptomatic children the NPC break should be 5 cm or less (25). Several authors have assessed NPC between subjects with normal binocular vision and convergence insufficiency and suggested a clinical cutoff value of 5 and 7 cm for the NPC break and NPC recovery, respectively (5,20,26). Furthermore, recent studies have used NPC of six or less as a criterion for the diagnosis of convergence insufficiency (27-29). To overcome the drawback of the RNPR to accurately measure less than 5.5 cm, Paul Adler [2004] came up with a simple and low-cost modification to RNPR while maintaining its advantages (4).
The drum was extended with a Meccano® part on one side and a homemade plastic extension on the other side to bring the target closer than 5 cm.
RNPR is an accommodative target, and it can be less sensitive to evaluate NPC for the diagnosis of convergence insufficiency. The study by Pang et al. [2010] evaluated and compared NPC between an accommodative target (RNPR), a transilluminator (TR), and a TR with a red lens (RL) and found that the mean NPC break (with all targets) was less than 4.5 in the control group. It also showed that TR with a RL had higher sensitivity (100%) and specificity (88.9%) values compared to RNPR and proposed to use RL in suspected cases of convergence insufficiency (5). Thus, the credibility and reliability of RNPR become questionable.
It is assumed that the NPC measurement obtained with the RNPR is accurate. However, a few studies submitted that use of RNPR gives a more remote NPC compared to other methods. Adler et al. [2007] evaluated NPC with five different targets and found that when RNPR and penlight were used the NPC break point was more remote as compared to a pencil tip, fingertip, and N5 letters. They concluded that NPC determined with targets in free space would be more accurate as it correlates with the real world scenario (23). Similarly, Siderov et al. [2001] concluded that in a non-presbyopic population the RNPR gives a more remote NPC as compared to a pencil tip or a fingertip though the author considers it clinically insignificant (17).
The possible reason for receded NPC with RNPR is the pressure of the cheek rest on the face. The touch gives a proprioceptive feedback which might indicate that the target is closer than its actual distance and provides a stimulus to cease convergence and accommodation early, resulting in a more remote NPC (23).
Several studies have reported that the NPC break point would differ from the recovery point (17,20,21). Adler et al. [2007] reported that the average difference between NPC break and recovery is significantly decreased with targets mounted on the RNPR compared to the targets in free space. The relative difference is important in making the diagnosis of convergence insufficiency; the use of the RNPL rule makes it difficult to diagnose the borderline cases of convergence insufficiency (20). Furthermore, it was suggested that in the interpretation of results obtained by RNPR, one should use the NPC norms established using RNPR; similarly for targets used in free space (23).
There are also no recent studies to validate the use of RNPR and the design of the instrument has remained unchanged since its introduction in the mid-1950s. Nevertheless, clinicians still choose to use the RNPR. Though there is no evidence on why clinicians prefer to use RNPR, one possible reason could be the assumption that as long as cheek rest remains in contact with the subject’s face, the measured distances are correct. Moreover, it is expected that if targets are used in free space, the chances of errors are high if the subject or the clinician moves or is not steady. Another possible reason could be that most of the clinicians are not aware of the drawbacks of the RNPR.
Conclusions
NPC is the prime finding in the diagnosis of convergence insufficiency and RNPR is the traditionally employed instrument for the measurement is the NPC. Though the RNPR has a few advantages; there is no enough evidence to validate its use. More recent studies have highlighted the demerits of RNPR and favoured other methods of NPC measurement. There is a need to reassess and modify the design of RNPR to overcome its drawbacks and make RNPR more effective. In the meantime, it is recommended that clinicians and researchers consider the merits and demerits and follow the norms established with RNPR itself while measuring NPC with the RNPR.
Acknowledgments
The author would like to thank Prof. Monica Chaudhry and Associate Prof. Gaurav Bhardwaj of Amity University Haryana, India for the guidance and support for the conduct of this review.
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.02.05). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hashemi H, Nabovati P, Yekta AA, et al. Amplitude of accommodation in an 11- to 17-year-old Iranian population. Clin Exp Optom 2017;100:162-6. [Crossref] [PubMed]
- Abraham LM, Kuriakose T, Sivanandam V, et al. Amplitude of accommodation and its relation to refractive errors. Indian J Ophthalmol 2005;53:105-8. [Crossref] [PubMed]
- Adler P. Efficacy of treatment for convergence insufficiency using vision therapy. Ophthalmic Physiol Opt 2002;22:565-71. [Crossref] [PubMed]
- Adler P. RAF Near Point Rule modification. Ophthalmic Physiol Opt 2004;24:469-70. [Crossref] [PubMed]
- Pang Y, Gabriel H, Frantz KA, et al. A prospective study of different test targets for the near point of convergence. Ophthalmic Physiol Opt 2010;30:298-303. [Crossref] [PubMed]
- Rouse MW, Borsting E, Hyman L, et al. Frequency of convergence insufficiency among fifth and sixth graders. The Convergence Insufficiency and Reading Study (CIRS) group. Optom Vis Sci 1999;76:643-9. [Crossref] [PubMed]
- Westman M, Liinamaa MJ. Relief of asthenopic symptoms with orthoptic exercises in convergence insufficiency is achieved in both adults and children. J Optom 2012;5:62-7. [Crossref]
- Convergence Insufficiency Treatment Trial (CITT) Study Group. The convergence insufficiency treatment trial: design, methods, and baseline data. Ophthalmic Epidemiol 2008;15:24-36. [Crossref] [PubMed]
- Cooper J, Jamal N. Convergence insufficiency-a major review. Optometry 2012;83:137-58. [PubMed]
- Bade A, Boas M, Gallaway M, et al. Relationship between clinical signs and symptoms of convergence insufficiency. Optom Vis Sci 2013;90:988-95. [Crossref] [PubMed]
- Rouse MW, Hyman L, Hussein M. CIRS Group. How do you make the diagnosis of convergence insufficiency?: Survey Results. J Optom Vis Devel 1997;28:91-7.
- Neely JC. The R.A.F. near-point rule. Br J Ophthalmol 1956;40:636-7. [Crossref] [PubMed]
- Catford GV. Amblyopia: a comparison between distance and near vision. Br J Ophthalmol 1956;40:633-5. [Crossref] [PubMed]
- Law FW. Standardization of reading types. Br J Ophthalmol 1951;35:765-73. [Crossref] [PubMed]
- Scheiman M, Wick B. Clinical Management of Binocular Vision: Heterophoric, Accommodative and Eye Movement Disorders. 2nd ed. Philadelphia: Lippincott, Williams and Wilkins, 2002:13.
- Jones L, Eperjesi F, Evans B. Binocular vision evaluation in practice. Optom Today 1999;39:33-6.
- Siderov J, Chiu SC, Waugh SJ. Differences in the nearpoint of convergence with target type. Ophthalmic Physiol Opt 2001;21:356-60. [Crossref] [PubMed]
- Wick BC. Horizontal deviations. In: Amos J. editor. Diagnosis and management in Vision care. Boston: Butterworth-Heineman, 1987:473.
- Mohindra I, Molinari J. Convergence insufficiency: its diagnosis and management--part 1. Opt Mon 1980;71:38-43.
- Scheiman M, Gallaway M, Frantz KA, et al. Nearpoint of convergence: test procedure, target selection, and normative data. Optom Vis Sci 2003;80:214-25. [Crossref] [PubMed]
- Jiménez R, Pérez MA, García JA, et al. Statistical normal values of visual parameters that characterize binocular function in children. Ophthalmic Physiol Opt 2004;24:528-42. [Crossref] [PubMed]
- Parkinson J, Linthorne N, Matchett T. Subjective measurement of the near point of accommodation in pre/early literates. Am Orthopt J 2001;51:75-83. [Crossref] [PubMed]
- Adler PM, Cregg M, Viollier AJ, et al. Influence of target type and RAF rule on the measurement of near point of convergence. Ophthalmic Physiol Opt 2007;27:22-30. [Crossref] [PubMed]
- Hung GK, Ciuffreda KJ, Rosenfield M. Proximal contribution to a linear static model of accommodation and vergence. Ophthalmic Physiol Opt 1996;16:31-41. [Crossref] [PubMed]
- Maples WC, Hoenes R. Near point of convergence norms measured in elementary school children. Optom Vis Sci 2007;84:224-8. [Crossref] [PubMed]
- Hayes GJ, Cohen BE, Rouse MW, et al. Normative values for the nearpoint of convergence of elementary schoolchildren. Optom Vis Sci 1998;75:506-12. [Crossref] [PubMed]
- Bade A, Boas M, Gallaway M, et al. Relationship between clinical signs and symptoms of convergence insufficiency. Optom Vis Sci 2013;90:988-95. [Crossref] [PubMed]
- Scheiman M, Rouse M, Kulp MT, et al. Treatment of convergence insufficiency in childhood: a current perspective. Optom Vis Sci 2009;86:420-8. [Crossref] [PubMed]
- CITT-ART Investigator Group. Convergence Insufficiency Treatment Trialz - Attention and Reading Trial (CITT-ART): Design and Methods. Vis Dev Rehabil 2015;1:214-28. [PubMed]
Cite this article as: Sharma IP. RAF near point rule for near point of convergence—a short review. Ann Eye Sci 2017;2:16.


