
Continuing professional development: progress beyond continuing medical education
Introduction
Continuing medical education (CME) (1), is rapidly evolving into competency-based continuing professional development (CPD) (2,3). This has been driven by many factors including rapid change in medical knowledge (4) and education of medical practitioners (5) along with changes in patients and society, healthcare systems, regulators and the political environment (2,3). In many jurisdictions, performing CPD is now an important component of maintenance of medical licensure (6,7). This narrative review provides clarification on changes in CME, describes CPD programs and systems, overviews the authors’ experiences as CPD educators and highlights ongoing challenges in CPD in the healthcare professions, focusing on ophthalmology. Reflecting progress in the field we have chosen to use the term CPD throughout.
Life long learning: a professional culture
Life-long learning (LLL) consists of continuous training over the course of a professional career (8) and occurs over the continuum of competencies required for medical education (9). Good practices of CPD emphasize that LLL is a duty and an ethical obligation of the medical profession (10,11). LLL is implied when physicians take the Hippocratic oath as a vowing demonstration that they should be primarily responsible for being self-directed lifelong learners, take personal responsibility for developing their learning goals and applying the best available evidence to address clinical questions.
The physician’s motivation to engage in LLL is thought to derive from three main needs:
- To provide the best care for the individual patient;
- To honor the demands from employers and society;
- To attain and maintain job satisfaction (12).
Lack of time, insufficient compensation and poor system support may hinder professional engagement in LLL. Health care organizations and CPD educators need to nurture a culture whereby health professionals feel encouraged to further their learning (13).
Evolution of continuing medical education of healthcare professionals
CME is evolving to CPD and more recently competency-based CPD. The terms CME and CPD are closely associated and frequently used interchangeably. Table 1 compares and contrasts the forms of on-going education.
Table 1
| Characteristics | Continuing medical education | Continuing professional development | Competency-based continuing professional development |
|---|---|---|---|
| Drivers | Teacher | Self-directed | Self-directed; needs of health-care system |
| Focus | Clinical expertise | All competencies required by medical practitioner | Performance of medical practitioner in clinical practice |
| Curriculum | No | Yes | Yes |
| Delivery | Formal lectures in auditoria | Wide-range of learning methods, including on-line and informal, unplanned learning | Wide-range of learning methods, including on-line and informal, unplanned learning. Includes audit of performance in practice |
| Outcome | Improved patient care | Improved patient outcomes | Improved patient outcomes; meets needs health-care system |
| Comment | Decontextualized, fragmented | Self-assessment and reflection are assumed | Performance in practice is measured objectively |
CME may be defined as educational activities aiming to maintain and expand the knowledge, skills and professional performance required for a physician to serve patients, the public and the profession (1). CME is classically characterized by being teacher-driven and primarily lecture-based in order to deliver topics as chosen by the teacher with no necessary reference to individual learning needs, curriculum or patient outcomes. Nevertheless the contribution of effectively applied classical CME as a didactic, formal educational methodology to drive practice change should not be disregarded and is an interesting research field (14).
CPD may be defined as the process whereby physicians maintain and improve standards of medical practice through the development of knowledge, skills, attitudes and behavior (1). Worldwide, CPD has evolved from CME (15-17) and differs in a number of ways (Table 1). CPD recognizes competencies other than medical expertise as required to practice high quality medicine. In the Royal College of Physicians and Surgeons of Canada competency framework, the CanMEDS model includes leadership, communication, professionalism, collaboration, scholarship and advocacy (18). CPD acknowledges that learning can occur using multiple modalities, from which the interactive ones have been demonstrated as more effective (19-22). It may occur in an informal setting, which can be unrecognized in a system based solely on lectures (23). CPD is ultimately self-directed and relies on the physician’s learning needs self-assessment to tailor education to personal and organizational needs (24). This implies a reflective component, which despite its intrinsic value and recommendation to develop has been deemed as a significant limitation of CPD due to recognized difficulties in physician self-assessment (25-29).
As a further evolution from CPD, competency-based CPD is viewed as a dynamic process allowing lifelong development of competence. It is founded on clear, effective and measurable competencies necessary to practice high quality medicine (30). This implies the need for external assessment of patient outcomes, commonly by clinical audit (31).
Elements of a CPD program and system
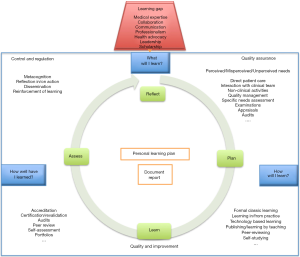
A CPD program can be viewed from the perspective of the individual participant, but also from the perspective of CPD educators, providers and regulators (Figure 1).

Individual participant
CPD begins with developing a personal learning plan (PLP) (32-35). The PLP prompts a cycle of reflection, planned learning, undertaking activities and evaluation of learning known as the CPD cycle (36). The PLP allows each professional to tailor CPD activities (content, instructional design and setting) to their personal learning style, meet the identified learning need and apply the appropriate solution while meeting career objectives and ambitions. Recent participatory research following a modified Delphi method based on several CPD stakeholders’ perspective (patients, education, scientific and society) confirmed the relevance of the individual needs analysis (37).
Elements of an individual CPD program are shown in Figure 2. A learning gap may be identified by reflection on clinical care activities, formal self-assessment or regulatory body examination. This triggers the foundational sequence of PLP professional questions: (I) What will I learn? (II) How will I learn? (III) How well have I learned? These activate the corresponding cyclic CPD actions: reflect, plan, learn and assess. Quality assurance, quality improvement, control and regulation are three critical elements of a CPD program. Accreditation of learning activities and re-licensure are highly related to producing effective CPD and may be undertaken by individual or combined regulatory authorities.
Clinical audit is one method to assess patient outcomes and review processes. An audit is a five-step cyclic process: (I) identify the problem; (II) set criteria and standards to establish the acceptable level of performance; (III) collect data through direct observation, peer-review, questionnaires, etc.; (IV) compare practice with the set standards, report if those were met, otherwise explain why not; and (V) implement changes. The process continues with measurement of changes and re-audit if necessary (32,39).
Portfolios are useful tools to record and demonstrate CPD activities and review the physician’s practice. Online or hard copy portfolios stimulate reflection on and in practice (40-42).
Effectiveness of CPD programs may be assessed using the classical descriptive Miller’s pyramid, Moore’s Outcome-based CME Evaluation Model and the Accreditation Council for Continuing Medical Education framework (43-45). Although not the topic of this review, there is extensive literature confirming that undertaking CPD (22,23,46-48) and clinical audit (49) improves physicians’ performance and patient outcomes.
CPD educators
CPD can be considered part of the medical education continuum (9) and thus medical educators should be involved in CPD systems and curriculum design, teaching and outcomes assessment (50).
CPD as a discipline is evolving along with other aspects of the medical education continuum. Swanwick identified three trends driving development of postgraduate medical educators: professionalization of medical education, increasing accountability and the pursuit of educational excellence, all of which are evident in CPD (51). The medical education movement towards competency-based education is clearly important for developing skills during professional practice but has been incompletely studied in the CPD setting (31).
CPD systems and providers
CPD systems are the framework to guide individuals undertaking personally directed CPD. Ideally CPD systems are designed by CPD educators and implemented by CPD providers, which should include professional societies (e.g., ICO, RANZCO, American Academy of Ophthalmology).
Increasing mobility of the healthcare workforce in a globalized world will be facilitated by mutual agreements regarding professionals’ qualifications and CPD systems (6,52). International standards encourage CPD participants to self-assessment, help providers to design and offer effective learning interventions, and support regulators.
Societies and Colleges should engage in developing structured systems to
- Facilitate overburdened physicians recording their personal learning activities and demonstrate CPD progression;
- Act as an interface and bridge all stakeholders;
- Inform clear guidelines and good practice standards within the medical profession;
- Provide templates and forms for submitting learning interventions to validate;
- Align CPD content, delivery format and outcomes assessment;
- Develop inter-professional education and teambuilding educational strategies;
- Embrace information technologies to enable timely learning opportunities stretching from the classroom to the point of care;
- Manage profession regulation aligned with improvement in patient safety and improvement in public health;
- Define program financing;
- Develop a scientific basis for CPD practice.
CPD and medical regulators
There is considerable worldwide variation regarding the process of regulating the maintenance of medical license to practice. Although foundational good practices are generally accepted, systems vary in detail or prescriptive criteria and corresponding consequences, with most of them relying on professional self-regulation. While in some jurisdictions there are no requirements, others request the demonstration of undertaken CME activities as credit units based on spent learning time. There is however a trend for demonstrating CPD progress supported on patient outcomes and improvement in public health as necessary for on-going medical licensure, known as revalidation, recertification or maintenance of certification (MOC) (6,7). Conversely, poor CPD performance has been associated with dyscompetence and investigation by medical regulators (53).
Factors driving change in continuing medical education
Several components concerning medical knowledge, medical practitioners, patients and society, healthcare systems, regulation processes and requirements and the political environment account for the ongoing change in continuing professional education (Table 2).
Table 2
| Factor driving change | Components |
|---|---|
| Medical knowledge | Rapid growth ( |
| Rapid redundancy ( |
|
| Evidence-based medicine | |
| Medical practitioners | Need to demonstrate competency to patients |
| Medico-legal consequences of changes in medical knowledge | |
| Increased global mobility | |
| Patients and society | Demographic changes |
| Increase in chronic disease | |
| Increased global mobility | |
| Increased expectations for doctor accountability | |
| Healthcare systems | Increasingly complex ( |
| Funding constraints | |
| Inter-professional team work ( |
|
| Regulators | CPD requirement for revalidation |
| Patient outcome analysis requirement for revalidation | |
| Political environment | Increased international recognition of professional qualifications (EU directive) |
The recently updated European Union directive on the recognition of professional qualifications represents a significant political endeavor to reach a mutual agreement in educational activities validation and healthcare qualifications. The document contains clauses regarding CPD for the healthcare workforce with the purpose to improve quality and maintain patient safety among the European Union (EU) countries (57).
Industry became a major source of research and funding after World War II. A study showed that 94% of U.S. physicians had a relationship with industry and from those 60% were involved in medical education and 40% in elaborating clinical practice guidelines. Given the significant industry sponsorship of CPD, disclosure of financial relationships between physicians and industry became critical. The Sunshine Act is a program created to balance data transparency against eventual effects on CME innovation. The program aims to manage potential conflicts of interest without affecting a constructive collaboration with industry (58,59).
Report of authors’ experiences
As CPD educators and bearing in mind the special needs of low-resource countries we focused on creating the “ICO Guide for Effective CPD/CME” (38), and in developing a CPD program in Cambodia following the twinning model (60).
The additional challenges of CPD in low resource settings and difficult circumstances, the geographically remote regions, the worldwide variety of CPD programs and systems and the increasing need to hold a holistic perspective of CPD were among the major reasons for the members of the International Council of Ophthalmology (ICO) Committee for CPD and their invitees to create the “ICO Guide to Effective CPD/CME”. They wrote collaboratively a collection of problem-based design manuscripts to guide to foundational concepts and relevant questions regarding CPD/CME. The manuscripts were organized into five sections reflecting the variety of perspectives of CPD stakeholders, who were grouped into four categories: Participant, Educator, Provider and Regulator. A Glossary and a “Forward & Perspectives” section with comments from ICO leaders and other individuals with interest in CPD were added. Some planned redundancy prevents the need for sequential reading of the collection of evidence based, stand-alone chapters, each holding a learning event. Hyperlinked words or phrases direct the reader to more detailed reading in other chapters. After proof reading, edition, and revision by external reviewers the e-book was formatted to be available online and downloaded for free. As a living document, it will welcome updating of existing manuscripts, future additions and feedback of how users utilize it in practice (38).
A CPD program for Cambodian ophthalmologists was established by partnering (twinning) between RANZCO and the Cambodian Ophthalmological Society (COS) (60). A conjoint committee comprising four ophthalmologists from RANZCO and three ophthalmologists from COS was established, supported by a RANZCO administrative team experienced in CPD administration. CPD requirements and recording were adapted from the RANZCO CPD framework. At the end of the 3-year program, at handover to COS a CPD program and online recording system had been established. All 47 (100%) practicing ophthalmologists in Cambodia were registered for CPD and 21/47 (45%) were actively participating in the COS CPD program on-line recording.
Participants were surveyed for attitudes towards CPD before program development and after handover to COS. They were asked to use a Likert scale to rate statements such as “I support the development of a CPD program for Cambodian ophthalmologists” (Question 1) and “I am happy for the Cambodian Ophthalmological Society to keep records about my CPD activities” (Question 2). Responses demonstrated no statistically significant change. For example for Question 1 the proportion “agreeing” or “strongly agreeing” increased from 96.3% [2013] to 96.9% [2016], The reasons for no detected attitude change towards CPD might include a low response rate, biased responses (determined by participants uninterested in CPD and not responding), survey poor question wording eliciting expected rather than genuine responses and lack of cultural acceptance of the importance of participating in CPD.
Challenges in CPD
From our experiences we note the following challenges in CPD:
- Identification of the most consistent CPD tools to demonstrate outcomes for physicians and professional accountability to society;
- Worldwide constrained human, financial and didactic resources;
- Teaching material not available in participant’s first language;
- Poor compliance with best CPD practices;
- Diversity in remediating, sanctioning and praising modes;
- A proper definition of commercial sponsorship and biased education might still be absent in some systems;
- Compulsory systems, sometimes associated with re-licensure, are expensive and have not yet been proven as associated to better healthcare outcomes;
- Assessment of CPD cost-effectiveness;
- Assessment of the cost-effectiveness of formal CPD accreditation systems;
- Lack of a clear role-definition and coordination of all CPD stakeholders.
We emphasize two approaches as potentially effective solutions for the challenges in CPD. These would include the recognition of
- The relevance of CPD by medical educators and medical regulators, particularly those in leadership positions. These key opinion leaders can effectively lead the cultural change necessary for CPD to take its place in the medical education continuum rather than being an optional activity after graduation from medical training;
- The CPD costs as part of the medical services provision budget, so that both medical services purchasers and providers are able to fully resource CPD activities and systems in a transparent manner.
With adequate recognition and resourcing, CPD providers will be better placed to improve the quality of educational activities and fund research in CPD that will underpin its ongoing quality improvement with a clear public health impact.
Our recommendations for future research are as follows:
- Researchers should adopt a common framework focused on the educational theory underneath CPD and its clinical application (50);
- Assessing CPD systems and their impact on health professionals’ performance is essential to find guidance for investing in CPD. Evaluating outcomes’ higher levels should be seamless and the data used to enhance quality and evidence-based CPD (61);
- Enhancing the profession of CPD by developing CPD providers and educators skilled in needs assessment, instructional design and program evaluation is critical.
Conclusions
Professional, social, political and economic context is driving CPD to structured, regulated mandatory systems. Mandatory or voluntary, CPD systems should be flexible and focused on lifelong learning as a primary duty and an ethical obligation of the medical profession.
If effectively applied, formal, didactic CME lectures may be a component of best practice CPD systems. Content other than medical expertise and modalities including informal, social, web based learning activities are considered valid in effective CPD. CPD has been evolving to competency-based CPD. This is anchored on a framework of clear, effective and measurable competencies and places increased emphasis on aligning healthcare quality improvement with physicians’ practice change, life long learning, assessment and educational strategies.
CPD systems should be built on the PLP, comprise several relevant components, promote innovative educational strategies at the professional and organizational levels and build upon robust research for self-regulation and effectiveness.
Despite the worldwide diversity to conduct CPD, the increasing globalized mobility of patients and healthcare professionals is leading to the need of some mutual agreement among professional organizations and harmonization of CPD best practice. CPD development in low resource regions represents an additional challenge though a significant rewarding value to pursue.
Structured CPD systems should facilitate health professionals to meet the system’s requirements, provide an interaction interface for all stakeholders and enable the development of effective educational programs built upon CPD research.
Effective CPD systems should ensure that healthcare professionals are prepared to provide patient centered care, work effectively in inter professional teams, use evidence-based medicine and health information technologies to timely access educational resources, gather and analyze patient data to make informed decisions and apply quality improvement resources.
Acknowledgments
The authors thank the International Council of Ophthalmology.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Karl C. Golnik, Dan Liang and Danying Zheng) for the series “Medical Education for Ophthalmology Training” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.04.01). The series “Medical Education for Ophthalmology Training” was commissioned by the editorial office without any funding or sponsorship. KCG served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Union Européene des Médecins Spécialistes [Internet]. Brussels: the Society; c2013 [cited 2017 Jan 17]. What is CME. Available online: http://www.uems.eu/general/glossary
- Balmer JT. The transformation of continuing medical education (CME) in the United States. Adv Med Educ Pract 2013;4:171-82. [Crossref] [PubMed]
- Moja L, Kwag KH. Point of care information services: a platform for self-directed continuing medical education for front line decision makers. Postgrad Med J 2015;91:83-91. [Crossref] [PubMed]
- Larsen PO, von Ins M. The rate of growth in scientific publication and the decline in coverage provided by Science Citation Index. Scientometrics 2010;84:575-603. [Crossref] [PubMed]
- Cooke M, Irby DM, Sullivan W, et al. American medical education 100 years after the Flexner report. N Engl J Med 2006;355:1339-44. [Crossref] [PubMed]
- Peck C, McCall M, McLaren B, et al. Continuing medical education and continuing professional development: international comparisons. BMJ 2000;320:432-5. [Crossref] [PubMed]
- Miller SH, Thompson JN, Mazmanian PE, et al. Continuing medical education, professional development, and requirements for medical licensure: a White Paper of the Conjoint Committee on Continuing Medical Education. J Contin Educ Health Prof 2008;28:95-8. [Crossref] [PubMed]
- Wojtczak, A. (2003) Glossary of Medical Education Terms. AMEE Occasional Paper No 3. Dundee:AMEE. Available online: https://www.mededworld.org/Glossary.aspx
- Mack HG, Filipe H, Golnik K. Governing the reform of the medical internship. Med J Aust 2016;205:380. [Crossref] [PubMed]
- Alahuhta S, Mellin-Olsen J, Blunnie WP, et al. Charter on continuing medical education/continuing professional development approved by the UEMS Specialist Section and European Board of Anaesthesiology. Eur J Anaesthesiol 2007;24:483-5. [Crossref] [PubMed]
- Consensus Statement of the European Medical Organisations on Continuing Professional Development, Luxembourg 2015. Available online: https://www.uems.eu/__data/assets/pdf_file/0018/29151/FINAL.EMOs.consensus.statement.CPD.December.2015.pdf
- World Federation for Medical Education. Continuing professional development (CPD) of medical doctors. WFME global standards for quality improvement [Internet]. Copenhagen 2003. Available online: http://wfme.org/standards/cpd/16-continuing-professional-development-cpd-of-medical-doctors-english/file
- Bierema LL. Systems thinking: a new lens for old problems. J Contin Educ Health Prof 2003;23:S27-33. [Crossref] [PubMed]
- Olson CA, Tooman TR. Didactic CME and practice change: don't throw that baby out quite yet. Adv Health Sci Educ Theory Pract 2012;17:441-51. [Crossref] [PubMed]
- Academy of Medical Royal Colleges [Internet]. Core Model for Royal Colleges’ and Faculties’ Continuing Professional Development Schemes. 2009. Available online: http://www.gmc-uk.org/Item_6e___Annex_D_AoMRC_CPD_Report.pdf_28991004.pdf
- Chan KKW. Medical education: From continuing medical education to continuing professional development. Asia Pac Fam Med 2002;1:88-90. [Crossref]
- Murgatroyd GB. General Medical Council: Continuing Professional Development. The international perspective 2011. Available online: http://www.gmc-uk.org/CPD___The_International_Perspective_Jul_11.pdf_44810902.pdf
- Frank JR, Snell L, Sherbino J. CanMEDS 2015 Physician Competency Framework. Ottawa: The Royal College of Physicians and Surgeons of Canada, 2015.
- Armstrong D, Reyburn H, Jones R. A study of general practitioners' reasons for changing their prescribing behaviour. BMJ 1996;312:949-52. [Crossref] [PubMed]
- Davis DA, Thomson MA, Oxman AD, et al. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA 1995;274:700-5. [Crossref] [PubMed]
- Davis D, O'Brien MA, Freemantle N, et al. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA 1999;282:867-74. [Crossref] [PubMed]
- Marinopoulos SS, Dorman T, Ratanawongsa N, et al. Effectiveness of continuing medical education. Evid Rep Technol Assess (Full Rep) 2007;1-69. [PubMed]
- Davis D, O'Brien MA, Freemantle N, et al. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA 1999;282:867-74. [Crossref] [PubMed]
- McMahon GT. What Do I Need to Learn Today?--The Evolution of CME. N Engl J Med 2016;374:1403-6. [Crossref] [PubMed]
- Gordon MJ. A review of the validity and accuracy of self-assessments in health professions training. Acad Med 1991;66:762-9. [Crossref] [PubMed]
- Woolliscroft JO, Tenhaken J, Smith J, et al. Medical students' clinical self-assessments: comparisons with external measures of performance and the students' self-assessments of overall performance and effort. Acad Med 1993;68:285-94. [Crossref] [PubMed]
- Eva KW, Regehr G. Self-assessment in the health professions: a reformulation and research agenda. Acad Med 2005;80:S46-54. [Crossref] [PubMed]
- Davis DA, Mazmanian PE, Fordis M, et al. Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA 2006;296:1094-102. [Crossref] [PubMed]
- Kruger J, Dunning D. Unskilled and unaware of it: how difficulties in recognizing one's own incompetence lead to inflated self-assessments. J Pers Soc Psychol 1999;77:1121-34. [Crossref] [PubMed]
- Campbell C, Silver I, Sherbino J, et al. Competency-based continuing professional development. Med Teach 2010;32:657-62. [Crossref] [PubMed]
- Burnett AC, Winyard G. Clinical audit at the heart of clinical effectiveness. J Qual Clin Pract 1998;18:3-19. [PubMed]
- International Council of Ophthalmology. Principles and guidelines of a curriculum for education of the ophthalmic specialist. Klin Monbl Augenheilkd 2006;223:S3-48. [PubMed]
- Filipe HP, Silva ED, Stulting AA, et al. Continuing professional development: best practices. Middle East Afr J Ophthalmol 2014;21:134-41. [Crossref] [PubMed]
- Grant J. The Good CPD Guide: A Practical Guide to Managed Continuing Professional Development in Medicine. Second Edition. London: Radcliffe Publishing, 2011.
- Brigley S, Young Y, Littlejohns P, et al. Continuing education for medical professionals: a reflective model. Postgrad Med J 1997;73:23-6. [Crossref] [PubMed]
- Filipe HP, Golnik KC. What is the CPD cycle? In Filipe HP, Mack HG, Mayorga EP, Golnik KC, editors. ICO Guide to Effective CPD/CME. San Francisco: International Council of Ophthalmology, 2015.
- Kjaer NK, Vedsted M, Høpner J. A new comprehensive model for Continuous Professional Development. Eur J Gen Pract 2017;23:20-6. [Crossref] [PubMed]
- Filipe HP, Mack HG, Mayorga EA, et al. ICO Guide to Effective CPD/CME. Available online: http://www.icoph.org/downloads/ICOGuidetoEffectiveCPDCME-PreviewEdition-February2016.pdf
- Royal Australasian College of Surgeons. A guide to surgical audit and peer review. Reviewing the outcomes of surgical care. 4th edition. Melbourne; Royal Australasian College of Surgeons, 2014.
- Challis M. AMEE Medical Education Guide No.11 (revised): Portfolio-based learning and assessment in medical education. Medical Teacher 1999;21:370-86. [Crossref]
- du Boulay C. From CME to CPD: getting better at getting better? BMJ 2000;320:393-4. [Crossref]
- Schön DA. The reflective practitioner. How professionals think in action. London: Basic Books, 1983.
- Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990;65:S63-7. [Crossref] [PubMed]
- Moore D. A framework for outcomes evaluation in the continuing professional development of physicians. In: Davis D, Barnes B, Fox R, editors. The continuing professional development of physicians. Chicago: American Medical Association Press, 2007:249-74.
- Educational Commission for Foreign Medical Graduates. Philadelphia: ECFMG; 1996-2016. ACGME Core Competencies. Available online: www.ecfmg.org/echo/acgme-core-competencies.html
- Bluestone J, Johnson P, Fullerton J, et al. Effective in-service training design and delivery: evidence from an integrative literature review. Hum Resour Health 2013;11:51. [Crossref] [PubMed]
- Schostak J, Davis M, Hanson J, et al. The Effectiveness of Continuing Professional Development. A report prepared on behalf of College of Emergency Medicine, Federation of Royal Colleges of Physicians and Manchester Metropolitan University. Commissioned by General Medical Council/Academy of Medical Royal Colleges 2010. Available online: http://www.fom.ac.uk/wp-content/uploads/cpd_efficacy_2010.pdf.
- Cervero RM, Gaines JK. The impact of CME on physician performance and patient health outcomes: an updated synthesis of systematic reviews. J Contin Educ Health Prof 2015;35:131-8. [Crossref] [PubMed]
- Jamtvedt G, Young JM, Kristoffersen DT, et al. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2006;CD000259 [PubMed]
- Mack HG, Sandhu SS, Filipe HP. Developing educators for continuing professional development. Can J Ophthalmol 2016;51:196-200. [Crossref] [PubMed]
- Swanwick T. See one, do one, then what? Faculty development in postgraduate medical education. Postgrad Med J 2008;84:339-43. [Crossref] [PubMed]
- Institute of Medicine (US) Committee on Planning a Continuing Health Professional Education Institute. Redesigning Continuing Education in the Health Professions. Washington (DC): National Academies Press (US), 2010.
- Williams BW. The prevalence and special educational requirements of dyscompetent physicians. J Contin Educ Health Prof 2006;26:173-91. [Crossref] [PubMed]
- You S. Perspective and future of evidence-based medicine. Stroke Vascular Neurology 2016.
- Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 2010;376:1923-58. [Crossref] [PubMed]
- Mitchell P, Wynia M, Golden R, et al. Core Principles & Values of Effective Team-Based Health Care. Available online: https://www.nationalahec.org/pdfs/vsrt-team-based-care-principles-values.pdf
- DIRECTIVE 2013/55/EU OF THE EUROPEAN PARLIAMENT AND OF THE COUNCILof 20 November 2013. Available online: http://eur-lex.europa.eu/LexUriServ/%20LexUriServ.do?uri=OJ:L:2013:354:0132:0170:en:PDF
- Patient Protection and Affordable Care Act of 2010, Pub. L. 111-148, USC HR 3590. Available online: https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf
- Agrawal S, Brennan N, Budetti P. The sunshine act--effects on physicians. N Engl J Med 2013;368:2054-7. [Crossref] [PubMed]
- Mack HG, Meng N, Parsons T, et al. Partnering to develop a continuing professional development program in a low-resource setting: Cambodia. Can J Ophthalmol 2017; [Crossref]
- Moore DE Jr, Green JS, Gallis HA. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Contin Educ Health Prof 2009;29:1-15. [Crossref] [PubMed]
Cite this article as: Filipe HP, Mack HG, Golnik KC. Continuing professional development: progress beyond continuing medical education. Ann Eye Sci 2017;2:46.


