
Outcomes of additional posterior to ridge diode laser versus conventional laser anterior to ridge in severe stage 3 retinopathy of prematurity—a randomized control trial
Introduction
Retinopathy of prematurity (ROP) is a proliferative retinopathy that develops in premature infants due to incomplete vasculogenesis of the retina at the time of birth. With advances in neonatal care, developing countries like India are seeing an increasing trend in the incidence of ROP constituting what is referred to as the third epidemic of ROP (1). The pathogenesis of ROP is attributed to the abnormal response of the immature retinal vasculature to both hypoxia and hyperoxia, resulting in characteristic pathological vasoproliferative lesions. Morphologic characteristics of this progressive retinopathy are used to stage the severity of disease.
The multi-center trial of Cryotherapy for Retinopathy of Prematurity (CRYO-ROP) showed that cryoablation of the peripheral avascular retina in zone I ROP reduces the very high unfavorable anatomical outcome to only 75% (2). The last two decades have seen a paradigm shift in the treatment of ROP from cryotherapy to laser photocoagulation. Data from several studies has indicated that laser therapy is superior to cryotherapy both in terms of anatomical and functional outcomes (3-5).
The vascular edge of the ridge has been identified as the site of development of retinal detachment in ROP (6). Laser therapy to the ridge has been approached with caution due to the theoretical risk of inducing tractional retinal detachment and hemorrhage. Very few studies have established the safety of laser therapy posterior to the ridge in threshold ROP (7-9). This is a randomized study which compares the efficacy and safety of additional laser posterior to the ridge to conventional laser to the avascular retina alone in threshold ROP.
Methods
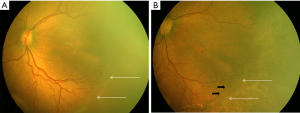
Infants requiring laser for stage 3 ROP with plus disease were enrolled in the study. An informed consent was taken from the parents and the Institutional Review Board approved the study. Forty two eyes of 24 infants were included in this study. Eighteen infants had bilateral disease and one eye was randomized to conventional laser to the peripheral avascular retina alone (control group), while the other eye received additional laser posterior to the ridge (study group). The other six infants with unilateral disease were randomized into the two treatment groups using random number table. Thus there were 21 eyes in each group. All infants were dilated with a mixture of phenylephrine 2.5% & tropicamide 0.5% instilled 3 times at 15 min interval about 45 min before the scheduled examination. A pediatric retina specialist experienced in the field of ROP performed the examination of all infants. The staging of ROP was based on the ICROP classification (10). The clinical findings of all infants included in the study were photographically documented at presentation and during follow-up using the RetCam (Clarity Medical Systems, CA, USA). Laser photocoagulation was performed under topical anesthesia in the presence of an anesthetist. Diode laser with an indirect ophthalmoscopy delivery system (Iridex Corporation, CA, USA) was used to deliver the laser. The laser spots were placed half burn width apart and the end point for laser burns was a grade 2 to 3 burn. The laser was applied to the entire avascular retina from ridge up to ora serrata in the control group. The eyes under study group received an extra two-row of laser posterior to the ridge in the vascular retina (Figure 1). The need for additional laser treatment was decided at 2 weeks follow-up. All infants were followed up for 1 year. Proportions were compared using chi square test. Mean values were compared between groups using the independent t test. A repeated measure analysis was employed (as the assessments were made are of same eye) to assess the regression of neovascularization post laser.
Results
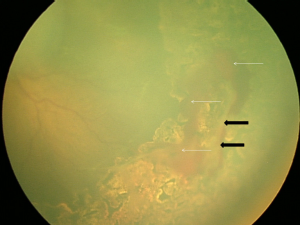
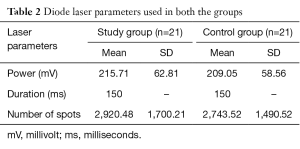
Of the 42 infants, 27 (64%) were male and 15 (36%) were female. The mean birth weight was 1,310.48±400.92 g in test group and 1,341.9±396.2 g in control group. As majority of the infants in the study (75%) had bilateral disease, the age distribution was almost similar in both groups. The mean post conceptional age at the time of intervention was 36.43±2.79 weeks in test group and 36.29±2.55 weeks in the control group. Both the groups had similar anterior and posterior segment findings (Table 1). In both the groups 16 eyes (76.2%) had zone 2 while five (23.8%) had zone 1 stage 3 disease. Diode laser was given to all. The mean power in study and control group was 215.71±62.81 and 209.05±58.56 mV respectively. The mean number of spots was higher in study group than the control group. Post laser vitreous hemorrhage was seen in two eyes (9.5%) in the study group (Figure 2) and in one eye (4.8%) in the control group but this difference was statistically not significant (P>0.05). In all the cases, the hemorrhage was mild and did not require any intervention. Table 2 compares the laser parameter details used in both groups. Four eyes (19%) in study group and five (23.8%) in control group required additional laser for persistent active disease at 2-week follow-up which again was not significant statistically (P>0.05). At 6 months follow-up, both the groups showed equal and complete regression in 20/21 eyes (95.2%). One eye from each group progressed to stage 4A which required vitrectomy.
Table 1
| Ocular findings | Study group (n=21, %) | Control group (n=21, %) |
|---|---|---|
| Anterior segment | ||
| Tunica vasculosa lentis | 3 (14.29) | 3 (14.29) |
| Rigid pupil | 2 (9.52) | 2 (9.52) |
| Cataract | 1 (4.76) | 1 (4.76) |
| Posterior segment | ||
| Zone 1 | 5 (23.8) | 5 (23.8) |
| Zone 2 | 16 (76.2) | 16 (76.2) |
Discussion
In cases with severe stage 3 ROP, the Early Treatment for Retinopathy of Prematurity (ETROP) randomized trial reported poor visual and functional outcomes following confluent laser therapy to the avascular retina alone due to inconsistent regression of the neovascular ridge (11). Hindle demonstrated histologically the benefit of treating the ridge in ROP (12).
In our study, the safety profile and anatomical outcome of additional laser posterior to the ridge is similar to conventional therapy to the avascular retina alone. This is in concordance with another randomized trial conducted by Uparkar et al. (13). In their study, a favorable anatomical outcome was obtained in 49/50 (98%) eyes treated with laser to the ridge and avascular retina and in 47/50 (94%) eyes treated conventionally. However they did not give laser posterior to the ridge. Our results also compare favorably with several other non-randomized trials. Steinmetz reported a favorable outcome in 12 eyes (75%) while Capone reported favorable outcome in 30 eyes (83.3%) (14,15). While the above-mentioned studies treated the ridge, Ells et al. employed a treatment protocol similar to our study were the vascular retina posterior to the ridge was treated avoiding the ridge (7). They reported a favorable outcome in 16 out of 18 eyes (90%), similar to our study. They hypothesized that the mechanism of action of this posterior laser may be due to destruction of the retinal pigment epithelium enabling drainage of subretinal fluid.
The potential to induce preretinal hemorrhage has been one of the limiting factors in perform laser therapy on the ridge. Uparkar et al. (13) and Steinmetz et al. (14) reported the incidence of preretinal hemorrhage to be 8% and 10% in their respective series. This was similar to our trial in which two eyes (9.52%) developed mild preretinal hemorrhage. To conclude, though additional laser treatment posterior to the ridge may be a safe treatment strategy in stage 3 threshold ROP, it provides no additional advantage in terms of faster time of regression or better anatomical outcomes. However previous studies have showed that in cases where repeat laser is required, the progression of the retinal detachment in late stage 3 or 4A ROP can be arrested by this technique especially after a failed conventional laser (7-9). Further long-term clinical trials are necessary to study the impact of this treatment strategy on functional and visual outcomes.
Full table
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.03.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional/regional/national ethics committee/ethics board and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gilbert C, Fielder A, Gordillo L, et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics 2005;115:e518-25. [Crossref] [PubMed]
- Palmer EA. Results of U.S. randomized clinical trial of cryotherapy for ROP (CRYO-ROP). Doc Ophthalmol 1990;74:245-51. [Crossref] [PubMed]
- Connolly BP, McNamara JA, Sharma S, et al. A comparison of laser photocoagulation with trans-scleral cryotherapy in the treatment of threshold retinopathy of prematurity. Ophthalmology 1998;105:1628-31. [Crossref] [PubMed]
- White JE, Repka MX. Randomized comparison of diode laser photocoagulation versus cryotherapy for threshold retinopathy of prematurity: 3-year outcome. J Pediatr Ophthalmol Strabismus 1997;34:83-7; quiz 121-2. [PubMed]
- Hendson L, Phelps D, Andersen C. Laser photocoagulation versus transscleral cryotherapy for threshold retinopathy of prematurity. Cochrane Database Syst Rev 2002;CD003847
- Pierce EA, Foley ED, Smith LE. Regulation of vascular endothelial growth factor by oxygen in a model of retinopathy of prematurity. Arch Ophthalmol 1996;114:1219-28. [Crossref] [PubMed]
- Ells AL, Gole GA, Lloyd Hildebrand P, et al. Posterior to the ridge laser treatment for severe stage 3 retinopathy of prematurity. Eye (Lond) 2013;27:525-30. [Crossref] [PubMed]
- Arvas S, Sarici AM, Akar S. Diode laser photocoagulation posterior to the ridge in severe stage 3+ threshold retinopathy of prematurity. Cutan Ocul Toxicol 2014;33:197-200. [Crossref] [PubMed]
- O’Keefe M, Burke J, Algawi K, et al. Diode laser photocoagulation to the vascular retina for progressively advancing retinopathy of prematurity. Br J Ophthalmol 1995;79:1012-4. [Crossref] [PubMed]
- International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol 2005;123:991-9. [Crossref] [PubMed]
- Good WVEarly Treatment for Retinopathy of Prematurity Cooperative Group. Final results of the Early Treatment for Retinopathy of Prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc 2004;102:233-48; discussion 248-50. [PubMed]
- Hindle NW. Critical mass retinopathy of prematurity: what is it and what can you do about it? Doc Ophthalmol 1990;74:253-62. [Crossref] [PubMed]
- Uparkar M, Sen P, Rawal A, et al. Laser photocoagulation (810 nm diode) for threshold retinopathy of prematurity: a prospective randomized pilot study of treatment to ridge and avascular retina versus avascular retina alone. Int Ophthalmol 2011;31:3-8. [Crossref] [PubMed]
- Steinmetz RL, Brooks HL Jr. Diode laser photocoagulation to the ridge and avascular retina in threshold retinopathy of prematurity. Retina 2002;22:48-52. [Crossref] [PubMed]
- Capone A Jr, Diaz-Rohena R, Sternberg P Jr, et al. Diode-laser photocoagulation for zone 1 threshold retinopathy of prematurity. Am J Ophthalmol 1993;116:444-50. [Crossref] [PubMed]
Cite this article as: Sindhu A, Siddharth N, Shah PK, Narendran V, Kalpana N. Outcomes of additional posterior to ridge diode laser versus conventional laser anterior to ridge in severe stage 3 retinopathy of prematurity—a randomized control trial. Ann Eye Sci 2017;2:49.


