Expert’s introduction
Prof. Anuj Chauhan (Figure 1) is a professor of Chemical Engineering at the University of Florida, USA. He was born and raised in India and moved to the United States to receive his Ph.D. degree in Chemical Engineering at the City University of New York. He completed his postdoctoral degree at the University of California, Berkeley. His areas of expertise include tear film dynamics, ophthalmic drug delivery, contact lenses, drug detoxification and microfluidics.
Editor’s note
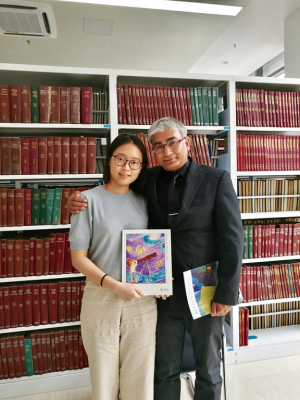
The 2nd Guangzhou International Glaucoma Forum was held successfully at Zhongshan Ophthalmic Center, Sun Yat-Sen University on 21, 22 April, 2018. Many international experts from USA, UK, Austria, Israel and Korea were invited to this forum to share and discuss the latest research results on diagnosis, drug treatment and minimally invasive surgical treatment of glaucoma. At this forum, we Annals of Eye Science (AES) had the great honor to invite Prof. Anuj Chauhan from the Department of Chemical Engineering, University of Florida, Gainesville, FL, United States to have an exclusive interview with us, leading our readers to learn more about the latest application of contact lenses in glaucoma treatment (Figure 2).
Interview
AES: Ophthalmic drug delivery by contact lenses is a potential treatment for glaucoma, could you briefly tell us the mechanism of how it works?
Prof. Chauhan: Sure, so the drugs we are interested in are currently delivered by eyedrops. When you put in an eyedrop, what happen is that the drug drains from the eye very quickly, and only about 1% of the drugs make it to the cornea and the target tissue. That has actually been well-known for decades. Now, because contact lenses are placed on the cornea, what happen is, the drug that gets out of the cornea from the back side, most of it actually ends up in the target tissue. The drug goes through the cornea and into the aqueous humour, and then interacts with the target tissue. In this way, it has much better efficacy because a very large fraction of the drug gets to the target issue, that’s the main benefit of the contact lenses. So the basic mechanism of how contact lenses work is the same as eyedrops, the drug still has to go through the cornea and interact with the target tissue. What we are doing now is improving the pharmacokinetics so that we are able to deliver our drug at the controlled rates and a high fraction of the drug actually makes it to the cornea.
AES: What are the advantages of using contact lenses to deliver ophthalmic drugs compared to eyedrops?
Prof. Chauhan: The biggest advantage of using contact lenses is that you can get a much higher fraction of the drugs into the cornea. Another advantage is compliance, for some diseases, patients need to deliver drug very frequently. For patients with glaucoma, it’s typically once a day or twice a day. There are some other diseases, like Cystinosis, which is an awful disease we are working on, you have to deliver the drug every hour every day for your entire life. You can imagine that is extremely tedious. With a contact lens, we can replace that with potentially just having to wear one contact lens everyday and only for a few hours. This could improve compliance, because patients would rather put a contact lens in for a few hours than put eyedrops every hour. So the biggest benefit is definitely improving our pharmacokinetics but also for some other diseases, the benefits might be improving compliance. There are also other advantages, currently for some diseases, the drugs are delivered to the back of the eye by intravitreal injections. However, with the contact lens, we think that we could actually get the drug to the back of the eye without using any injection. We may be able to replace the intravitreal injection with the contact lens, which of course would be a very big improvement, because we can make the therapy significantly less invasive.
AES: You and your team have developed novel nanoparticle-laden soft contact lenses which can increase the fraction of the entrapped drug that enters the cornea, did you face any challenges during this research?
Prof. Chauhan: I think there are many challenges. The biggest challenge was that the contact lens needs to have certain critical properties. It has to be transparent, it has to allow oxygen to go through, it has to allow ions to go through, it has to be soft, it has to not have protein binding, it should be lubricious, it needs to be wettable. You need to have all those properties in contact lens, you can’t change those because those are critical, but yet you want to control the drug release time scale. If you take a commercial contact lens and try to put the drug into the lens, the drug comes out very quickly. After about one hour, the drugs are gone, you know it’s not very suitable. So the challenge was how to improve the drug release kinetics without impacting any other property. Now we have achieved that with multiple technologies, but that was the biggest challenge at the time.
AES: As animal trials of this research are already undergoing, what is the schedule for clinical trials?
Prof. Chauhan: We actually have a clinical trial as well ongoing, it’s a glaucoma trial. We already started the safety study and the results showed these lenses are safe and comfortable. The efficacy study should start in a couple of months hopefully. This study is with COSOPT, COSOPT is a combination therapy. It is a mixture of two drugs, dorzolamide and timolol, so we put those drugs inside a contact lens and then we release those drugs into the patient’s eyes. The animal study was very successful; that’s the reason why we are trying the human study. The animal study showed that if you put the contact lens on the eye for four days, you actually get efficacy for about 15 days. That’s great, because that could significantly improve the compliance as patients don’t want to deliver drugs every day. If we can design a contact lens that needs to be worn just for 1 day and have efficacy for 7 days. That would be really exciting. Because even though you can not insert a contact lens, you can ask your friends or parents or somebody else to put the lens in your eyes and at the end of the day you can take it off. You don't have to do anything in the rest of the week. If we could achieve that, I think it will be a great improvement for delivering drugs to the eyes.
AES: Do you expect any product based on this technology to be released soon?
Prof. Chauhan: Well, then you need to define soon first. The problem with clinical studies is that these studies need to be multi-center studies. We usually need hundreds of patients. This is just the first study we have started, so it is difficult to speculate when the product can come out. But we are definitely very hopeful, we are also very hopeful that we can get a product for Cystinosis, the other disease we are looking at. Another big challenge is of course raising the funds for the clinical study, because it’s very expensive. Hopefully soon, but I think it will still take probably a couple of years.
AES: What are the issues needed to be resolved in the future for ophthalmic drug delivery?
Prof. Chauhan: I think the challenges are still the same which is targeting. How do you get the drug to the target with high efficacy and with the compliance. Right now, I think the biggest challenge is compliance which has been a problem all along. You can tell patients that you need to take the drugs, but a lot of times the patients just don't take the drugs, especially for a disease like glaucoma, because you don't sense the pressure at the eye. I think anytime you are aware of the disease, you tend to apply the drug, like infections, you can see the infections, so you use the drugs. For glaucoma, it’s why they call it the “silent killer”. You don’t sense the pressure, you just forget about it. I think that is very critical—how to get good compliance. And we need to effectively treat diseases affecting the back of the eye, hopefully without injection. It is better that we don't have to use invasive therapies like intravitreal injection. I think those are probably the biggest challenges.
Acknowledgments
Funding: None.
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Eye Science for the series “Meet the Professor”. The article did not undergo external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.05.06). The series “Meet the Professor” was commissioned by the editorial office without any funding or sponsorship. Tan-Lun Yu reports that she is a full-time employee of the AME publishing company (publisher of the journal). The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
(Science Editor: Tan-Lun Yu, AES, aes@amegroups.com)
doi: 10.21037/aes.2018.05.06
Cite this article as: Yu TL. Prof. Anuj Chauhan: contact lenses as the future of glaucoma treatment. Ann Eye Sci 2018;3:27.