Using a rigid lens as endocapsular supporting device in cataract surgery for moderate subluxated cataracts
Introduction
Surgical management of subluxated cataract presents a challenge to cataract surgeons (1-3). Such surgery is now relatively safe with the help of capsular support devices, such as capsule tension rings (CTR) and modified CTR with single or double fixation points (2,3). The use of CTR has enabled surgeons to achieve safer cataract removal by preventing iatrogenic loss of zonular support, minimizing vitreous loss. However, whether implanted before or after lens extraction, it required more involved intraocular manipulation and weaknesses persist (i.e., difficulty removing cortical material and significant capsular torque) (4,5).
Manual small incision cataract surgery (MSICS) has been shown to be as effective and safe as phacoemulsification in treating ectopia lentis. It provides a closed stable chamber with a well-expanded capsular bag for greater control. Moreover, it is faster, less expensive, and less technology dependent than phacoemulsification (4,5). We would like to describe our surgical strategies of cataract extraction via a subconjunctival oblique limbus incision (SCOLI) combined with a polymethyl methacrylate (PMMA) PC-IOL implantation for subluxated lens, with zonulysis of ≤120 degree and nuclear sclerosis of grade ≤3 (6).
Methods
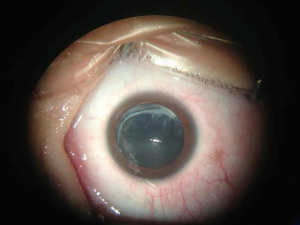
MSICS using PMMA intraocular lens as endocapsular-supporting device was performed in 19 eyes of 14 patients, consisting of 9 males and 5 females. The mean age of males was 49.1±4.6 years with minimum age of 25 to 76 years. The mean age of females was 37.9±7.5 years with minimum age of 35 to 75 years. The cause of subluxation was trauma and idiopathic in 11 eyes and 8 eyes, respectively. All eyes had nuclear sclerosis ≤3. The extent of zonulysis was assessed based on the amount of displacement and/or tilt of the lens as well as its mobility intraoperatively. The lens was decentered in 11 eyes and tilted in 8; 14 eyes had <90 degree of dialysis, and 5 eyes had <120 degree. Preoperative best corrected visual acuity (BCVA) ranged from light perception to 20/60, with visual acuity in 14 eyes <20/200, 5 eyes from 20/200 to 20/60.
Operation methods
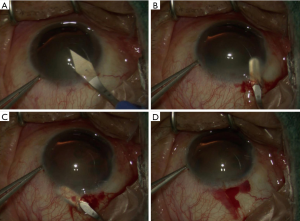
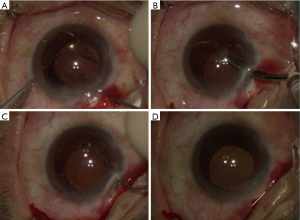
The main incision is constructed in the gradient opposite to the zone of maximum zonular weakness (Figure 1A). A 1.0-mm paracentesis is made at 90 degree to the left side of the main port. A generous amount of highly retentive viscoelastic is placed over the area of zonular dialysis to help tamponade the vitreous through the paracentesis. A subconjunctival limbal tunnel is subsequently created with an angled bevel-up crescent blade (SHARPOINT, USA) (Figure 1B,C). With the technique of SCOLI developed by us, this incision can be performed within the 360 degree of limbus, including at 6 or 3 o’clock (Figure 1D).
A continuous curvilinear capsulorrhexis is created, starting away from the area of dialysis (Figure 2A). An oval-shaped capsulorhexis with a diameter of 5.0×6.0 mm was made using a forceps (Figure 2B,C,D).
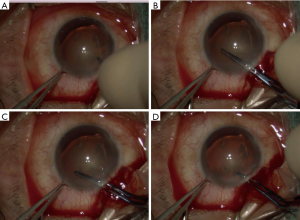
The hydrodissection cannula is inserted in the direction of the zone of disinsertion, until one part of the equator of nucleus is forced out of the capsular rhexis (Figure 3A). Viscoelastic is injected beneath the exposed equatorial region, between the nucleus and the capsular bag, lifting the nuclear as well as expanding and stabilizing the capsular bag (Figure 3B). A vectis may be passed into the anterior chamber and under the half-dislocated nucleus (Figure 3C). Using toothed forceps to grasp the side incision and rotate the eye downward a little, the bulk of the nucleus can then be lifted and drawn into the tunnel using downward pressure of the ‘heel’ of the vectis, and the nucleus is delivered in whole (Figure 3D).
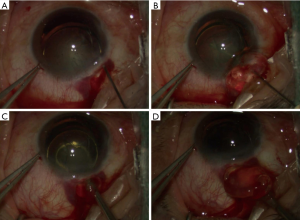
A single-piece PMMA lens (13.0 mm diameter, 6 mm optic, model C55, AMO) is implanted in the bag, orienting the haptics in whichever axis is vertical to the zonular dialysis (Figure 4A). Manually aspirate cortex with a Simcoe cannula in a tangential stripping motion instead of radially to limit stress on zonules (Figure 4B). Additional cortical is removed by careful rotation of PC-IOL (Figure 4C,D). A short-acting intracameral miotic is instilled to confirm centration at conclusion of the procedure (Figure 5).
Results
Depending on the site of zonulysis, the wound was constructed superiorly (9 eyes), temporally (7 eyes) or inferiorly (3 eyes). Intraoperative extension of the dialysis did not occur in any eye. The IOL was placed in the bag in all but 1 case, in which dislocation of the IOL haptic into the vitreous occurred, and one site trans-scleral suture fixation of IOL was carried out. All eyes had endocapsular PC IOL during surgery. Visual acuity was ≥20/40 in 15 of 19 eyes at 6 months of follow up, in 11 of 16 eyes at 1 year of follow up. The IOL de-centration of >1 mm and tilt of >15 degree was not noticed in any case up to at least 6 months following up. Though the IOL was slightly decentered in some cases, it kept stable. All patients were asymptomatic (Figure 6).
Discussion
With the development of newer techniques and devices, subluxated cataracts can be effectively managed by both phacoemulsification and MSICS (2-4). When a foldable, acrylic IOL is used, an endocapsular support devices like CTR, is usually necessary to improve intraoperative capsular support for safer cataract removal (5). In developing countries such as China, however, this adjunctive surgical device is expensive and not always available. Using PMMA PC-IOL as endocapsular supporting device, we performed successfully in some cases with mild-moderate zonular loss.
In our strategy, the main incision should be placed in the gradient opposite to the zone of maximum zonular weakness to help reduce stress on the existing zonules. Moreover, if the zonular dehiscence is located at the incision site, lens placement is more difficult. With the SCOLI technique, the main incision can be easily performed in the gradient opposite to the zone of maximum zonular weakness. For example, in cases of zonular loss between 9 and 12 o’clock, it can be done between 3 and 6 clock, facilitated by rotating the head of the patient and adjusting sitting position of the operator (8).
Compared to central continuous curvilinear capsulorrhexis (CCCC), a decentered-oval-shaped capsulorhexis opening owns four advantages: firstly, an eccentric rhexis is easily performed in the area absent of zonular supporting. Secondly, an oval capsular opening facilitate prolapse the nucleus out of the bag. Thirdly, a larger (2–3.0 mm) margin between the capsulorhexis edge and the equator ensure the IOL haptic staying in bag. Fourthly, a larger margin in the area of zonular loss helps to restrict the turbulence in the bag and prevented vitreous lose during cortex clean up. Therefore, an intact eccentric rhexis in oval shape presents the most essential and challenging step in ectopia lentis in our procedures.
In this approach, the nucleus is prolapsed out of the bag and then out of the tunnel as a whole, followed by cortical aspiration using manual aspiration. During these procedures, a minimal flow or irrigation is used, giving the procedure advantage over phacoemulsification (9).
In our approach, the IOL is inserted prior to the cortical clean up. In eyes with less than 4 clock hours of zonular loss, this endocapsular-implanted IOL will ensure stretching of the bag and provide sufficient stability and lens centration. Furthermore, the tautness of the bag provides countertraction facilitating cortical aspiration at zone of disinsertion. We noted difficulty in performing the aspiration of cortical matter where the PMMA IOL haptical is placed. It is helpful to rotate the PC-IOL prior to aspiration of cortex.
Unfortunately, our procedure meets difficult in cases of severe subluxation (>120), or larger grade of nucleus (≥4). This is due to the following disadvantages: In the presence of largely compromised zonules, there is more difficulty in creating a large capsular opening, which is a prerequisite to prolapse the nucleus out of bag. Moreover, the denser nuclei are usually hard to get out of the bag, making the surgery more challenging. In addition, placement of PC-IOL into the capsular bag is challenging when there is significant zonular weakness, since one must achieve IOL centration, and maximize long-term stability. In these cases, some form of augmented capsule support devices will likely be helpful (10,11).
Using endocapsular flexible PMMA ring helps to prevent iatrogenic loss of zonular support, minimizing vitreous loss (8). In our procedures, the use of endocapsular PMMA IOL has enabled surgeons to achieve these objectives and approaches. In our experience, capsular bag retention is possible in 100% cases in subluxated cases with zonulysis of ≤90 degree and in 90% cases of zonulysis of ≤120 degree. The rigid IOL help minimize the chance of capsular contraction and decentration in the long term. In summary, we could achieve in-the-bag implantation in most eyes of patients presenting with minimal—moderate lens subluxation. This may present an alternative method for dealing with ectopia lentis cases.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.05.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by IRB of The First People’s Hospital of Yunnan Province (No. 2016031). Informed consent was taken from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Blecher MH, Kirk MR. Surgical strategies for the management of zonular compromise. Curr Opin Ophthalmol 2008;19:31-5. [Crossref] [PubMed]
- Chee SP, Jap A. Management of traumatic severely subluxated cataracts. Am J Ophthalmol 2011;151:866-71.e1. [Crossref] [PubMed]
- Hoffman RS, Snyder ME, Devgan U, et al. Management of the subluxated crystalline lens. J Cataract Refract Surg 2013;39:1904-15. [Crossref] [PubMed]
- Cionni RJ, Osher RH. Endocapsular ring approach to the subluxed cataractous lens. J Cataract Refract Surg 1995;21:245-9. [Crossref] [PubMed]
- Vasavada AR, Praveen MR, Vasavada VA, et al. Cionni ring and in-the-bag intraocular lens implantation for subluxated lenses: a prospective case series. Am J Ophthalmol 2012;153:1144-53.e1. [Crossref] [PubMed]
- Yang J, Lai P, Wu D, et al. Manual cataract extraction via a subconjunctival limbus oblique incision for mature cataracts. Indian J Ophthalmol 2014;62:274-8. Erratum in: Indian J Ophthalmol 2014;62:679. [Crossref] [PubMed]
- Lai PH, Yang J, Han F. Operation procedure of a 45-year-old man with blunt injury of left eye. Asvide 2018;5: 545. Available online: http://www.asvide.com/article/view/25262
- Ma X, Li Z. Capsular tension ring implantation after lens extraction for management of subluxated cataracts. Int J Clin Exp Pathol 2014;7:3733-8. [PubMed]
- Goel R, Kamal S, Kumar S, et al. Feasibility and Complications between Phacoemulsification and Manual Small Incision Surgery in Subluxated Cataract. J Ophthalmol 2012;2012:205139.
- Tribus C, Alge CS, Haritoglou C, et al. Indications and clinical outcome of capsular tension ring (CTR) implantation: A review of 9528 cataract surgeries. Clin Ophthalmol 2007;1:65-9. [PubMed]
- Assia EI, Ton Y, Michaeli A. Capsule anchor to manage subluxated lenses: initial clinical experience. J Cataract Refract Surg 2009;35:1372-9. [Crossref] [PubMed]
Cite this article as: Lai PH, Yang J, Han F. Using a rigid lens as endocapsular supporting device in cataract surgery for moderate subluxated cataracts. Ann Eye Sci 2018;3:29.