
An intensive and personalised care planning programme improves clinical outcomes in patients with diabetic retinopathy: a pilot randomised controlled trial
Introduction
Landmark trials have demonstrated that optimal glycaemic, blood pressure (BP) and lipid control reduces the risk of progression of diabetic retinopathy (DR), a common microvascular complication of diabetes (1,2). Good diabetes control is, however, alarmingly low in Singaporeans with diabetes and DR, with 82.6% and 89.7% not meeting the recommended glycaemic and BP control thresholds, respectively (3). Barriers to optimal diabetes control are multifactorial which includes poor self-efficacy, fragmented care, patient’s reluctance to ask questions to their diabetes care providers, and difficulty reconciling contradictory health information (4). Accordingly, an evidence-based, patient-centred strategy to address poor diabetes control is needed.
A recent meta-analysis showed that patient-centred interventions in those with diabetes conferred improvements in glycaemic control compared to usual care, especially when they were comprehensive, intensive, and integrated into routine care (5). However, as most studies were conducted in Caucasian patients, findings may not be generalisable to Asian populations due to differences in healthcare systems, cultural, religious and environmental habits, people’s perceptions to illness, and disease coping mechanisms (6). In addition, very few patient-centred personalised interventions have aimed to improve diabetes outcomes in those with microvascular complications such as DR, and related study findings have been equivocal (7,8).
We conducted a pilot randomised controlled trial (RCT) to test the effectiveness of a novel DR-specific intensive and personalised care planning (DR-IPCP) programme on improving glycated haemoglobin (HbA1c, primary outcome), BP and lipids (secondary outcomes). DR-IPCP involved personalised physician consultations and DR-specific behaviour change sessions conducted by DR specialist nurse educators using patients’ own retinal images. We hypothesised that DR-IPCP would be effective in improving diabetes control parameters in patients with type 2 diabetes and mild-moderate DR over three months, compared to usual care (UC).
Methods
English-speaking patients of Chinese, Malay or Indian ethnicity aged ≥21 years with type 2 diabetes, mild-moderate DR, and poor glycaemic control [HbA1c ≥64 mmol/mol (≥8.0%) over two consecutive readings] were recruited from retinal clinics at the Singapore National Eye Centre between 2015 and 2016. Participants with hearing or cognitive impairment [ascertained using the 6 item Cognitive Impairment Test (9)] were excluded. The study was approved by the SingHealth Centralised Institutional Review Board (#1199/5/2015) and written consent was obtained from each participant. The study was conducted according to the tenets of the Declaration of Helsinki.
Participants were randomly assigned to UC or the DR-IPCP intervention using concealed allocation. UC participants received routine care from their primary and tertiary care providers and were advised to seek medical support from a diabetes nurse educator or hospital physician per standard care protocol.
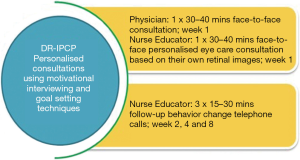
DR-IPCP was designed based on the Health Change Australia methodology (10), an innovative patient-centred behaviour change strategy grounded in evidence-based psychological theories and principles including Motivational Interviewing (11), Theory of planned behaviour (12), Social Cognition Theory (13), and Transtheoretical Model (14). The intervention involved continuous and active conversations between the participant, personalised care-trained physician and diabetes nurse educator with the aim of establishing a mutual understanding on an individualised treatment regimen (Figure 1).
All participants underwent a baseline assessment of diabetes history, prior diabetes education, and self-reported medical conditions. HbA1c and lipid [total (TC), low and high -density lipoprotein cholesterol (LDL/HDL); and triglyceride (TG)] values were obtained from patients’ case records, if available in the past 6 months; otherwise venipuncture was performed. Systolic and diastolic BP (in mmHg) was assessed once using a digital sphygmomanometer. DR in the worse eye was graded from 2-field fundus images using the Early Treatment Diabetic Retinopathy Study Scale (15). Blood and BP parameters were collected again at three months post-intervention. Finally, telephone interviews were conducted with DR-IPCP participants to obtain feedback about the intervention using both open-ended questions about their experience and a question rated on five-point Likert scale ranging from ‘Satisfied’ to ‘Not at all satisfied’.
Statistical analyses were performed using STATA version 10 (StataCorp LP., College Station, TX, USA). Within-group and between-group means were compared using Paired t-tests and ANOVA, respectively; and medians were compared using Mann-Whitney’s U-test. Within-group proportions were compared using the Chi-square test or Fisher’s exact test and between-group proportions were compared using Wilcoxon signed-rank test. Statistical significance was set at 5%. Satisfaction levels of DR-IPCP participants were measured using proportions.
Results
Eighteen patients (9= UC and 9= DR-IPCP) completed the study [mean age (standard deviation) (SD) =61 (14.83) years; 56% (n=10) female]. Twelve (67%) and 6 (33%) patients had mild and moderate DR, respectively (Table 1). There were no differences in age, gender, DR severity or diabetes control parameters at baseline (all P>0.05) between the DR-IPCP and UC groups.
Table 1
| Parameters | DR-IPCP | P value (WG) | Control | P value (WG) | P value |
|---|---|---|---|---|---|
| Age (years) | 59.22 (11.53) | 62.55 (18.13) | 0.647 | ||
| Gender (female) | 5 (55.56) | 5 (55.56) | 1.000 | ||
| DR type | 1.000 | ||||
| Mild NPDR | 6 (66.67) | 6 (66.67) | |||
| Moderate NPDR | 3 (33.33) | 3 (33.33) | |||
| Outcomes | |||||
| HbA1c (mmol/mol; %) | 0.032# | 0.771 | 0.068* | ||
| B | 81; 9.63 (1.13) | 85; 9.97 (1.19) | |||
| F | 73; 8.85 (0.95) | 86; 10.07 (1.62) | |||
| TC (mmol/L) | 0.049# | 0.515 | 0.606* | ||
| B | 4.94 (0.99) | 5.43 (1.36) | |||
| F | 4.30 (0.59) | 5.07 (0.50) | |||
| HDL (mmol/L) | 0.077 | 0.656 | 0.271* | ||
| B | 1.30 (0.30) | 1.36 (0.29) | |||
| F | 1.16 (0.29) | 1.33 (0.28) | |||
| LDL (mmol/L) | 0.040# | 0.358 | 0.385* | ||
| B | 2.98 (1.06) | 3.12 (0.69) | |||
| F | 2.22 (0.63) | 2.77 (0.58) | |||
| TG (mmol/L) | 0.795 | 0.636 | 0.740* | ||
| B | 2.05 (1.28) | 1.92 (1.57) | |||
| F | 2.12 (1.11) | 2.19 (1.00) | |||
| SBP (mmHg) | 0.190 | 0.756 | 0.381* | ||
| B | 142.75 (25.10) | 136.85 (16.18) | |||
| F | 134.87 (15.55) | 135.42 (15.16) | |||
| DBP (mmHg) | 0.393 | 0.320 | 0.630* | ||
| B | 71.37 (10.28) | 71.85 (13.65) | |||
| F | 69.62 (9.10) | 68.28 (9.19) |
Values are n (%) for categorical variables and mean (SD) for numerical variables. *P value between groups. #indicate statistical significance (P<0.05). B, baseline; F, follow-up; WG, within group; DR-IPCP, diabetic retinopathy-specific, intensive, and personalised care planning; NPDR, non-proliferative diabetic retinopathy; HbA1c, glycated haemoglobin; TC, total cholesterol; HDL, high density lipoprotein; LDL, low density lipoprotein; TG, triglycerides; SBP, systolic blood pressure; DBP, diastolic blood pressure.
In the DR-IPCP group, there were significant within-group reductions in HbA1c, TC, and LDL between baseline and follow-up [7 mmol/mol (−0.8%), −0.64 mmol/L, −0.66 mmol/L, respectively, P<0.05; Table 1]. There were however no significant changes in any of the study parameters in the UC group. While the observed within-group reduction in HbA1c in DR-IPCP participants was greater than in UC participants, this between-group difference was non-significant [7 mmol/mol (−0.8%), vs. 1 mmol/mol (+0.1%), respectively; P=0.068, Table 1].
DR-IPCP participants reported a clear understanding of their diabetes management and how diabetes control was linked with their own DR after the intervention, e.g., “From the retinal photos, I could see if my eye disease is getting worse or not”; “I know more about the food restrictions than before. I did not know I should eat wholemeal bread”; and “I learnt to reduce low sugar incidents at night”. Overall, 91% reported being ‘satisfied’ with the intervention.
Discussion
Our DR-specific, intensive, and personalised intervention resulted in short-term significant improvements in HbA1c, TC, and LDL in patients with early DR and poor glycaemic control in the intervention group alone. No between-group effects were observed, however, likely due to the small sample size. Given the high level of patient satisfaction with DR-IPCP and the fact that the intervention can be delivered by trained nurse educators, an integration into existing healthcare systems to complement routine eye care appears feasible. However, larger, longer-term RCTs to test the effectiveness of DR-IPCP on a range of clinical, behavioural, patient-centred, and economical outcomes are needed.
Our 7 mmol/mol (−0.8%) reduction in HbA1c is similar to an Australian RCT of patients in type 2 diabetes and mild-moderate DR (16). However, our results differ from a large US study which found no improvement in HbA1c or diabetes self-management practices at 1-year following an estimate of the participant’s risk of DR progression and a structured diabetes education program (7), highlighting the difficulty of sustained optimal diabetes control and the importance of incorporating behaviour change strategies into education interventions.
In contrast to several studies in patients with type 2 diabetes with more intensive and long term interventions (17,18), we found no significant within- or between-group reductions in BP following the DR-IPCP intervention although the intervention group had an absolute mean reduction of 7.88 mmHg. Our patients’ baseline SBP [mean (SD) =142 (Jeny25) mmHg] and DBP [mean (SD) =71 (Jeny10) mmHg] values were however relatively low, limiting its potential for further improvement.
Strengths of our study include its RCT design, a thorough clinical assessment, and a structured personalized behaviour change intervention tailored to support patients to achieve optimal diabetes control. If successful, the intervention could be adapted for other microvascular complications, such as diabetic nephropathy and neuropathy, and scaled up across primary care settings. However, there are several limitations to acknowledge. First, our pilot intervention was short-term, leading to only transient behavioural changes, and the sustainability of results is not known. Second, our small sample size limited our power to detect significant between-group effects. Third, we did not assess other key diabetes management behaviours, such as medication adherence, a healthy eating plan, regular physical activity, blood glucose-monitoring and diabetes self-care. Fourth, DR-IPCP was implemented in English- and Mandarin-speaking patients only. However, with diabetes prevalence highest amongst Malays (17.1%) and Indians (21.6%) in Singapore, our results may not be generalisable. Fifth, we restricted our patient sample to those with mild-moderate DR as targeting patients with early disease may be most successful given that preventative action is possible to avoid disease progression (19); thus, it is unclear if this intervention would benefit those with severe DR. Finally, we did not measure the intervention’s effect on DR progression outcomes or DR-specific QoL, nor did we assess its cost-effectiveness compared to UC.
Whilst our results are promising, they need to be replicated in a large, adequately powered, and multi-ethnic RCT to understand the long-term clinical, ocular, cognitive, behavioural, psychosocial, and economic effectiveness of DR-IPCP, and we have been funded by the Singapore National Medical Research Council (#HSRG-DB17nov001) to undertake this important work. If successful, this novel approach may be a key step in personalising care for the Asian population living with poorly controlled type 2 diabetes and preventing the development of vision-threatening DR.
Acknowledgments
Funding: This study was supported by Singapore Health Services Pte Ltd. Prof Ecosse L. Lamoureux received the funding under the SingHealth Research Strategic Hires Scheme, STH-1202-SERI. The grant body had no roles in design, conduct or data analysis of the study.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2019.10.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the SingHealth Centralised Institutional Review Board (#1199/5/2015) and written consent was obtained from each participant. The study was conducted according to the tenets of the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- ACCORD Study Group. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med 2010;363:233-44. [Crossref] [PubMed]
- O'Connor PJ, Ismail-Beigi F. Near-Normalization of Glucose and Microvascular Diabetes Complications: Data from ACCORD and ADVANCE. Ther Adv Endocrinol Metab 2011;2:17-26. [Crossref] [PubMed]
- Huang OS, Lamoureux EL, Tay WT, et al. Glycemic and blood pressure control in an asian malay population with diabetes and diabetic retinopathy. Arch Ophthalmol 2010;128:1185-90. [Crossref] [PubMed]
- Nam S, Chesla C, Stotts NA, et al. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract 2011;93:1-9. [Crossref] [PubMed]
- Coulter A, Entwistle VA, Eccles A, et al. Personalised care planning for adults with chronic or long-term health conditions. Cochrane Database Syst Rev 2015;CD010523 [PubMed]
- Li L, Yang Y, He J, et al. Emotional suppression and depressive symptoms in women newly diagnosed with early breast cancer. BMC Womens Health 2015;15:91. [Crossref] [PubMed]
- Aiello LP, Ayala AR, Antoszyk AN, et al. Assessing the Effect of Personalized Diabetes Risk Assessments During Ophthalmologic Visits on Glycemic Control: A Randomized Clinical Trial. JAMA Ophthalmol 2015;133:888-96. [Crossref] [PubMed]
- Wagner H, Pizzimenti JJ, Daniel K, et al. Eye on diabetes: a multidisciplinary patient education intervention. Diabetes Educ 2008;34:84-9. [Crossref] [PubMed]
- Upadhyaya AK, Rajagopal M, Gale TM. The Six Item Cognitive Impairment Test (6-CIT) as a screening test for dementia: comparison with Mini-Mental State Examination (MMSE). Curr Aging Sci 2010;3:138-42. [Crossref] [PubMed]
- Gale J, Skouteris H. Health Coaching. Faciliting health behaviour change for chronic condition prevention and self-management. In: Caltabiano ML, Ricciardelli L, editors. Applied Topics in Health Psychology. John Wiley and Sons; 2013.
- Rollnick S Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. Guilford Publications; 2007.
- Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckman J, eds. Action-control: from cognition to behavior. Heidelberg: Springer; 1985.
- Bandura A. Self-Efficacy: The Exercise of Control. New York. W.H. Freeman and Company; 1997.
- Prochaska JO, DiClemente CC. The transtheoretcial approach: Crossing traditional boundaries of therapy. Homewood, Ill. 1984.
- . Grading diabetic retinopathy from stereoscopic color fundus photographs--an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1991;98:786-806. [Crossref] [PubMed]
- Rees G, Lamoureux E, Nicolaou T, et al. Feedback of personal retinal images appears to have a motivational impact in people with non-proliferative diabetic retinopathy and suboptimal HbA1c: findings of a pilot study. Diabet Med 2013;30:1122-5. [Crossref] [PubMed]
- Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003;348:383-93. [Crossref] [PubMed]
- Rothe U, Muller G, Schwarz PE, et al. Evaluation of a diabetes management system based on practice guidelines, integrated care, and continuous quality management in a Federal State of Germany: a population-based approach to health care research. Diabetes Care 2008;31:863-8. [Crossref] [PubMed]
- Milne S, Sheeran P, Orbell S. Prediction and intervention in health-related behaviour: a meta-analytic review of protection motivation theory. J Appl SocPsychol 2000;30:106-43. [Crossref]
Cite this article as: Aravindhan A, Fenwick EK, Man REK, Tee AA, Lamoureux EL. An intensive and personalised care planning programme improves clinical outcomes in patients with diabetic retinopathy: a pilot randomised controlled trial. Ann Eye Sci 2020;5:3.


