Safety and efficacy of trans-scleral glued intraocular lens implantation
Introduction
For most of the cataract surgeons, securely placing an intraocular lens (IOL) in the eye with weak zonules, in eyes with a rent in a posterior capsule or lack of posterior capsular support had been a problem for a long time (1). The usual modalities used in such cases include iris fixated IOL, anterior chamber (AC) IOL, sutured and suture less trans-scleral fixated IOL.
Severe endothelial cell loss and morphologic changes leading to pseudophakic bullous keratopathy and chronic uveitis were seen in patients who had been implanted with AC lenses (2). Other complications of AC lens implants after long term follow up include late ‘iris ovalling’, iris tuck and progressive endothelial cell loss throughout the life in all operated eyes and this progressive cell loss was greater in eyes with iris tuck (3).
Long term follow up studies have found that there were chances for slippage of one or both of the iris-claw haptics and spontaneous complete posterior dislocation. Cases also presented with retinal detachment, cystoid macular edema and post-operative increased intraocular pressures, which was managed medically with topical anti-glaucoma drugs (4).
Some of the limitations in the sutured scleral fixated intraocular lenses (SFIOL) were surgical expertise, prolonged surgical time, suture induced inflammation, suture degradation and delayed IOL subluxation or dislocation due to any broken suture (5).
Fibrin glue to implant a posterior chamber intraocular lens (PCIOL) in eyes with a deficient or absent posterior capsule was introduced. Two partial-thickness limbal based scleral flaps were made 180 degrees apart diagonally, and the haptics of the PCIOL were externalized to place them beneath the flaps. Fibrin glue was used to attach the haptics to the scleral bed, beneath the flap (6). Modification of SFIOL technique was also tried and found to be as safe and effective as conventional techniques (7).
Fibrin glue has two components that occur naturally in the blood namely fibrinogen and thrombin. They were separated before use, when mixed, thrombin converts fibrinogen to fibrin producing local fibrin clot. Glued IOLs were found to be safe, when implanted in eyes with micro cornea using modifications such as custom haptic trimming and 6.0 mm optic foldable IOL’s (8). Multifocal IOL can also be scleral fixated with fibrin glue.
Common complications encountered were decentration of the IOL requiring repositioning, Optic capture, mostly observed with PMMA three piece IOL and was less common in foldable glued IOL. Chronic macular edema and sub conjunctival haptic visibility were also reported. However, there was no post-operative secondary glaucoma or endophthalmitis in any of the cases.
Hence suture less, trans-scleral fixated glued IOL was found to be an effective surgical modality in patients for whom endocapsular placement of PCIOL is not possible. This prompted us to do this retrospective study on visual outcome and complications for all Glued IOL surgeries performed in our eye hospital.
Methods
Study protocol was made for retrospective analysis of “Safety and efficacy of trans-scleral glued intraocular lens”, after scientific committee and ethical committee clearance of our institution (Ethical approval ID: 011/AFEH/2016). Twenty-eight cases of Glued IOL fixation, performed by a single surgeon over a 4-year period were identified. Pre-operative data included demographics and etiology of aphakia. Pre-operative and post-operative evaluations comprised objective and subjective refraction, slit lamp bio microscopy, non-contact tonometry and dilated fundus examination. The IOL power was calculated by the SRK-T formula using an A constant of 118.5. Visual acuity was converted to Log MAR for statistical ease and analysis was done using Microsoft Excel.
The Glued IOL used was of MATRIX optics- three piece biconvex hydrophobic foldable UV [384] posterior chamber IOL with overall 12 mm, length 6.0 mm and optic diameter of 6.0 mm.
Glued IOL implantations were done under peribulbar anesthesia except for the pediatric patients who were given general anesthesia. It was done as a secondary procedure in the surgical aphakia and trauma groups. But in the subluxated/dislocated lens and Nucleus/IOL drop/explantation groups, along with glued IOL implantation, pars plana lensectomy + pars plana victrectomy + IOL explantation/phacofragmentation were done respectively as a primary procedure.
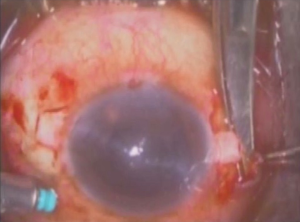
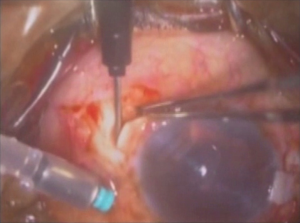
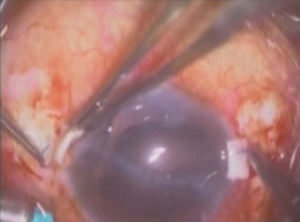
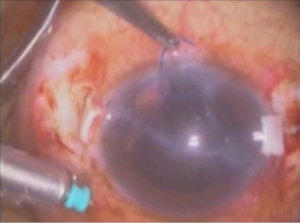
The glued IOL technique involves making two partial thickness scleral flaps exactly 180° apart followed by a sclerotomy with a 22-gauge needle at 1.5 mm from the limbus as shown in Figures 1 and 2 respectively. After that 25-gauge microsurgical technology forceps were passed through the sclerotomy which was used to grasp the IOL haptic and brought out onto the ocular surface as represented in Figure 3. Tunnels were made at the edge of the flap with a 26-gauge needle into which the two haptics were then tucked for additional stability as presented in Figure 4. The scleral flaps were then glued back into place using biological glue. The glue used was a quick-acting surgical fibrin sealant derived from human blood plasma (Tisseel, Baxter) with both hemostatic and adhesive properties.
Results
The study group consisted of 17 males and 11 females. The mean age of males was 39.1±4.6 years with minimum age of 12 to 76 years. The mean age of females was 37.9±7.5 years with minimum age of 8 to 75 years.
Glued IOL was implanted in 13 traumatic cataracts with subluxation (46.4%) and nine aphakic patients (32.1%). The other indications for glued IOL along with number of eyes and percentage are depicted in Table 1.
Table 1
| S. no. | Indications for glued IOL | Number | Percentage |
|---|---|---|---|
| 1 | Aphakia | 9 | 32.1 |
| 2 | Traumatic cataract with subluxation | 13 | 46.4 |
| 3 | Typical complete lenticulo-chorioretinal coloboma | 2 | 7.1 |
| 4 | Surgical aphakia after congenital cataract extraction | 1 | 3.6 |
| 5 | Absorbed cataract without capsular support | 1 | 3.6 |
| 6 | Congenital subluxation associated Marfan’s syndrome | 1 | 3.6 |
| 7 | Lens drop | 1 | 3.6 |
IOL, intraocular lens.
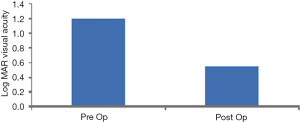
The mean pre-operative and post-operative Log MAR acuity was found to be 1.18 and 0.55 respectively as displayed in Figure 5. A paired t test was performed between the pre- and post-operative Log MAR acuities which revealed statistical significance with P=0.00. The mean pre-operative and post-operative astigmatism was found to be 1.08 D and 0.62 D respectively indicating no statistical significance with P>0.05.
There were no associated ocular manifestations for 64.2% of the study population. For the remaining population, the most common associated ocular abnormality was penetrating ocular trauma with corneal tear (10.6%) and the other ocular associations are listed in Table 2.
Table 2
| S. no. | Ocular associations | Number | Percentage (%) |
|---|---|---|---|
| 1. | Penetrating ocular trauma with corneal tear | 3 | 10.6 |
| 2. | Amblyopia | 2 | 7.2 |
| 3 | Wet ARMD | 1 | 3.6 |
| 4 | Congenital subluxation associated Marfan’s syndrome | 1 | 3.6 |
| 5 | Lattice degeneration | 1 | 3.6 |
| 6 | Typical complete lenticulo-chorioretinal Coloboma | 2 | 7.2 |
| 7 | Without any ocular association | 18 | 64.2 |
Most of the patients had uneventful intra operative and post-operative period with satisfactory visual outcome. The mean follow up of all the patients was 15.2±12.9 months with minimum and maximum of 5 and 43 months respectively. About 89% of the study population had no postoperative complications. Postoperative complications were seen in 11% of the cases and are given in Table 3. These complications were well managed in succeeding follow up visits. One patient with megalocornea and secondary aphakia (congenital cataract surgery done elsewhere) developed dislocated glued IOL after 9 months due to improper sizing of the IOL. He later underwent explanation of Glued IOL and implantation of iris fixated IOL. This patient’s post-operative Log MAR acuity was found to be 0.3. Two cases had dislocated IOL after 2 months post-operatively. One case had a spontaneous dislocation and the second one had a blunt trauma postoperatively. These two patients who had dislocated glued IOL, developed retinal breaks along with PVD, which led to rhegmatogenous retinal detachment (RRD). Both the cases underwent pars plana-victrectomy, internal limiting membrane peeling, endolaser, silicon oil implantation with Glued IOL repositioning. Out of these, one patient had post-operative Log MAR acuity which improved to 0.2 and other had post-operative Log MAR acuity of 0.8.
Table 3
| S. no. | Complications | Number | Percentage |
|---|---|---|---|
| 1 | Dislocated glued IOL | 1 | 3.6 |
| 2 | Dislocated glued IOL with RD | 2 | 7.2 |
IOL, intraocular lens; RD, retinal detachment.
Preoperative and postoperative intraocular pressures were measured with non-contact tonometer. Mean pre-operative IOP was 14.6±7.14 mm of Hg and mean postoperative IOP was 14.7±3.72 mm of Hg. A paired t test was performed and found that there was no statistical significance in IOP with P>0.05.
Discussion
All types of ocular trauma can lead to lens damage causing traumatic cataract, traumatic subluxation of lens, with or without posterior capsular damage or zonular dialysis. In such situations, most of the cases will not have adequate capsular/zonular support to implant a posterior chamber IOL in the bag or in the ciliary sulcus. In such cases, an IOL can be placed in the AC, as closed or open-loop anterior chamber IOLs (ACIOLs), in iris as retro-iris-fixated IOL's and with sutures or suture less (Glued) trans-scleral fixated IOL. There are high risks of severe corneal endothelial cell loss, chronic low grade uveitis in cases with implanted ACIOL and iris fixated IOL (9).
In our study, especially in post-traumatic patients with subluxated traumatic cataract, trans-scleral fixated IOL had a theoretical advantage over other types of IOLs with regards to complications because of the anatomical location. These IOLs provide better visual acuity and binocularity, and avoid complications of ACIOLs and iris fixated IOLs (9).
Sutured trans-scleral fixated IOLs were associated with visually significant complications due to late subluxation, higher risk of axial IOL tilt, complications related to sutures, exposed IOL haptic and exposed suture and potential risks of endophthalmitis (10). Another added benefit to glued IOL implantation was the ability to use currently available IOLs in contrast to other non-endocapsular procedures which require special lenses (11).
In our study of 28 eyes, glued IOL was implanted in 9 surgically induced aphakic patients (32.1%), 13 patients with traumatic cataracts along with subluxation (46.4%), as compared to other studies (9), where it was done only as secondary procedure in surgically induced aphakia due to intraoperative posterior capsular rent. They had post-operative Log MAR BCVA of 0.57±0.24 and was almost similar to our study where it was found to be 0.55±035.
Ocular hypertension was observed in only 0.4% of glued IOL patients compared to 30.5–50% in sutured scleral fixated IOL (11). Also in our study, there was no significant effect on IOP postoperatively. In glued IOL the haptics were tucked in the scleral pockets and the flaps were then adhered to the base with the help of tissue fibrin glue. The glue also helped in sealing the sclerotomy site which would otherwise act as a filtration site and cause hypotony. Hypotony was not observed in any of the case included in our study.
The haptics are placed in its normal curved configuration without traction and hence no distortion in the shape of the IOL optic. Externalization of the haptics, stabilized the axial positioning of the IOL and thereby prevented IOL tilt. The use of scleral tunnel fixation of the haptic using fibrin glue was technically less demanding and it stabilized the three piece IOL in the posterior chamber without the difficulty of suturing as in case of sutures in intra scleral fixated IOLs (12). Placing the IOL haptic beneath the flap further stabilized the movement of the haptics, and thus optic was held in place, reducing the pseudophacodonesis. There were Patients who had undergone fibrin glue assisted intrascleral fixation of 3 piece IOL combined with DSAEK (13). IOL fixation was strong enough to sustain the manipulation required for corneal procedure with a good postoperative centration. The ends of the haptic were left underneath the tunnel preventing foreign body sensation, erosion of the conjunctiva and also reduced the risk of inflammation and late post-operative endophthalmitis. In our study, there were three cases of dislocated glued IOL. One case was due to the blunt trauma which was sustained postoperatively. The second case was due to the improper sizing of the IOL in a case of megalocornea. The actual dislocation of glued IOL was 1 out of 28 cases, which is 3.5%.
The only limitation in this study was short term follow up visits. A prospective and long follow up study may give rise to better results. However this technique is promising and has yielded good and significant postoperative visual acuity.
Conclusions
This study resulted in good prognosis of glued IOL surgical technique with 89% success rate and no postoperative complications with statistically significant improvement in visual acuity.
Acknowledgments
We wish to thank our Consultant Ophthalmologist Dr. Satyajit MV for his valuable suggestion and inputs throughout the study.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.06.07). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was waived due to the retrospective nature of the study. The study was approved by scientific committee and ethical committee clearance of our institution (Ethical approval ID: 011/AFEH/2016).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kumar DA, Agarwal A, Agarwal A, et al. Glued intraocular lens implantation for eyes with defective capsules: A retrospective analysis of anatomical and functional outcome. Saudi J Ophthalmol 2011;25:245-54. [Crossref] [PubMed]
- Numa A, Nakamura J, Takashima M, et al. Long-term corneal endothelial changes after intraocular lens implantation. Anterior vs posterior chamber lenses. Jpn J Ophthalmol 1993;37:78-87. [PubMed]
- Walters RF, McGill JI, Batterbury M, et al. Complications of anterior chamber lens implants and their effects on the endothelium. Eye (Lond) 1989;3:690-5. [Crossref] [PubMed]
- Forlini M, Soliman W, Bratu A, et al. Long-term follow-up of retropupillary iris-claw intraocular lens implantation: a retrospective analysis. BMC Ophthalmol 2015;15:143. [Crossref] [PubMed]
- Price MO, Price FW Jr, Werner L, et al. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg 2005;31:1320-6. [Crossref] [PubMed]
- Agarwal A, Kumar DA, Jacob S, et al. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg 2008;34:1433-8. [Crossref] [PubMed]
- Young AL, Leung GY, Cheng LL, et al. A modified technique of scleral fixated intraocular lenses for aphakic correction. Eye (Lond) 2005;19:19-22. [Crossref] [PubMed]
- Ashok Kumar D, Agarwal A, Sivangnanam S, et al. Implantation of glued intraocular lenses in eyes with microcornea. J Cataract Refract Surg 2015;41:327-33. [Crossref] [PubMed]
- Narang P, Narang S. Glue-assisted intrascleral fixation of posterior chamber intraocular lens. Indian J Ophthalmol 2013;61:163-7. [Crossref] [PubMed]
- Ganekal S, Venkataratnam S, Dorairaj S, et al. Comparative evaluation of suture-assisted and fibrin glue-assisted scleral fixated intraocular lens implantation. J Refract Surg 2012;28:249-52. [Crossref] [PubMed]
- Williamson S, Watkins W Jr, Thinda S, et al. Review of “Complications and visual outcomes after glued foldable intraocular lens implantation in eyes with inadequate capsules”. EyeWorld journal club, 2013.
- Scharioth GB. A European surgeon offers his views on the treatment of luxated intraocular lenses. IOL Fixation Techniques 2009.
- Sinha R, Shekhar H, Sharma N, et al. Intrascleral fibrin glue intraocular lens fixation combined with Descemet-stripping automated endothelial keratoplasty or penetrating keratoplasty. J Cataract Refract Surg 2012;38:1240-5. [Crossref] [PubMed]
Cite this article as: Maheshwari R, Vaishnavi T, Revanasiddappa I, Joseph J, Kalikivayi V, Jacob SC. Safety and efficacy of trans-scleral glued intraocular lens implantation. Ann Eye Sci 2017;2:54.