
Anti-vascular endothelial growth factor and macular atrophy: an unanswered question
Does anti-vascular endothelial growth factor (VEGF) therapy lead to geographic atrophy? If so, does the number of injections or the duration of anti-VEGF therapy correlate with the risk of developing geographic atrophy? With intravitreal injections becoming the most common ophthalmic invasive procedure and an increasingly aging population, these questions really matter.
Anti-VEGF therapy has become a revolution in the treatment of vascular retinal disease. Although the therapy is easy to apply and safe, the drugs involved have been shown to cause many side effects. These side effects are either caused by the intravitreal injection procedure or by the drugs themselves. The former are associated with elevation of IOP, intravitreal hemorrhage, and inflammation or retinal detachment, whereas the latter are associated with myocardial infarction, thromboembolic events, stroke, hypertension, and gastrointestinal bleeding (1,2). In our paper, we have showed that anti-VEGF treatment of type 1 choroidal neovascularization (CNV) leads to abnormalization of the choroidal neovascular membranes, which become more dense and develop more branches, thereby becoming more complex (3). We know that anti-VEGF therapy can cause macular atrophy (MA) when used for a long duration; however, most studies including an analysis of the inhibition of VEGF in age-related choroidal neovascularisation (IVAN) trial data have been done only with 2 years of follow-up (4).
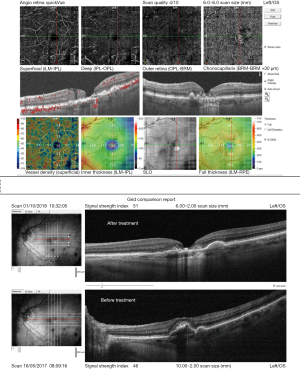
In the IVAN trial, 1.25 mg bevacizumab and 0.5 mg ranibizumab were injected under either a continuous (every month) or a discontinuous (as needed) regimen over a 2-year period. The primary outcome was best corrected visual acuity (BCVA) at 2 years of follow-up, and the results showed that there was no significant difference in BCVA between both the agents and the regimens. Recently, an image grading analysis of the IVAN trial data was performed to evaluate the progression of MA during anti-VEGF therapy in a study and the fellow eye. The most important finding was that there was no correlation between the incidence and progression of MA over the study period and the number of injections. This result was contrary to those reported by CATT and the previous IVAN studies. However, 24.4% and 1.54% of the eyes undergoing treatment over a period of 2 years were found to develop intralesional and extralesional MA, respectively. Moreover, the authors found a negative correlation between the presence of pigment epithelial detachment at the final visit and development of MA. This new finding highlights the need to assess the types of neovascularization as classic CNV at baseline was found to be a protective factor preventing the development or progression of MA within the lesion. Detecting atrophy among CNV lesions can be a challenge as the tissues are already affected Figure 1.
It is possible that sub-RPE neovascularization creates resistance to MA. The presence of atrophy both in and out of the CNV lesion in the fellow eye was found to be a risk factor for MA in the study eye at the end of a visit.
Despite approximately 1/4th of the eyes developing intralesional MA, no visual impairment was observed. It may be reasonable to think that patients can develop eccentric viewing or that visual acuity measurement is more subjective than multimodal image grading.
It is worth noting that the previously published IVAN results showed a higher percentage of MA, i.e., more than 30%. Detecting atrophy among CNV lesions can be a challenge as the tissues are already affected. So, in the recent evaluation of the IVAN trial data, the authors used altered criteria for the diagnosis of MA; in the CATT and previous IVAN studies, the diagnosis of MA was based on the presence of MA regardless of its location, whereas in the new evaluation of the IVAN trial data, the study group divided MA based on its location as intralesional (5,6).
The issue of the development of MA during anti-VEGF treatment was studied in the CATT trial with a maximum follow-up period of 5 years. The results showed an increase in the incidence of MA with the increase in year as follows: 12% at 1 year, 17% at 2 years, and 38% at 5 years. The risk factors included advanced age, hypercholesterolemia, lower BCVA, larger CNV area, type 3 CNV lesion, MA in the fellow eye, and the presence of intraretinal fluid. Patients with a thicker subretinal lesion and the presence of subretinal fluid were less likely to develop MA (7).
This multicenter, long-term study showed that there was an increase in the incidence of MA with anti-VEGF treatment. Its main shortcoming was the relatively short follow-up period of only 24 months. Moreover, the authors showed no significant decrease in BCVA which can be a result of confounding factors rather than reality.
Discrepancies between the results of 2015 IVAN trial and results of reevaluation of the trial data might be due to the different methodologies used. During the reevaluation, the authors utilized more strict criteria for the detection of MA. Moreover, they used a multimodal approach, i.e., they used color fundus photography, fluorescein angiography, and optical coherence tomography (OCT), to identify MA. Furthermore, there was a senior grader who supervised all the diagnoses.
It is understandable that physicians and patients are concerned about the side effects of intravitreal drugs. After all, every drug causes some side effects. However, it would be unwise not to mention the extreme benefits that anti-VEGF therapy provided to patients with neovascular AMD or that no significant decrease in BCVA was found over 2 years of treatment of MA.
We also advocate not to prolong the anti-VEGF treatment over 1 year when there is only subretinal fluid, as it may lead to MA. This is especially important because the presence of subretinal fluid with the lack of intraretinal fluid was shown to lower the risk of MA as this may indicate the existence of functional blood-retinal barrier.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Eye Science. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.11.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Schmid MK, Bachmann LM, Fäs L, et al. Efficacy and adverse events of aflibercept, ranibizumab and bevacizumab in age-related macular degeneration: a trade-off analysis. Br J Ophthalmol 2015;99:141-6. [Crossref] [PubMed]
- Falavarjani KG, Nguyen QD. Adverse events and complications associated with intravitreal injection of anti-VEGF agents: a review of literature. Eye (Lond) 2013;27:787-94. [Crossref] [PubMed]
- Wylęgała A, Wylęgała F, Wylęgała E. Aflibercept Treatment Leads to Vascular Abnormalization of the Choroidal Neovascularization. J Healthc Eng 2018;2018:8595278 [Crossref] [PubMed]
- Bailey C, Scott LJ, Rogers CA, et al. Intralesional Macular Atrophy in Anti-Vascular Endothelial Growth Factor Therapy for Age-Related Macular Degeneration in the IVAN Trial. Ophthalmology 2019;126:75-86; [PubMed]
- Martin DF, Maguire MG, Ying GS, et al. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med 2011;364:1897-908. [Crossref] [PubMed]
- Chakravarthy U, Harding SP, Rogers CA, et al. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet 2013;382:1258-67. [Crossref] [PubMed]
- Grunwald JE, Pistilli M, Daniel E, et al. Incidence and Growth of Geographic Atrophy during 5 Years of Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology 2017;124:97-104. [Crossref] [PubMed]
Cite this article as: Wylęgała A, Wylęgała E. Anti-vascular endothelial growth factor and macular atrophy: an unanswered question. Ann Eye Sci 2018;3:61.


