
Conjunctival flap cover surgery: 10-year review
Introduction
Conjunctival flaps, which have been successfully used for over 100 years, are an received treatment modality for challenging disorders of the ocular surface. However, the indications for performing conjunctival flap cover surgery have reduced over the years. This may be primarily due to alternative and more effective methods of managing serious disorders of the ocular surface. The utilization of more potent antimicrobials, tissue adhesives, soft bandage contact lenses, better ocular lubrication systems, immunosuppressive agents, and other corneal, conjunctival, and oculoplastic surgical procedures have made the need for conjunctival flaps infrequent (1). The conjunctival flap, however, remains a useful therapeutic option in the selected cases (2). In this study, we review the indications, symptoms and complications of conjunctival flap cover surgery, to evaluate this technique for the treatment of ocular surface disorders.
Methods
In this retrospective noncomparative interventional case series review study, 253 eyes of 253 consecutive patients, who underwent conjunctival flap cover surgery at The Joint international eye center of Shantou University and The Chinese University of Hong Kong from January 2010 to December 2015, were included. Institutional Ethics Committee approval was obtained [Ethic Approval ID: EC 20160616(Jeny4)-A10], and the study was conducted in accordance of the guide-lines of the Declaration of Helsinki and the Health Insurance Portability and Accountability Act of 1996. Inclusion criteria include patients who underwent conjunctival flap cover surgery for any reason. Exclusion criteria include patients who received conjunctival flap for ordinary pterygium, or who performed conjunctival flap cover surgery failed to complete at least 6-month follow-up. The surgical indications are divided into therapeutic, aesthetic, tectonic, and analgesic according to the cause and the purpose of treatment. The therapeutic indications include unresponsive ulcerative infectious keratitis, severe chemical injury, persistent corneal epithelial defect, corneal limbal disease, and so on. The aesthetic indications are primarily ocular surface preparation for a cosmetic scleral shell. The tectonic indications are mainly corneal perforation, glaucoma surgery complications, or corneal and scleral melting. The analgesic indications are primarily bullous keratopathy with poor vision prognosis. It was defined as satisfactory anatomic and functional results when local corneal infection, dissolution and perforation of the eye are under control, and eyeball are preserved in the last visit. It was defined as a satisfactory symptom of the results if pain, foreign body sensation, photophobia, tears and other symptoms disappeared. Detailed indications, symptoms and complications information was available in all cases.
Surgical procedure
All procedures are performed under local retrobulbar or infiltration anesthesia, and general anesthesia is reserved for children and uncooperative adults. Specific surgical procedures reported previously of total conjunctival flap, bipedicle bridge flap, single pedicle flap and advancement flap (1), which were selected in accordance with the needs of patients.
Results
A total of 253 eyes of 253 patients were operated on using this technique. The ages and genders of the patients preoperative are shown in Table 1.
Table 1
| Variables | Number |
|---|---|
| Age (years) | 48.97±19.10 [7–87] |
| Gender (%) | |
| Male | 176 (69.6) |
| Female | 77 (30.4) |
In all of these cases, satisfactory anatomic and functional outcomes were achieved. The BCVA of 224 eyes out of 253 patients were no worse than that of preoperative, and it accounts for 88.5%. The BCVA of 29 eyes out of 253 patients (11.5%) decreased postoperatively.
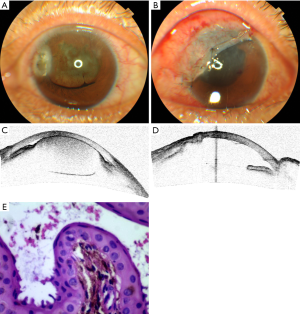
The surgical indications for conjunctival flap cover surgery are shown in Table 2. The primary surgical indications is therapeutic (Figure 1). As it was shown in the table that 138 eyes out of 253 patients are therapeutic, and it accounts for 54.5%. The main diagnose of therapeutic indication is refractory corneal ulcer for 135 eyes out of 253 patients (53.4%), and the diagnosis of the second therapeutic indication is corneoscleral dissolution induced by chemical injury for 3 eyes out of 253 patients. The second surgical indications is aesthetic for 63 eyes out of 253 patients (24.9%). The main diagnose of aesthetic indications is atrophy of eyeball for 45 eyes out of 253 patients (17.8%) and corneal leukoma for 18 eyes out of 253 patients (7.1%). The third surgical indications is tectonic for 45 eyes out of 253 patients (17.8%). The main diagnose of tectonic indications is corneal perforation with corneal ulcer for 41 eyes out of 253 patients (Figure 2). There is one case of postoperative pterygium excision, iris cyst, scleral ulcer, and necrotizing scleritis (Figure 3) in the tectonic indications, respectively. The last surgical indications is analgesic. Seven eyes out of 253 patients are analgesic indications, and it accounts for 2.8%.
Table 2
| Indications | Number | Percentage (%) |
|---|---|---|
| Therapeutic | 138 | 54.5 |
| Refractory corneal ulcer | 135 | |
| Fungal | 64 | |
| Bacterial | 38 | |
| Herpes simplex keratitis | 21 | |
| Others | 12 | |
| Chemical injury | 3 | |
| Tectonic | 45 | 17.8 |
| Corneal perforation | 43 | |
| Corneal ulcer | 41 | |
| Postoperative Pterygium excision | 1 | |
| Iris cyst | 1 | |
| Scleral ulcer | 1 | |
| Necrotizing scleritis | 1 | |
| Aesthetic | 63 | 24.9 |
| Atrophy of eyeball | 45 | |
| Corneal leukoma | 18 | |
| Analgesic | 7 | 2.8 |
| Bullous keratopathy, Absolute glaucoma | 7 |


All the operations were completed without any complications except 8 cases buttonhole formation intraoperatively (Table 3). They all obtain satisfactory results after simple suture. Three eyes out of 253 patients (1.2%) presented conjunctival flaps dissolving and corneal perforation postoperative conjunctival flap cover surgery. They had to receive corneal transplantation to avoid enucleation. Four eyes out of 253 patients (1.6%) presented cystic flap and two of them received surgical excision.
Table 3
| Variables | Complications | Treatment |
|---|---|---|
| Intraoperative | Buttonhole formation [8] | Suture [8] |
| Postoperative | Conjunctival flaps dissolving and corneal perforation [3] | Corneal transplantation [3] |
| Cystic flap [4] | Surgical excision [2] | |
| Retraction of the flap [12] | None |
Discussion
The primary option for the management of an ocular surface disorder is usually conventional medical or surgical therapy. Conjunctival flap surgery, which can provide metabolism and mechanical support for cornea healing and hence restore the integrity of the damaged eye surface, is reserved for those who failed to ordinary treatments (1).
The main indications of therapeutic conjunctival flap cover surgery include unresponsive ulcerative infectious keratitis, persistent corneal epithelial defect, and corneal limbal disease. The conventional treatment for acute microbial keratitis is local eye drops. However, conjunctival flap may be useful in either unresponsive bacterial (3,4), fungal keratitis (5), Herpes simplex virus Keratitis (6), or acanthamoeba keratitis (7,8) in which damage to the epithelial basement membrane and underlying stroma prevents surface healing. In our study, 135 eyes in 253 patients were diagnosed acute microbial keratitis and account for 53.4%. In this primary indication, 64 eyes were diagnosed of mycotic keratitis,38 eyes were diagnosed of bacterial keratitis, 21 eyes were diagnosed of Herpes simplex keratitis. The diagnose of remain 12 eyes were mixed keratitis. Many unresponsive ulcerative infectious keratitis cannot be treated with corneal transplantation because of the lack of corneal donor material in China (9,10). Conjunctival flap cover surgery may be able to shorten the course, alleviate pain, and reduce the incidence of corneal perforation, is sometimes the reserved way to save the eyeball (1). This may be the reasons why therapeutic conjunctival flap procedure account for the largest proportion in our study. However, Conjunctival flap may undermine the vision significantly in cases where the flap covers the visual axis (1). It gives grounds that why the BCVA of 29 eyes out of 253 patients (11.5%) decreased postoperatively. Fortunately, this procedure can be reversed and an optical keratoplasty surgery can be performed at a later date.
The main indications of aesthetic conjunctival flap cover surgery are ocular surface preparation for a cosmetic scleral shell. Patients, with no useful vision or a blind disfigured eye under the condition of phthisis bulbi or microphthalmia, may need a cosmetic scleral shell (11). A conjunctival flap provides a regular surface and eradicates significant irritation caused by the sensitive cornea, and therefore make it easy to coordinate the prosthesis (1). In addition, conjunctival flap has other advantages such as good cosmetic appearance, relieved pain, and no need to invasive surgery or enucleation (11). The indications include atrophy of eyeball for 45 eyes out of 253 patients (17.8%) and corneal leukoma with no useful vision for 18 eyes out of 253 patients (7.1%) in our study. The total amount for aesthetic was 63 out of 253 patients (24.9%) which was similar to the report of Boidin (12).
The main indications of tectonic conjunctival flap cover surgery include corneal and scleral melting, corneal perforation (13), and glaucoma surgery complications (14,15).
Thin conjunctival flaps, with only a weak layer of conjunctiva covers the ulcer, are not suitable for active suppurative processes with impending corneal perforations or perforated corneas in eyes with good visual potential (1). However, thick pedunculated conjunctival flap with adherent Tenon’s capsule may be able to provide stronger mechanical support for the cornea. It may be appropriate for impending perforations or perforated cornea when donor corneal material is not available. This technique ensures the closure of perforations and prevents leakage from the anterior chamber (16). However, when it comes to cases with bigger corneal perforation, scleral ulcer or necrotizing scleritis, advancement flap may be more appropriate. The surgical indications for tectonic were 45 out of 253 patients (17.8%) in our study, in which include forty-three corneal perforations, one case of scleral ulcer and necrotizing scleritis respectively.
The main indications of analgesic conjunctival flap cover surgery are bullous keratopathy. As we all knows that the first and most important option for bullous keratopathy is DSAEK (17,18) and DMEK (19) nowadays. Conjunctival flap cover surgery is an alternative for those with poor potential useful vision (20).
Conjunctival flaps dissolving and corneal perforation are rarely, however, very serious complication after conjunctival flap cover surgery. There were 3 eyes out of 253 patients (1.2%) presented conjunctival flaps dissolving and corneal perforation 2–4 weeks after surgery. Corneal transplantation is often needed to avoid enucleation under this condition. Fortunately, No enucleation was performed in all those three eyes and they achieved satisfactory clinical results after secondary corneal transplantation. There were 4 out of 253 patients (1.6%) assumed cystic flap. Two of them become large enough and received surgical excision. No other complications require surgical treatment presented. In addition, Postoperative Sympathetic ophthalmia, even rare, should be noticed (21).
In conclusion, we present our 10-year experiences of indications and complications of conjunctival flap cover surgery. Its primary indication is refractory corneal ulcer and corneal perforation, and the second indication is aesthetic with poor visual potential coexisting ocular surface diseases. We believe that this underused technique represents an interesting alternative to more mutilating surgeries.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.05.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All patients provided informed consent, and this study adhered to the tenets of the Declaration of Helsinki (as revised in 2013) [Ethic Approval ID: EC 20160616(4)-A10].
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vieira AC, Mannis MJ. Conjunctival Flaps. In: Krachmer JH, Mannis MH, Holland EJ. editors. Cornca. 4th edition. St. Louis: Elsevier; 2016;142:1573-80.
- Lim LS, How AC, Ang LP, et al. Gundersen flaps in the management of ocular surface disease in an Asian population. Cornea 2009;28:747-51. [Crossref] [PubMed]
- Jang SY, Yoon JS. Treatment of refractory exposure keratitis with modified medial tarsorrhaphy using tarsoconjunctival flap. Graefes Arch Clin Exp Ophthalmol 2013;251:1369-72. [Crossref] [PubMed]
- Abdulhalim BE, Wagih MM, Gad AA, et al. Amniotic membrane graft to conjunctival flap in treatment of non-viral resistant infectious keratitis: a randomised clinical study. Br J Ophthalmol 2015;99:59-63. [Crossref] [PubMed]
- Sun GH, Li SX, Gao H, et al. Clinical observation of removal of the necrotic corneal tissue combined with conjunctival flap covering surgery under the guidance of the AS-OCT in treatment of fungal keratitis. Int J Ophthalmol 2012;5:88-91. [PubMed]
- Gao H, Jia Y, Li S, et al. Conjunctival flap covering combined with antiviral and steroid therapy for severe herpes simplex virus necrotizing stromal keratitis. Scientific World Journal 2015;2015:565964
- Cremona G, Carrasco MA, Tytiun A, et al. Treatment of advanced acanthamoeba keratitis with deep lamellar keratectomy and conjunctival flap. Cornea 2002;21:705-8. [Crossref] [PubMed]
- Mauger TF, Craig E. Combined acanthamoeba and Stenotrophomonas maltophilia keratitis treated with a conjunctival flap followed by penetrating keratoplasty. Cornea 2006;25:631-3. [Crossref] [PubMed]
- Zhang Z, Niu G, Choi JS, et al. Bioengineered multilayered human corneas from discarded human corneal tissue. Biomed Mater 2015;10:035012 [Crossref] [PubMed]
- Pan ZQ, Liang QF. Pay attention to the donor material supply for corneal transplantation. Zhonghua Yan Ke Za Zhi 2016;52:641-3. [PubMed]
- Ding J, Chen T, Hou Z, et al. Cosmetic shell fitting over a sensitive cornea in mild phthisis bulbi using total conjunctival flap. Aesthetic Plast Surg 2013;37:398-401. [Crossref] [PubMed]
- Boidin H, Gueudry J, Portmann A, et al. Conjunctival flap: Still a relevant procedure. J Fr Ophtalmol 2012;35:170-5. [Crossref] [PubMed]
- Kim MH, Chung SH, Kim HS, et al. The Use of Conjunctival Pedicle Flaps to Prevent Corneal Perforation in Graft-Versus-Host Disease. Semin Ophthalmol 2016; [Epub ahead of print]. [Crossref] [PubMed]
- Grover DS, Merritt J, Godfrey DG, et al. Forniceal conjunctival pedicle flap for the treatment of complex glaucoma drainage device tube erosion. JAMA Ophthalmol 2013;131:662-6. [Crossref] [PubMed]
- Medel R, Hristodulopulos V, Mazzarella S, et al. Upper eyelid tarsoconjunctival flap for the treatment of Ahmed valve plate exposure. J Glaucoma 2014;23:579-81. [Crossref] [PubMed]
- Sandinha T, Zaher SS, Roberts F, et al. Superior forniceal conjunctival advancement pedicles (SFCAP) in the management of acute and impending corneal perforations. Eye (Lond) 2006;20:84-9. [Crossref] [PubMed]
- Javadi MA, Feizi S, Jafari R, et al. Descemet Stripping Automated Endothelial Keratoplasty in Fuchs' Endothelial Dystrophy versus Pseudophakic Bullous Keratopathy. J Ophthalmic Vis Res 2016;11:372-8. [Crossref] [PubMed]
- Kim SE, Lim SA, Byun YS, et al. Comparison of Long-term Clinical Outcomes between Descemet's Stripping Automated Endothelial Keratoplasty and Penetrating Keratoplasty in Patients with Bullous Keratopathy. Korean J Ophthalmol 2016;30:443-50. [Crossref] [PubMed]
- Bhandari V, Reddy JK, Chougale P. Descemet's Membrane Endothelial Keratoplasty in South Asian Population. J Ophthalmic Vis Res 2016;11:368-71. [Crossref] [PubMed]
- Güell JL, Morral M, Gris O, et al. Treatment of symptomatic bullous keratopathy with poor visual prognosis using a modified Gundersen conjunctival flap and amniotic membrane. Ophthalmic Surg Lasers Imaging 2012;43:508-12. [Crossref] [PubMed]
- Tripathy K, Mittal K, Chawla R. Sympathetic ophthalmia following a conjunctival flap procedure for corneal perforation. BMJ Case Rep 2016;2016:bcr2016214344
Cite this article as: Yao Y, Jhanji V. Conjunctival flap cover surgery: 10-year review. Ann Eye Sci 2017;2:25.


