Allogeneic sclera graft combined autologous conjunctival flap for repairing the emergent corneal perforation
Introduction
Intractable corneal perforation is one of the severe complications in the ocular chemical burn, infectious, and immunological corneal ulcer. Amniotic membrane transplantation (AMT), buccal mucosa or conjunctival graft is considered as an alternative candidate for repairing corneal perforation (1-3). However, none of them is available for a more than 2-mm perforation due to their little tension cannot bear the intraocular pressure (4-6). Penetrating keratoplasty (PK) is a desirable method to address this devastating situation. However, donor corneal graft is a severe shortage in many countries, especially in China. Not every patient is so lucky to get a donor graft at that point the corneal perforations occur. Without the proper treatment, the contents of eyeball will gush out through the perforation, necessitating evisceration or enucleation, resulting in more cosmetological and psychological damages which are more serious than the disease itself.
Under such emergent condition, the preserved allogeneic sclera is a viable alternative for addressing the lack of an available donor corneal graft. Allogeneic sclera graft is available from eye bank and can be easily preserved for several months. It consists of collagen fibers and is so strong, flexible and easy to handle. Larsson (7) employed sclera graft to repair corneal perforation caused by exposure. Several other studies showed that sclera graft was a definitive strategy for repairing corneal perforation to avoid the potential infection and/or endophthalmitis (8-10). However, sclera graft without epithelia is so-called ‘bared graft’ and seems so difficult to survive on corneal bed due to delaying re-epithelialization (11). Additionally, sclera graft is the lack of vascularization, which is dispositive to necrosis, degradation, and shedding after transplantation (12,13).
In this report, we introduced a palliative and alternative surgical procedure, an allogeneic sclera graft combined with autologous conjunctival flap (ASGACF), to repair the large emergent corneal perforation. Encouraging results were achieved in each of patients. We believed that this procedure could be valuable for repairing large emergent corneal perforation while there is the lack of a donor corneal graft.
Surgical procedure
The donor sclera graft was obtained from Eye Bank of Shaanxi Province, immersed into 75% ethanol solution for 48h for sterilization and then transferred into glycerol at −70 °C. Before the operation, it was rinsed with saline and immersed in BBS solution containing gentamicin 20 mg/mL for 10 min.
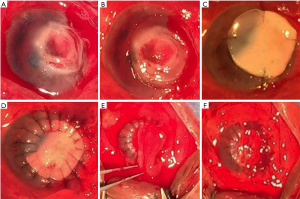
The detail protocol of the surgical procedure was as follows (Figure 1): after local anesthesia of the affected eye, prepared an anterior chamber paracentesis at 11 o’clock position and infused viscoelastic substance (Healonid, AMO) into the anterior chamber to restore the prolapse and/or anterior synechiae iris. Then, marked the edge of the surgical corneal bed with a corneal trephine, 1.0 mm larger than the area of the corneal perforation (for the infectious corneal perforation, the bed size was determined according to the lesion area). Along the edge, the affected cornea was removed using the corneal scissors. The donor sclera graft was manually trimmed to the appropriate thickness and size, 0.75 mm larger than the surgical bed, and sutured to the recipient bed with the interrupted 10-0 nylon suture. A pedicle autologous conjunctival flap with a thin fascia, about half of the sclera graft in width, was prepared and sutured onto the sclera graft with 10-0 nylon suture. Any effusion beneath the conjunctival flap should be driven out so that the flap could be closely attached to the sclera graft.
The eyes were bandaged after surgery and opened the next day. Topical corticosteroids, antibiotics, and lubricant eye drops were prescribed and gradually tapered in 1 month. Surgical success was defined as healing the perforation and restoring the integral wall of the eyeball in 3–6-month follow-up, but failure was as sclera graft melting and recurring perforation in the original position.
Case presentation
This study was approved by the Ethical Board of Shaanxi Provincial Institute of Ophthalmology. The prognosis and complication of ASGACF were explained to all the patients. A written informed consent was obtained from each of them.
Case 1
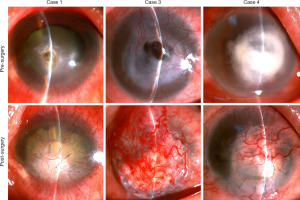
A 43-year-old male suffered from a corneal ulcer perforation in the left eye. His medical history revealed that he had removed the corneal foreign body in the left eye 1 year before. The best-corrected visual acuity was negative light perception. Slit lamp examination showed a 4-mm diameter corneal ulcer and 2.5-mm perforation in the affected eye. Moreover, a metal foreign body was found in vitreous chamber, accompanied with long-standing whole retinal detachment. The ASGACF was performed on the affected eye and sealed the corneal perforation successively in the 6-month follow-up, which rescued the integral wall of the eyeball (Figure 2).
Case 2
A 62-year-old male was referred for acute onset of a 7-mm diameter corneal ulcer in the left eye. A 3–3.5 mm perforation occurred in the area of corneal ulcer sooner after 4-days anti-inflammatory therapy. Then, the ASGACF was performed and was successively sealed the corneal perforation in the 6-month follow-up.
Case 3
A 69-year-old male suffered from a severe alkali burn in the right eye 7 months before. Despite our best efforts at medical management, repeated corneal melts occurred and ultimately led to a 3.0-mm diameter perforation in the center of the cornea. Then, the ASGACF was performed but the superior cornea-sclera graft junction ruptured out and the conjunctival flap fell off 2 weeks later, due to the secondary glaucoma. The second surgery was performed to suture the rupture and cover with a new conjunctival flap again, following with the cyclocryosurgery to control intraocular pressure. In the follow-up, the conjunctival flap survived and the ASGACF restored the integral wall of eyeball (Figure 2).
Case 4
A 60-year-old male suffered from an infectious corneal ulcer in the left eye. Slit lamp examination revealed that there was a 7-mm diameter ulcer deepened to Descemet’s membrane in center cornea and 3-mm empyema in the lower anterior chamber. The best-corrected vision was light perception. Only 2 days later, a 3-mm corneal perforation occurred and the anterior chamber disappeared immediately. Then the ASGACF was performed for him and also successively repaired the corneal perforation in the 6-month follow-up (Figure 2).
Discussion
Corneal perforation is an ocular emergency and, if not managed promptly and effectively, can cause devastating consequences. Facing this condition, the primary importance step is to restore the integral wall of the eyeball and ocular tension.
Human homograft and autograft techniques are commonly employed today to manage those diseases that compromise the tectonic stability of the eye, including AMT, conjunctival flaps, keratoplasty and scleral patch grafts (14,15). The amniotic membrane consists of a thick basement membrane and an avascular stroma and is endowed with the anti-inflammatory, antifibrotic, and epithelialization-promoting property. It is immunologically inert and popularly employed in ocular surface reconstruction and corneal ulcers or perforation (16), which acting both as a graft to replace damaged ocular stroma and as a patch to reduce inflammation and promote healing. However, AMT only partially restored corneal stromal thickness, leading to the persisting corneal thinning. On the other hand, it does not provide adequate tectonic rigidity by itself alone and is amenable to rapid disintegration and loss, which doomed the application of AMT only in the small corneal perforation but not a large one (17). Conjunctival flaps could be used for a small eccentric corneal perforation, but could not seal a large corneal perforation alone, due to the leap would continue under the flap (4,6). Therapeutic keratoplasty offers more benefits over the others, but its success in the acute setting of corneal inflammation and/or perforation is variable and generally poor (14). Furthermore, the donor graft is the shortage and cannot be ready for order at any needed time. Scleral graft has many intrinsic advantages in this scenario (13). However, failure of scleral grafts has been reported just owing to the lack of vascularization, leading to the resultant necrosis and sloughing (12,13). The scleral graft does not contain epithelium so that it is difficult for it to survive on an avascular surface (11).
Under an emergent situation, on the one side, the corneal perforation is so large that AMT or conjunctival flap fails to close it alone. On the other side, there is no a donor cornea at hand. Addressing this condition, we performed the ASGACF on each of the patients with large corneal perforations and achieved encouraging results. The success of this combined procedure could be attributed to the following aspects. Firstly, sclera graft with little immunogenicity had a lower risk of immune rejection and histolysis. Secondly, sclera graft reconstructed the integral wall of eyeball immediately and formed a strong barrier between aqueous humor and conjunctival flap, which facilitated conjunctival flap to closely attach to graft. Thirdly, conjunctival flap, rich in plenty of blood vessels, provided the blood supply for sclera graft, thus preventing it from ischemic histolysis or necrosis. Ultimately, conjunctival flap provided many epithelial seed cells to accelerate re-epithelization of the ‘bare graft’ (18), which also protected sclera graft from histolysis or shedding.
In summary, under the emergent condition, the ASGACF is a palliative and alternative surgical procedure for repairing a large corneal perforation while there is the lack of a donor corneal graft. Tectonic integral wall of eyeball was salvaged, which minimized the psychological and cosmetological damages to the patients, compared with evisceration or enucleation.
Acknowledgments
Funding: This work was supported by grants from Shaanxi Provincial Natural Science Basic Research Program (NO. 2016JM8017).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.09.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Arora R, Mehta D, Jain V. Amniotic membrane transplantation in acute chemical burns. Eye (Lond) 2005;19:273-8. [Crossref] [PubMed]
- Berguiga M, Mameletzi E, Nicolas M, et al. Long-term follow-up of multilayer amniotic membrane transplantation (MLAMT) for non-traumatic corneal perforations or deep ulcers with descemetocele. Klin Monbl Augenheilkd 2013;230:413-8. [Crossref] [PubMed]
- Rodríguez-Ares MT, Touriño R, López-Valladares MJ, et al. Multilayer amniotic membrane transplantation in the treatment of corneal perforations. Cornea 2004;23:577-83. [Crossref] [PubMed]
- Jhanji V, Young AL, Mehta JS, et al. Management of corneal perforation. Surv Ophthalmol 2011;56:522-38. [Crossref] [PubMed]
- Por YM, Tan YL, Mehta JS, et al. Intracameral fibrin tissue sealant as an adjunct in tectonic lamellar keratoplasty for large corneal perforations. Cornea 2009;28:451-5. [Crossref] [PubMed]
- Bhatt PR, Lim LT, Ramaesh K. Therapeutic deep lamellar keratoplasty for corneal perforations. Eye (Lond) 2007;21:1168-73. [Crossref] [PubMed]
- Larsson S. Treatment of perforated corneal ulcer by autoplastic scleral transplantation. Br J Ophthalmol 1948;32:54-7. [Crossref] [PubMed]
- Turner SJ, Johnson Z, Corbett M, et al. Scleral autoplasty for the repair of corneal perforations: a case series. Br J Ophthalmol 2010;94:669-70. [Crossref] [PubMed]
- Prasher P. Use of an autologous lamellar scleral graft to repair a corneal perforation. Int Ophthalmol 2014;34:957-60. [Crossref] [PubMed]
- Prydal JI. Use of an autologous lamellar scleral graft to repair a corneal perforation. Br J Ophthalmol 2006;90:924. [Crossref] [PubMed]
- Mansour AM, Bashshur Z. Surgically induced scleral necrosis. Eye (Lond) 1999;13:723-4. [Crossref] [PubMed]
- Nguyen QD, Foster CS. Scleral patch graft in the management of necrotizing scleritis. Int Ophthalmol Clin 1999;39:109-31. [Crossref] [PubMed]
- Sangwan VS, Jain V, Gupta P. Structural and functional outcome of scleral patch graft. Eye (Lond) 2007;21:930-5. [Crossref] [PubMed]
- Portnoy SL, Insler MS, Kaufman HE. Surgical management of corneal ulceration and perforation. Surv Ophthalmol 1989;34:47-58. [Crossref] [PubMed]
- Sandinha T, Zaher SS, Roberts F, et al. Superior forniceal conjunctival advancement pedicles (SFCAP) in the management of acute and impending corneal perforations. Eye (Lond) 2006;20:84-9. [Crossref] [PubMed]
- Arora R, Mehta D, Jain V. Amniotic membrane transplantation in acute chemical burns. Eye (Lond) 2005;19:273-8. [Crossref] [PubMed]
- Prabhasawat P, Tesavibul N, Komolsuradej W. Single and multilayer amniotic membrane transplantation for persistent corneal epithelial defect with and without stromal thinning and perforation. Br J Ophthalmol 2001;85:1455-63. [Crossref] [PubMed]
- Mauger TF, Craig E. Combined acanthamoeba and Stenotrophomonas maltophilia keratitis treated with a conjunctival flap followed by penetrating keratoplasty. Cornea 2006;25:631-3. [Crossref] [PubMed]
Cite this article as: Wang S, Tian Y, Zhu H, Cheng Y, Wu J. Allogeneic sclera graft combined autologous conjunctival flap for repairing the emergent corneal perforation. Ann Eye Sci 2017;2:66.