The Handan Offspring Myopia Study (HOMS): an overview
Background
In China, the prevalence of myopia in the Chinese adult (40 years or older) population in both the urban (Beijing) and rural area (Handan) is similar (approximately 20%) (1,2). However, the prevalence of myopia and the average refractive error in 15-year-old children in urban China (Guangzhou) is 78.4% and −1.50D, respectively (3), which is significantly greater than that found in children of the same age residing in rural China (Yangxi, a rural area located west of Guangzhou) (43.0% and −0.50D respectively) (4). These data provide strong evidence that the lifestyle and exposure to environmental factors is different in the younger generation in rural versus that of urban China (5,6). Hence, the Handan Offspring Myopia Study (HOMS) was conducted between March and June 2010 to determine the prevalence of myopia among the offspring of the Handan Eye Study (HES), with focus on the generational shift in refractive error within families (7).
The HES, in Handan, Hebei province, northern China, was a population-based eye study in adults ≥30 years (8). The prevalence of myopia was 18.8% (2). In order to determine the prevalence of myopia among the offspring of the HES, the HOMS was conducted between March and June 2010, with focus on the generational shift in refractive error within families.
Study population
The target population of HOMS was from the 6 villages in the Yongnian County of Handan, Hebei province, northern China. All children aged 6–18 years, with at least one parent who was included in the HES, were included. The HES was a population-based eye study in adults ≥40 years, with 18.8% of the prevalence of myopia.
Main ocular examinations
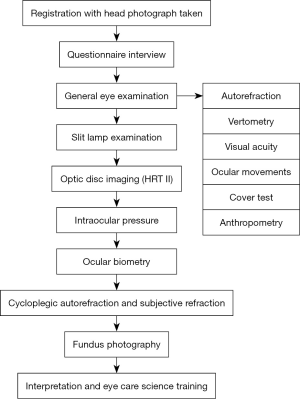
The main ocular examinations included intraocular pressure (Perkins), optic disc imaging [Heidelberg Retina Tomograph (HRT)], axial length (A-scan), cycloplegic (cyclopentolate 1%) autorefraction/subjective refraction, and fundus photography. A detailed questionnaire was also performed. The detailed examination flow of HOMS was presented below (Figure 1). Of 1,238 eligible individuals, 878 children (70.9%; 52.6% male) from 541 families were recruited. Mean age of the children was 10.5±2.5 years.
Major findings
1 diopter (D) of generational myopic shift
Refractive error difference (RED) was defined as the difference between the parental spherical equivalence (SE) and their children’s SE. Generational myopic shift was defined as the estimated RED between the children’s SE and the parental SE when a child would be 18 years old according to a prediction model. The RED (median, quartiles) increased from −1.33 (−1.99, −0.98) D in children aged 6 to 7 years to 0.81 (−0.16, 2.28) D in children aged 16 to 17 years. The children’s SE was predicted to approach the parental SE at 14 years of age. Moreover, the children’s estimated myopic shift would be 1.03 D at 18 years old. Multiple linear regression revealed that older children (beta =0.23 D/y, P<0.0001) and girls (beta =0.24, P=0.01) tended to have a higher RED (9).
There is approximately 1 D of generational myopic shift in rural area, which is approximately 1 D less than that in urban area found in Beijing Myopia Progression Study (BMPS) (6). These myopic trends suggested a predominantly increased exposure to environmental factors between the 2 generations in the last 3 to 4 decades after China ended the Cultural Revolution and a formal education system was put in place.
A weak protective effect of the outdoor activity on myopia
The overall time spent on near work and outdoor activity in the children was 4.8±1.6 and 2.9±1.4 h per day, respectively. Myopic children spent more time on near work (5.0±1.7 vs. 4.7±1.6 h, P=0.049), while no significant difference was found in outdoor activity hours (2.8±1.3 vs. 3.0±1.4 h, P=0.38), as compared to non-myopic children. In the multiple logistic analysis, no association between near work and myopia was found after adjusting for the children’s age, gender, parental refractive error, parental educational level, and daily outdoor activity hours [odds ratio (OR) 1.10, 95% confidence interval (CI), 0.94–1.27]. However, a weak protective effect of the outdoor activity on myopia was found (OR 0.82, 95% CI, 0.70–0.96), after adjusting for similar confounders (10).
These results were inconsistent with Xichang Pediatric Refractive Error Study (X-PRES) in southern rural China (age range, 5–13 years) (11), or in BMPS (age range, 6–17 years) (12). The inconsistent findings may be attributed to the different living environments between rural and urban areas, or between northern and southern areas. Further studies are warranted.
A modest protective effect of the eye exercises of acupoints on myopia
Chinese traditional “eye exercises of acupoints” have been advocated as a compulsory measure to reduce visual symptoms, as well as to retard the development of refractive error, among Chinese students for decades. The exercises are comprised of a 5-min, bilateral eye acupoint self-massage. The participants in the HOMS were asked to complete the eye exercises and vision questionnaire, the convergence insufficiency symptom survey (CISS) questionnaire. In this study, we found only 14.5% of the rural students performed the eye exercises of acupoints in school. The multiple OR and 95% CI for those having a “serious attitude” towards performing the eye exercises (0.12, 0.03–0.49) demonstrated a protective effect for myopia, after adjusting for the children's age, gender, average parental refractive error, and the time spent on near work and outdoor activity. The more frequently, and the more seriously, the students performed the eye exercises each week, the less likely was their chance of being myopic (OR 0.17, 95% CI, 0.03–0.99), after adjusting for the same confounders (13).
These results were also inconsistent with our previous studies on urban students, where we did not find the associations between the eye exercises of acupoints and myopia (13). This could be due to a dose effect of the eye exercises of acupoints for myopia. In the current study, the rural students who performed the eye exercises in school had less myopic refractive error as compared to the urban students (−0.40 vs. −1.70 D).
Summary
The HOMS is the first offspring eye study in a Chinese population. The study design is based on another representative study, HES. In this study, we found 1 D of generational myopic shift, a weak protective effect of the outdoor activity on myopia, and a modest protective effect of the eye exercises of acupoints on myopia, among the rural children in the northern area.
Acknowledgments
Funding: This study is funded by Wenzhou Medical University R&D Fund (No. QTJ13009), and Zhejiang Province Health Innovation Talents Fund (No. 2016025).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ian G. Morgan, Xiaohu Ding and Xinxing Guo) for the series “Managing Myopia in East Asia Myopia Crisis” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.09.02). The series “Managing Myopia in East Asia Myopia Crisis” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Xu L, Li J, Cui T, et al. Refractive error in urban and rural adult Chinese in Beijing. Ophthalmology 2005;112:1676-83. [Crossref] [PubMed]
- Liang YB, Wong TY, Sun LP, et al. Refractive errors in a rural Chinese adult population the Handan eye study. Ophthalmology 2009;116:2119-27. [Crossref] [PubMed]
- He M, Zeng J, Liu Y, et al. Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci 2004;45:793-9. [Crossref] [PubMed]
- He M, Huang W, Zheng Y, et al. Refractive error and visual impairment in school children in rural southern China. Ophthalmology 2007;114:374-82. [Crossref] [PubMed]
- Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet 2012;379:1739-48. [Crossref] [PubMed]
- Liang YB, Lin Z, Vasudevan B, et al. Generational difference of refractive error in the baseline study of the Beijing Myopia Progression Study. Br J Ophthalmol 2013;97:765-9. [Crossref] [PubMed]
- Gao TY, Zhang P, Li L, et al. Rationale, design, and demographic characteristics of the handan offspring myopia study. Ophthalmic Epidemiol 2014;21:124-32. [Crossref] [PubMed]
- Liang YB, Friedman DS, Wong TY, et al. Rationale, design, methodology, and baseline data of a population-based study in rural China: the Handan Eye Study. Ophthalmic Epidemiol 2009;16:115-27. [Crossref] [PubMed]
- Lin Z, Gao TY, Vasudevan B, et al. Generational difference of refractive error and risk factors in the handan offspring myopia study. Invest Ophthalmol Vis Sci 2014;55:5711-7. [Crossref] [PubMed]
- Lin Z, Gao TY, Vasudevan B, et al. Near work, outdoor activity, and myopia in children in rural China: the Handan offspring myopia study. BMC Ophthalmol 2017;17:203. [Crossref] [PubMed]
- Lu B, Congdon N, Liu X, et al. Associations between near work, outdoor activity, and myopia among adolescent students in rural China: the Xichang Pediatric Refractive Error Study report no. 2. Arch Ophthalmol 2009;127:769-75. [Crossref] [PubMed]
- Lin Z, Vasudevan B, Mao GY, et al. The influence of near work on myopic refractive change in urban students in Beijing: a three-year follow-up report. Graefes Arch Clin Exp Ophthalmol 2016;254:2247-55. [Crossref] [PubMed]
- Lin Z, Vasudevan B, Jhanji V, et al. Eye exercises of acupoints: their impact on refractive error and visual symptoms in Chinese urban children. BMC Complement Altern Med 2013;13:306. [Crossref] [PubMed]
Cite this article as: Liang YB, Lin Z, Gao TY. The Handan Offspring Myopia Study (HOMS): an overview. Ann Eye Sci 2018;3:48.