
Focal alteration of the intraretinal layers in neurodegenerative disorders
Background
With the advent of optical coherence tomography (OCT) in the 1990s (1,2), the evolved image resolution and robust segmentation of the intraretinal layers in volumetric data allowed for detailed analysis of retinal structure (3,4). The most widely used segmentation involves the following layers: retinal nerve fiber layer (RNFL) (5,6), which contains unmyelinated axons, ganglion cell-inner plexiform layer (GCIPL), which contains retinal ganglion cell (RGC) bodies (7,8), and the ganglion cell complex (GCC), which includes RNFL and GCIPL (9). Though definitions vary in different OCT devices, these retinal layers have been suggested to be structural image biomarkers, which have been used in monitoring disease progression and aiding in diagnostics of neurodegenerative diseases (5,10,11). The majority of these published studies used the average thickness of certain areas such as the macula. However, the distribution of the neural fiber and ganglion cells in the retina is not even (12-16). For example, using Zeiss OCT, nasal and superior quadrants of GCIPL are thicker compared to the temporal and inferior quadrants in normal healthy subjects (12). Furthermore, the uneven distribution of the intraretinal layers has been demonstrated in normal healthy subjects using ultra-high-resolution OCT (UHR-OCT) and commercial segmentation software (Orion software) (13,14,16). Moreover, based on previous histological studies, there is a selective vulnerability of RGCs to various neurodegenerative disorders (17). Parasol RGCs and related magnocellular pathways are more involved in the pathogenesis of Alzheimer’s disease (AD) (18). The parasol RGCs are usually located in the peripheral retina. More interestingly, the prominent Aβ deposition has been demonstrated in the superior-temporal quadrant in flat-mounted retinas (18). Patients with AD had inferior visual field loss (17,18). The midget RGCs and the parvocellular pathway, located in the papillomacular bundle (center of the macula), are more involved in mitochondrial optic neuropathy (19,20). Hence, the commonly used average thickness of these intraretinal layers may not be sensitive enough to reveal the focal thickness alterations (21-24), which limits further improvement of these neural biomarkers in diagnostic powers.
Because of the limitations of the thickness parameters averaged from the area, further analysis of sectional areas has been applied (25-27). Sectional thickness analysis using arbitrary partitions, such as the Early Treatment Diabetic Retinopathy Study (ETDRS) partition, hemisphere partition (16) and Zeiss elliptical partition (21), appears to improve the refinement of thickness alterations and provides a better understanding of the pathologic locations. The improved analysis further strengthens the establishment of correlations between neurodegeneration and clinical manifestations, which provides better biomarkers for monitoring treatment efficacy in clinical trials (25-27). However, some studies have pointed out that these arbitrary partition methods often define the sections of RNFL and GCIPL, which may not be sufficient to observe early change, especially focal thickness reduction, which may not fall into any predefined partition (13,14,16,28). Hence, beyond the traditional partition method, some studies used the freedom of self-defined regions of interest (ROI) to describe the focal thickness alteration change in neurodegenerative diseases in an attempt to find important associations with clinical manifestations such as visual acuity, visual field, contrast sensitivity and disability (14,25,29,30). However, without direct visualization of the thickness map alteration, exploration of the most profound alteration may miss the target, although the relations between the thickness of the ROI and clinical manifestations may provide some critical information.
In this review, we summarize focal thickness alterations in different regions of the intraretinal layers in normal aging and several central nervous system neurodegenerative diseases, which involve slow progressive loss of neurons in the central nervous system, such as AD and Parkinson’s disease (PD). Current literature involving focal alterations in the intraretinal layers were reviewed through PubMed using the search terms “focal alteration”, “region of interest”, “optical coherence tomography” with “glaucoma”, “multiple sclerosis”, “Alzheimer’s disease”, “Parkinson disease”, “neurodegenerative diseases” and other related items. The clinical implications of these focal thickness alterations and future research directions were discussed.
Thickness mapping and visualization of the intraretinal layers
The most commonly used OCT devices in the clinic provide thickness maps of the GCIPL, GCC and peripapillary RNFL (pRNFL) (5,31,32). The benefits of these approaches are their availability and ease of assessment, which do not require further processing of the OCT scans for further interpretation. The drawbacks are as follows: First, clinical reports of OCT scans do not provide thickness information on other intraretinal layers. Second, the visualization is often limited to each scan and cannot be averaged for further visualization of a group of eyes. Third, the preset partitions, such as the Zeiss elliptical partition and ETDRS partition, cannot be modified, which limits redefining the ROI for detecting focal thickness alterations.
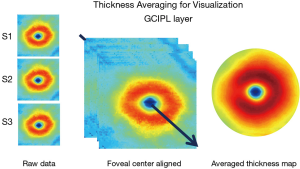
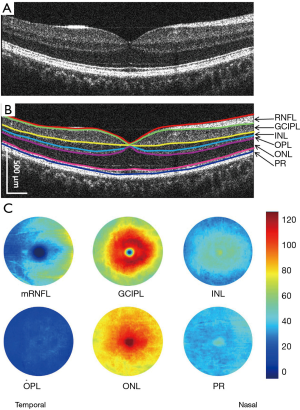
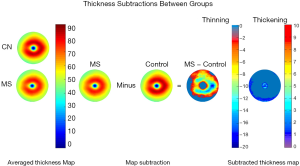
The advancement of retinal segmentation provides a solution to the automated segmentation of the intraretinal layers, which opens the door for visualization of the thickness maps. Chen et al. reported three-dimensional segmentation, which can segment the retina into 11 intraretinal layers and creates a visualization of these segmented layers (3,33). Furthermore, using commercially available segmentation software (Orion, Voxeleron LLC, Pleasanton, CA, USA), up to seven layers can be segmented in the three-dimensional dataset (13-15,34). To visualize the thickness maps of the intraretinal layers for a special group, averaging of each thickness map is required with access to the raw segmented thickness data. Mwanza et al. reported a GCIPL thickness map averaged from 47 normal eyes to demonstrate the thickness contour about the fovea (12). Generating the average thickness requires alignment of the foveal center as an alignment landmark (Figure 1). Of note, the study by Mwanza et al. only segmented the GCIPL and demonstrated the uneven distribution of GCIPL in normal eyes (12). Similar approaches were conducted by our group using UHR-OCT and Orion software (13-16) (Figure 2). These studies segmented six intraretinal layers and visualized focal thickness alterations in patients with AD (15) and multiple sclerosis (MS) (13,14) by calculating the difference of the average thickness maps between the diseased eyes and normal controls (Figure 3). This approach provides a practical method of searching for more sensitive structural biomarkers in neurodegenerative disorders (13-15). The Orion software has been adapted in commercial OCT devices such as Zeiss Cirrus HD-OCT (with special data exportation) (35,36), Topcon 3D-1000 (Topcon Medical Systems, Inc., Oakland, NJ, USA) (34) and Spectralis SD-OCT (Heidelberg Engineering, Heidelberg, Germany) (37). It could be speculated that the visualization of focal thickness alterations can be performed using these commercial OCT devices and the Orion software (34-37).
With these recent developments in OCT and segmentation, focal thickness alterations in the intraretinal layers may help determine the most vulnerable region during aging and in certain neurodegenerative diseases, including glaucoma, Leber’s hereditary optic neuropathy (LHON), MS and its related optic neuritis (ON), mild cognitive impairment (MCI), AD and PD (Table 1). The focal thickness reduction zone in the intraretinal layers generally may represent the area that is most seriously affected by certain diseases. These characteristic patterns may also provide disease-specific information and better discrimination powers (38,41,42).
Table 1
| Authors | Disease | No. of eyes | OCT device | Analysis tool | Thinning pattern | AUC | Map |
|---|---|---|---|---|---|---|---|
| Hu |
Multiple sclerosis with optic neuritis |
30 |
Custom-built UHR-OCT | Orion software | U zone | 0.97 | |
| Shi |
Multiple sclerosis without optic neuritis |
47 patients |
Custom-built UHR-OCT | Orion software | M zone | 0.77 | |
| Lee |
Glaucoma |
67 |
Cirrus HD-OCT | Built-in software | Temporal raphe sign | 0.811 | |
| Chen |
Preperimetric glaucoma |
67 |
SD-OCT | Built-in software | Inferotemporal | 0.784 | |
| Lee |
Ethambutol-induced optic neuropathy |
28 |
Cirrus SD-OCT | Built-in software | Inferonasal | 0.833 | |
| Sharifipour |
Glaucoma |
101 |
Cirrus HD- OCT | Built-in software | Inferotemporal | 0.944 | |
| Yum |
Optic chiasmal compression by a pituitary adenoma |
46 |
Cirrus HD-OCT | Built-in software | Inferonasal, superonasal | 0.965, 0.958 | |
| Shao |
Alzheimer’s disease |
25 |
Custom-built UHR-OCT | Orion software | Inner superior | – | |
| Mild cognitive impairment |
24 |
Custom-built UHR-OCT | Orion software | Outer superior | – | ||
| Shin |
Primary open-angle glaucoma | 292 | Cirrus HD-OCT | MATLAB software | Inferotemporal region (250°–339°) at 2.08 mm from the fovea | – | |
| Balducci |
Acute Leber’s hereditary optic neuropathy |
6 |
Cirrus HD-OCT | Built-in software | Superonasal | 0.9545 | |
| Acute Leber’s hereditary optic neuropathy |
6 |
Cirrus HD-OCT | Built-in software | Inferonasal, superonasal | 1.0, 1.0 | ||
| Cheung |
Alzheimer’s disease |
100 |
Cirrus HD-OCT | Built-in software | Inferior | 0.722 | |
| Mild cognitive impairment |
41 |
Cirrus HD-OCT | Built-in software | Inferotemporal | 0.688 |
GCIPL, ganglion cell-inner plexiform layer; OCT, optical coherence tomography; AUC, area under the curve; UHR-OCT, ultra-high-resolution OCT; S, superior; I, inferior; ST, superotemporal; SN, superonasal; IT, inferotemporal; IN, inferonasal; II, inner inferior; IS, inner superior; OS, outer superior; OT, outer temporal; ON, outer nasal; OI, outer inferior.
Normal aging
Aging increases the likelihood of neurodegeneration in the brain and retina. Age plays a role in the onset of AD, PD, and other neurodegenerative diseases (45). Studying the effect of age on the intraretinal layers improves our understanding of neurodegeneration during normal aging and disease-related retinal morphology changes. The alteration of the intraretinal layers during aging has been well-studied, and annual decline rates provide a reference for disease conditions (46-51). Many OCT studies have reported age-related thickness alteration of the retinal neural layers (46-51). In a study with 121 subjects, the pRNFL was found to decrease by 0.37 µm/year with the greatest decrease in the lower quadrant (0.58 µm) (46). Hammel et al. found that the mean rate of average GCIPL thickness reduction was 0.57 µm/year (47), whereas the average decline rate of the macular GCIPL thickness was reported as 0.12 µm/year in another study (48). In previous studies, Harwerth et al. suggested that 15% of RNFL thickness loss, 50% loss of axons and 40% reduction of axon density in RFNL can occur in a 70-year lifespan (52). Wei et al. reported that, during a period of six decades, the RNFL was 0.35% (0.13 µm) thinning per year and 0.21% (0.14 µm) per year in the GCIPL layer (53). A longitudinal study showed that, over 40 years, the ganglion cells defined as GCC thickness decreased 0.25 µm per year and RNFL decreased 0.21 µm per year (54). Previous studies showed that the inner annulus (IA) part of macular GCIPL was most correlated with age (49-51) (Wang JH, et al., IOVS 201;59: ARVO, E-Abstract 1102). Because the Zeiss elliptical partition mainly covers the IA of the retina, all sectors showed reduced thickness with age (12,48). The variation of the annual thinning rates is mainly due to the differences of the measurement areas of the unevenly distributed intraretinal layers. Other factors to explain the variations include different study cohorts and different OCT devices and segmentation methods.
In contrast to the thinning of the inner retinal layers, age-related thickening was found in some sublayers of the outer retina. Several studies found the thicknesses of the outer plexiform layer (OPL), outer photoreceptor segment (OS), and photoreceptor complex (PR) were positively correlated with age (51,53). This finding can be illustrated by histopathological studies because the density of cone and RPE cells showed no significant loss in the fovea of the eye. Furthermore, the accumulation of residual bodies and loss of melanin granules were found in the retinal pigment epithelium-Bruch’s membrane (RPE-BM) (55,56). These age-related intraretinal layer thickness changes may be mainly due to selective loss of neurons and axons with aging, as found in histology studies (57,58).
Glaucoma
Glaucoma, a leading cause of visual impairment, is a group of diseases with multifactorial etiology defined by atypical optic neuropathy accompanying structural damage of RGCs and their axons, resulting in visual field damage and blindness (59,60). Accurate diagnosis is crucial for vision preservation (60). However, it is difficult to differentiate between glaucomatous optic neuropathy (GON) and nonglaucomatous optic neuropathy (NGON) even for a well-trained ophthalmologist (61). Thus, alterations in focal intraretinal layer thickness are useful in diagnosis, and clinical management.
The evolution of OCT with better resolution, faster scanning speed, and advanced imaging patterns improves the reliability of OCT measurements (62). However, in advanced stages of glaucoma, RNFL thinning has a “floor effect”, which may not be sensitive enough to monitor the disease progression (62). Meanwhile, current OCT structural parameters cannot provide differential structural measurements between normal and early glaucomatous eyes (62). OCT-measured pRNFL thickness has been found to have the ability to differentiate between normal and glaucomatous eyes (62,63).
In addition to the thickness measurement of the RNFL, the macular GCIPL layer is another way to monitor glaucomatous progression and detect early glaucoma (38,64). Early involvement and progressive damage of RGCs occurs in both GON and NGON (38,64). Chen et al. found that thickness reduction in the inferior temporal (IT) sector in the Zeiss elliptical partition had the largest discrimination power [area under the receiver operator curve (AUROC) =0.794] to differentiate preperimetric glaucoma eyes from normal eyes (39). Sharifipour et al. reported that the same IT thinning pattern in the Zeiss elliptical partition had an AUROC of 0.944 to detect eyes with early glaucoma (41). These measurements mentioned above were based on commercial OCT with built-in thickness analysis.
By using custom-built retinal thickness measurement software and an improved analysis algorithm, some typical OCT image biomarkers were found (29,43). By subtracting the average RNFL and GCIPL thicknesses of normal eyes from glaucoma eyes, Hood et al. found a pattern located at the inferior area associated with greater visual field loss, which may represent greater vulnerability of the inferior retinal region (29). Using OCT Guided Progression Analysis (GPA) in GCIPL analysis, Shin et al. found a similar area located in the IT region (250°–339°) at 2.08 mm from the fovea, which had the most frequent GCIPL thinning (43). Lee et al. found a temporal raphe sign of GCIPL that can be used to differentiate glaucomatous from nonglaucomatous GCIPL thinning (38).
LHON and visual pathway pathology
A specific pattern of retinal thickness layer reduction was also found in LHON, a subacute neurodegenerative blinding disorder characterized by selective loss of RGCs (19). Balducci et al. found that the natural progression of LHON followed a specific pattern of reduction in macular GCIPL located in the inferior nasal pattern (44). The specific pattern changes in macular GCIPL in LHON may indicate that the papillomacular bundle is primarily involved in LHON. The thinning pattern of GCIPL thickness of LHON follows a centrifugal and spiral pattern in line with the anatomic distribution of the papillomacular bundle fibers (44,65). Specifically, nasal focal thinning of GCIPL at the presymptomatic stage before the diffuse thinning of GCIPL was observed in LHON (44).
MS and its related ON
MS is an autoimmune neurodegenerative disorder affecting the central nervous system (66). Eighty percent of patients with longstanding MS also experience deficits in visual function (67). ON is an inflammatory optic neuropathy that affects many patients with MS at some point during their disease progression (68). OCT is regarded as an alternative to magnetic resonance imaging (MRI) for monitoring MS (69). Thinning of the pRNFL and GCIPL measured by OCT is considered as an ocular biomarker of the central nervous system in MS (70,71). The thickness reductions of pRNFL and GCIPL have been used in MS clinical trials (5,72). However, although the thickness reductions of pRNFL and GCIPL were significant among groups of patients with MS without a history of optic neuritis (MSNON), MS with a history of ON (MSON) and matched normal controls had longitudinal changes of these neuronal layers of ~1 µm per year. This poses difficulty in following up on disease severity and therapeutic efficacy (5,23), which inspired the exploration of more sensitive retinal structural markers for monitoring neurodegeneration compared to the average thickness reduction of pRNFL and GCIPL. Detailed analysis of focal thickness alteration may meet the challenge.
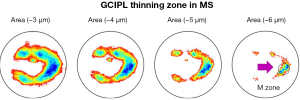
Shi et al. used UHR-OCT and automatic segmentation software to visualize topographic thickness alterations of intraretinal thickness in patients with relapsing-remitting MS without a history of ON (14). The visualized thickness map of GCIPL showed a profound thickness reduction zone, named “M Zone”, short of the “MS thinning Zone of the GCIPL” (Figure 4). It was a circling zone located at nasal ~2 mm and inferior 0.42 mm from the fovea. The “M zone” was found to be the most profound alteration compared to any sectors partitioned using the ETDRS partition. The discrimination power (AUROC =0.75) was second to pRNFL (AUROC =0.79) in differentiating eyes with MS and no ON. Furthermore, the focal thickness alteration in the M Zone had good correlation with MS-related disability and visual dysfunctions. The authors suggested that the focal thinning zone (i.e., the M Zone) can be an imaging biomarker to monitor neurodegeneration in patients with MS. The finding also echoes the thinning of temporal pRNFL compared to other zones in MS patients without ON (73). It is also consistent with previous histological studies reporting midget RGCs and the parvocellular pathway located in the papillomacular bundle, which are more selectively damaged (18,74,75).
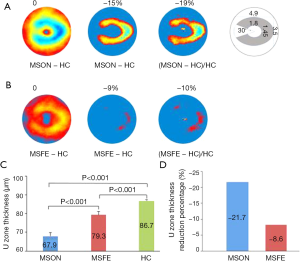
For the MS diagnosis, there is another challenge in that subclinical ON often occurs but is difficult to diagnose. Current imaging diagnostic criteria include lesions of the brain and spine but not the optic nerve. Clinical and subclinical ON are highly prevalent during the MS disease course (76-78), and image markers for ON are under development. A recent study suggested that inter-eye differences in pRNFL and GCIPL thicknesses can identify a history of unilateral ON, which may add the diagnosis of ON. However, inter-eye difference has only moderate differential power at 70% to identify ON from healthy control subjects (10,22,24). Visualization and quantitative analysis of the intraretinal layers may help define the most profound thinning zone in MS patients with ON eyes. Hu et al. used the same method used in the study by Shi et al. (14) to visualize the changes in thickness maps and reported a horseshoe-like thinning zone named the “U Zone” in macular GCIPL in MS patients with ON (Figure 5) (13). The GCIPL thickness alteration in the “U Zone” had the greatest differential power (AUROC =0.97) to identify MS patients with ON eyes from normal eyes. The intereye difference in the “U Zone” had a differential power at 0.85 to identify ON eyes from healthy control eyes (8). The discovery of the “M zone” and “U zone” indicates that detailed analysis of thickness maps may provide a better understanding of eye degeneration and could further improve the diagnostic power of MS-related ON. The established relationships of these focal thickness alterations and clinical manifestations demonstrate their value in the clinical management of neurodegenerative disorders.
MCI and AD
The most common form of dementia in elderly people is AD (79). Neurodegeneration due to AD usually occurs decades before clinically detectable cognitive function decline (80). The transitional phase between normal cognition and AD is MCI. Patients with MCI can maintain their independent normal life, and ~15% MCI transfers to AD (80). Monitoring cerebral neurodegeneration may provide information on disease onset and progression. Brain MRI and positron emission tomography are the main tools but are expensive, sometimes invasive and time-consuming (81,82). The retina is an extension of the brain, and neurodegenerative progress in the retina may reflect neurodegenerative progress in the brain. OCT has been used for a long time to noninvasively measure the thickness of retinal neural layers, including RNFL and GCIPL, which are also used as biomarkers to monitor AD progress (31).
Recent meta-analysis studies revealed that thinning RNFL occurs in patients with MCI and/or AD (83,84). The Rotterdam Study found that thinner RNFL was associated with a higher risk of dementia in subsequent years (85). The thinning of RNFL was also related to worse MRI variables in the volume of hippocampus, global cingulum and posterior thalamic radiations (86). The GCIPL in patients with AD and MCI was also thinner compared with that of normal subjects (32,87,88). Using the Zeiss elliptical partition method, Cheung et al. found that the IT sector was the most affected region in patients with MCI but an inferior sector in patients with AD (32). Choi et al. used the Zeiss elliptical partition and drew a similar conclusion that the IT sector was thinner than other sectors in patients with MCI (87). Shao et al. used custom UHR-OCT and automated retinal segmentation software to visualize the topographic thickness maps of the intraretinal layers (15). More interestingly, by subtracting the GCIPL layer in cognitively normal subjects from that in MCI patients and AD patients, a focal thickness reduction was found in the superior outer region in patients with MCI and the superior inner region in AD using the ETDRS partition (15). This focal thickness reduction was more profound compared to any other sectors based on the Zeiss elliptical partition method. The findings are in agreement with previous histological studies that the peripheral retina, mainly containing parasol RGCs in the magnocellular pathway, is more involved in AD. Inferior visual field loss was also evident in patients with AD, and prominent Aβ deposition was found in the superior temporal quadrant in flat-mount retinas from patients with AD (89). However, whether the focal thinning in the superior quadrant was more related to disease onset and progression compared to average thickness reduction at the inferior quadrant needs to be further confirmed in future studies.
PD
PD is a neurodegenerative disease that presents mainly with tremor, rigidity, akinesia and postural instability (90) due to selective dopamine neuron damage (91). Visual impairments such as decreased contrast sensitivity, visual acuity and impaired color vision often occur in patients with PD (92,93). A recent meta-analysis study showed thinning of pRNFL and GCIPL (94). Changes in the thickness of the intraretinal layers in PD may result from decreased dopamine (95) and accumulation of pathologic alpha-synuclein deposits in the retina (96).
Furthermore, the thinning of pRNFL mainly occurred in the inferior sector, followed by the superior sector (94). Sari et al. reported that the thicknesses of all sectors in the Zeiss elliptical partition of GCIPL in patients with PD were significantly lower than normal healthy controls (97). Bayhan et al. also found that average GCIPL, superior GCIPL, and inferior GCIPL were thinner in patients with PD compared with those in normal healthy subjects (98). Both studies found that the thickness of the inferior sector of GCIPL was correlated with disease duration and severity (97,98). Therefore, the inferior sector of GCIPL has the potential to be an imaging biomarker to monitor disease severity and duration. However, the alteration of the thickness map of GCIPL in patients with PD was not visualized in these previous studies.
Conclusions
In conclusion, we have summarized focal thickness changes of the intraretinal layers in some ocular and cerebral neurodegenerative disorders. These focal alterations in the intraretinal layers appear to provide better differential power and stronger correlations with clinical manifestations compared with those of the traditional partition method. Future longitudinal and large sample studies are needed.
Acknowledgments
Funding: The work was supported by the National Multiple Sclerosis Society (RG-1506-04890), NIH Center Grant P30 EY014801, NINDS 1R01NS111115-01 (Wang), and a grant from Research to Prevent Blindness (RPB).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Fiona Costello and Steffen Hamann) for the series “The Use of OCT as a Biomarker in Neuro-ophthalmology” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2019.12.04). The series “The Use of OCT as a Biomarker in Neuro-ophthalmology” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science 1991;254:1178-81. [Crossref] [PubMed]
- Fujimoto J, Swanson E. The Development, Commercialization, and Impact of Optical Coherence Tomography. Invest Ophthalmol Vis Sci 2016;57:1-13. [PubMed]
- Sonka M, Abramoff MD. Quantitative analysis of retinal OCT. Med Image Anal 2016;33:165-9. [Crossref] [PubMed]
- Kafieh R, Rabbani H, Kermani S. A review of algorithms for segmentation of optical coherence tomography from retina. J Med Signals Sens 2013;3:45-60. [Crossref] [PubMed]
- Petzold A, Balcer LJ, Calabresi PA, et al. Retinal layer segmentation in multiple sclerosis: a systematic review and meta-analysis. Lancet Neurol 2017;16:797-812. [Crossref] [PubMed]
- Seibold LK, Mandava N, Kahook MY. Comparison of retinal nerve fiber layer thickness in normal eyes using time-domain and spectral-domain optical coherence tomography. Am J Ophthalmol 2010;150:807-14. [Crossref] [PubMed]
- Saidha S, Al-Louzi O, Ratchford JN, et al. Optical coherence tomography reflects brain atrophy in multiple sclerosis: A four-year study. Ann Neurol 2015;78:801-3. [Crossref] [PubMed]
- Shin JW, Sung KR, Lee GC, et al. Ganglion Cell-Inner Plexiform Layer Change Detected by Optical Coherence Tomography Indicates Progression in Advanced Glaucoma. Ophthalmology 2017;124:1466-74. [Crossref] [PubMed]
- Kim NR, Kim JH, Lee J, et al. Determinants of perimacular inner retinal layer thickness in normal eyes measured by Fourier-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2011;52:3413-8. [Crossref] [PubMed]
- Xu SC, Kardon RH, Leavitt JA, et al. Optical coherence tomography is highly sensitive in detecting prior optic neuritis. Neurology 2019;92:e527-35. [Crossref] [PubMed]
- Ko F, Muthy ZA, Gallacher J, et al. Association of Retinal Nerve Fiber Layer Thinning With Current and Future Cognitive Decline: A Study Using Optical Coherence Tomography. JAMA Neurol 2018;75:1198-205. [Crossref] [PubMed]
- Mwanza JC, Durbin MK, Budenz DL, et al. Profile and predictors of normal ganglion cell-inner plexiform layer thickness measured with frequency-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2011;52:7872-9. [Crossref] [PubMed]
- Hu H, Jiang H, Gameiro GR, et al. Focal thickness reduction of the ganglion cell-inner plexiform layer best discriminates prior optic neuritis in patients with multiple sclerosis. Invest Ophthalmol Vis Sci 2019;60:4257-69. [Crossref] [PubMed]
- Shi C, Jiang H, Gameiro GR, et al. Visual Function and Disability Are Associated With Focal Thickness Reduction of the Ganglion Cell-Inner Plexiform Layer in Patients With Multiple Sclerosis. Invest Ophthalmol Vis Sci 2019;60:1213-23. [Crossref] [PubMed]
- Shao Y, Jiang H, Wei Y, et al. Visualization of Focal Thinning of the Ganglion Cell-Inner Plexiform Layer in Patients with Mild Cognitive Impairment and Alzheimer's Disease. J Alzheimers Dis 2018;64:1261-73. [Crossref] [PubMed]
- Tan J, Yang Y, Jiang H, et al. The measurement repeatability using different partition methods of intraretinal tomographic thickness maps in healthy human subjects. Clin Ophthalmol 2016;10:2403-15. [Crossref] [PubMed]
- La Morgia C, Ross-Cisneros FN, Sadun AA, et al. Retinal Ganglion Cells and Circadian Rhythms in Alzheimer's Disease, Parkinson's Disease, and Beyond. Front Neurol 2017;8:162. [Crossref] [PubMed]
- La Morgia C, Di Vito L, Carelli V, et al. Patterns of Retinal Ganglion Cell Damage in Neurodegenerative Disorders: Parvocellular vs Magnocellular Degeneration in Optical Coherence Tomography Studies. Front Neurol 2017;8:710. [Crossref] [PubMed]
- Carelli V, Ross-Cisneros FN, Sadun AA. Mitochondrial dysfunction as a cause of optic neuropathies. Prog Retin Eye Res 2004;23:53-89. [Crossref] [PubMed]
- Yu-Wai-Man P, Griffiths PG, Chinnery PF. Mitochondrial optic neuropathies - disease mechanisms and therapeutic strategies. Prog Retin Eye Res 2011;30:81-114. [Crossref] [PubMed]
- Mwanza JC, Oakley JD, Budenz DL, et al. Macular ganglion cell-inner plexiform layer: automated detection and thickness reproducibility with spectral domain-optical coherence tomography in glaucoma. Invest Ophthalmol Vis Sci 2011;52:8323-9. [Crossref] [PubMed]
- Nolan RC, Galetta SL, Frohman TC, et al. Optimal Intereye Difference Thresholds in Retinal Nerve Fiber Layer Thickness for Predicting a Unilateral Optic Nerve Lesion in Multiple Sclerosis. J Neuroophthalmol 2018;38:451-8. [Crossref] [PubMed]
- Nolan-Kenney RC, Liu M, Akhand O, et al. Optimal intereye difference thresholds by optical coherence tomography in multiple sclerosis: An international study. Ann Neurol 2019;85:618-29. [Crossref] [PubMed]
- Coric D, Balk LJ, Uitdehaag BMJ, et al. Diagnostic accuracy of optical coherence tomography inter-eye percentage difference for optic neuritis in multiple sclerosis. Eur J Neurol 2017;24:1479-84. [Crossref] [PubMed]
- Hood DC, Xin D, Wang D, et al. A Region-of-Interest Approach for Detecting Progression of Glaucomatous Damage With Optical Coherence Tomography. JAMA Ophthalmol 2015;133:1438-44. Erratum in: Error in Byline [JAMA Ophthalmol 2016]. [Crossref] [PubMed]
- Birkeldh U, Manouchehrinia A, Hietala MA, et al. The Temporal Retinal Nerve Fiber Layer Thickness Is the Most Important Optical Coherence Tomography Estimate in Multiple Sclerosis. Front Neurol 2017;8:675. [Crossref] [PubMed]
- Bock M, Brandt AU, Kuchenbecker J, et al. Impairment of contrast visual acuity as a functional correlate of retinal nerve fibre layer thinning and total macular volume reduction in multiple sclerosis. Br J Ophthalmol 2012;96:62-7. [Crossref] [PubMed]
- Kobayashi W, Kunikata H, Omodaka K, et al. Correlation of papillomacular nerve fiber bundle thickness with central visual function in open-angle glaucoma. J Ophthalmol 2015;2015:460918 [Crossref] [PubMed]
- Hood DC, Raza AS, de Moraes CG, et al. The Nature of Macular Damage in Glaucoma as Revealed by Averaging Optical Coherence Tomography Data. Transl Vis Sci Technol 2012;1:3. [Crossref] [PubMed]
- Choi JA, Shin HY, Park HL, et al. The Pattern of Retinal Nerve Fiber Layer and Macular Ganglion Cell-Inner Plexiform Layer Thickness Changes in Glaucoma. J Ophthalmol 2017;2017:6078365 [Crossref] [PubMed]
- Cheung CY, Ikram MK, Chen C, et al. Imaging retina to study dementia and stroke. Prog Retin Eye Res 2017;57:89-107. [Crossref] [PubMed]
- Cheung CY, Ong YT, Hilal S, et al. Retinal ganglion cell analysis using high-definition optical coherence tomography in patients with mild cognitive impairment and Alzheimer's disease. J Alzheimers Dis 2015;45:45-56. [Crossref] [PubMed]
- Chen X, Niemeijer M, Zhang L, et al. Three-dimensional segmentation of fluid-associated abnormalities in retinal OCT: probability constrained graph-search-graph-cut. IEEE Trans Med Imaging 2012;31:1521-31. [Crossref] [PubMed]
- Lamin A, Oakley JD, Dubis AM, et al. Changes in volume of various retinal layers over time in early and intermediate age-related macular degeneration. Eye (Lond) 2019;33:428-34. [Crossref] [PubMed]
- Behbehani R, Abu Al-Hassan A, Al-Salahat A, et al. Optical coherence tomography segmentation analysis in relapsing remitting versus progressive multiple sclerosis. PLoS One 2017;12:e0172120 [Crossref] [PubMed]
- Keller J, Oakley JD, Russakoff DB, et al. Changes in macular layers in the early course of non-arteritic ischaemic optic neuropathy. Graefes Arch Clin Exp Ophthalmol 2016;254:561-7. [Crossref] [PubMed]
- Hecht I, Yeshurun I, Bartov E, et al. Retinal layers thickness changes following epiretinal membrane surgery. Eye (Lond) 2018;32:555-62. [Crossref] [PubMed]
- Lee J, Kim YK, Ha A, et al. Temporal Raphe Sign for Discrimination of Glaucoma from Optic Neuropathy in Eyes with Macular Ganglion Cell-Inner Plexiform Layer Thinning. Ophthalmology 2019;126:1131-9. [Crossref] [PubMed]
- Chen MJ, Yang HY, Chang YF, et al. Diagnostic ability of macular ganglion cell asymmetry in Preperimetric Glaucoma. BMC Ophthalmol 2019;19:12. [Crossref] [PubMed]
- Lee JY, Han J, Seo JG, et al. Diagnostic value of ganglion cell-inner plexiform layer for early detection of ethambutol-induced optic neuropathy. Br J Ophthalmol 2019;103:379-84. [Crossref] [PubMed]
- Sharifipour F, Morales E, Lee JW, et al. Vertical Macular Asymmetry Measures Derived From SD-OCT for Detection of Early Glaucoma. Invest Ophthalmol Vis Sci 2017;58:4310-7. [Crossref] [PubMed]
- Yum HR, Park SH, Park HY, et al. Macular Ganglion Cell Analysis Determined by Cirrus HD Optical Coherence Tomography for Early Detecting Chiasmal Compression. PLoS One 2016;11:e0153064 [Crossref] [PubMed]
- Shin JW, Sung KR, Park SW. Patterns of Progressive Ganglion Cell-Inner Plexiform Layer Thinning in Glaucoma Detected by OCT. Ophthalmology 2018;125:1515-25. [Crossref] [PubMed]
- Balducci N, Savini G, Cascavilla ML, et al. Macular nerve fibre and ganglion cell layer changes in acute Leber's hereditary optic neuropathy. Br J Ophthalmol 2016;100:1232-7. [Crossref] [PubMed]
- Ramanan VK, Saykin AJ. Pathways to neurodegeneration: mechanistic insights from GWAS in Alzheimer's disease, Parkinson's disease, and related disorders. Am J Neurodegener Dis 2013;2:145-75. [PubMed]
- Celebi AR, Mirza GE. Age-related change in retinal nerve fiber layer thickness measured with spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci 2013;54:8095-103. [Crossref] [PubMed]
- Hammel N, Belghith A, Weinreb RN, et al. Comparing the Rates of Retinal Nerve Fiber Layer and Ganglion Cell-Inner Plexiform Layer Loss in Healthy Eyes and in Glaucoma Eyes. Am J Ophthalmol 2017;178:38-50. [Crossref] [PubMed]
- Huo YJ, Guo Y, Li L, et al. Age-related changes in and determinants of macular ganglion cell-inner plexiform layer thickness in normal Chinese adults. Clin Exp Ophthalmol 2018;46:400-6. [Crossref] [PubMed]
- Yoo YJ, Hwang JM, Yang HK. Inner macular layer thickness by spectral domain optical coherence tomography in children and adults: a hospital-based study. Br J Ophthalmol 2019;103:1576-83. [Crossref] [PubMed]
- Demirkaya N, van Dijk HW, van Schuppen SM, et al. Effect of age on individual retinal layer thickness in normal eyes as measured with spectral-domain optical coherence tomography. Invest Ophthalmol Vis Sci 2013;54:4934-40. [Crossref] [PubMed]
- Ooto S, Hangai M, Tomidokoro A, et al. Effects of age, sex, and axial length on the three-dimensional profile of normal macular layer structures. Invest Ophthalmol Vis Sci 2011;52:8769-79. [Crossref] [PubMed]
- Harwerth RS, Wheat JL. Modeling the effects of aging on retinal ganglion cell density and nerve fiber layer thickness. Graefes Arch Clin Exp Ophthalmol 2008;246:305-14. [Crossref] [PubMed]
- Wei Y, Jiang H, Shi Y, et al. Age-Related Alterations in the Retinal Microvasculature, Microcirculation, and Microstructure. Invest Ophthalmol Vis Sci 2017;58:3804-17. [Crossref] [PubMed]
- Zhang X, Francis BA, Dastiridou A, et al. Longitudinal and Cross-Sectional Analyses of Age Effects on Retinal Nerve Fiber Layer and Ganglion Cell Complex Thickness by Fourier-Domain OCT. Transl Vis Sci Technol 2016;5:1. [PubMed]
- Okubo A, Sameshima M, Unoki K, et al. Ultrastructural changes associated with accumulation of inclusion bodies in rat retinal pigment epithelium. Invest Ophthalmol Vis Sci 2000;41:4305-12. [PubMed]
- Okubo A, Rosa RH Jr, Bunce CV, et al. The relationships of age changes in retinal pigment epithelium and Bruch's membrane. Invest Ophthalmol Vis Sci 1999;40:443-9. [PubMed]
- Harman A, Abrahams B, Moore S, et al. Neuronal density in the human retinal ganglion cell layer from 16-77 years. Anat Rec 2000;260:124-31. [Crossref] [PubMed]
- Gao H, Hollyfield JG. Aging of the human retina. Differential loss of neurons and retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 1992;33:1-17. [PubMed]
- Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006;90:262-7. [Crossref] [PubMed]
- Foster PJ, Buhrmann R, Quigley HA, et al. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol 2002;86:238-42. [Crossref] [PubMed]
- O'Neill EC, Danesh-Meyer HV, Kong GX, et al. Optic disc evaluation in optic neuropathies: the optic disc assessment project. Ophthalmology 2011;118:964-70. [Crossref] [PubMed]
- Lavinsky F, Wollstein G, Tauber J, et al. The Future of Imaging in Detecting Glaucoma Progression. Ophthalmology 2017;124:S76-82. [Crossref] [PubMed]
- Mwanza JC, Oakley JD, Budenz DL, et al. Ability of cirrus HD-OCT optic nerve head parameters to discriminate normal from glaucomatous eyes. Ophthalmology 2011;118:241-8.e1. [Crossref] [PubMed]
- Mwanza JC, Durbin MK, Budenz DL, et al. Glaucoma diagnostic accuracy of ganglion cell-inner plexiform layer thickness: comparison with nerve fiber layer and optic nerve head. Ophthalmology 2012;119:1151-8. [Crossref] [PubMed]
- Zehnder S, Wildberger H, Hanson JVM, et al. Retinal Ganglion Cell Topography in Patients With Visual Pathway Pathology. J Neuroophthalmol 2018;38:172-8. [Crossref] [PubMed]
- Browne P, Chandraratna D, Angood C, et al. Atlas of Multiple Sclerosis 2013: A growing global problem with widespread inequity. Neurology 2014;83:1022-4. [Crossref] [PubMed]
- Albrecht P, Ringelstein M, Muller AK, et al. Degeneration of retinal layers in multiple sclerosis subtypes quantified by optical coherence tomography. Mult Scler 2012;18:1422-9. [Crossref] [PubMed]
- Petzold A, Wattjes MP, Costello F, et al. The investigation of acute optic neuritis: a review and proposed protocol. Nat Rev Neurol 2014;10:447-58. [Crossref] [PubMed]
- Sotirchos ES, Saidha S. OCT is an alternative to MRI for monitoring MS - YES. Mult Scler 2018;24:701-3. [Crossref] [PubMed]
- Saidha S, Syc SB, Durbin MK, et al. Visual dysfunction in multiple sclerosis correlates better with optical coherence tomography derived estimates of macular ganglion cell layer thickness than peripapillary retinal nerve fiber layer thickness. Mult Scler 2011;17:1449-63. [Crossref] [PubMed]
- Saidha S, Syc SB, Ibrahim MA, et al. Primary retinal pathology in multiple sclerosis as detected by optical coherence tomography. Brain 2011;134:518-33. [Crossref] [PubMed]
- Petzold A, de Boer JF, Schippling S, et al. Optical coherence tomography in multiple sclerosis: a systematic review and meta-analysis. Lancet Neurol 2010;9:921-32. [Crossref] [PubMed]
- Klistorner A, Sriram P, Vootakuru N, et al. Axonal loss of retinal neurons in multiple sclerosis associated with optic radiation lesions. Neurology 2014;82:2165-72. [Crossref] [PubMed]
- Sadun AA, Bassi CJ. Optic nerve damage in Alzheimer's disease. Ophthalmology 1990;97:9-17. [Crossref] [PubMed]
- La Morgia C, Ross-Cisneros FN, Koronyo Y, et al. Melanopsin retinal ganglion cell loss in Alzheimer disease. Ann Neurol 2016;79:90-109. [Crossref] [PubMed]
- Saidha S, Naismith RT. Optical coherence tomography for diagnosing optic neuritis: Are we there yet? Neurology 2019;92:253-4. [Crossref] [PubMed]
- Balcer LJ. Clinical practice. Optic neuritis. N Engl J Med 2006;354:1273-80. [Crossref] [PubMed]
- Ikuta F, Zimmerman HM. Distribution of plaques in seventy autopsy cases of multiple sclerosis in the United States. Neurology 1976;26:26-8. [Crossref] [PubMed]
- Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011;7:280-92. [Crossref] [PubMed]
- Kirova AM, Bays RB, Lagalwar S. Working memory and executive function decline across normal aging, mild cognitive impairment, and Alzheimer's disease. Biomed Res Int 2015;2015:748212 [Crossref] [PubMed]
- Zhang N, Song X, Zhang Y, et al. An MRI brain atrophy and lesion index to assess the progression of structural changes in Alzheimer's disease, mild cognitive impairment, and normal aging: a follow-up study. J Alzheimers Dis 2011;26:359-67. [Crossref] [PubMed]
- Jack CR Jr, Holtzman DM. Biomarker modeling of Alzheimer's disease. Neuron 2013;80:1347-58. [Crossref] [PubMed]
- den Haan J, Verbraak FD, Visser PJ, et al. Retinal thickness in Alzheimer's disease: A systematic review and meta-analysis. Alzheimers Dement (Amst) 2017;6:162-70. [Crossref] [PubMed]
- Thomson KL, Yeo JM, Waddell B, et al. A systematic review and meta-analysis of retinal nerve fiber layer change in dementia, using optical coherence tomography. Alzheimers Dement (Amst) 2015;1:136-43. [Crossref] [PubMed]
- Mutlu U, Colijn JM, Ikram MA, et al. Association of Retinal Neurodegeneration on Optical Coherence Tomography With Dementia: A Population-Based Study. JAMA Neurol 2018;75:1256-63. [Crossref] [PubMed]
- Méndez-Gómez JL, Pelletier A, Rougier MB, et al. Association of Retinal Nerve Fiber Layer Thickness With Brain Alterations in the Visual and Limbic Networks in Elderly Adults Without Dementia. JAMA Netw Open 2018;1:e184406 [Crossref] [PubMed]
- Choi SH, Park SJ, Kim NR. Macular Ganglion Cell -Inner Plexiform Layer Thickness Is Associated with Clinical Progression in Mild Cognitive Impairment and Alzheimers Disease. PLoS One 2016;11:e0162202 [Crossref] [PubMed]
- Cunha LP, Lopes LC, Costa-Cunha LV, et al. Macular Thickness Measurements with Frequency Domain-OCT for Quantification of Retinal Neural Loss and its Correlation with Cognitive Impairment in Alzheimer's Disease. PLoS One 2016;11:e0153830 [Crossref] [PubMed]
- Koronyo Y, Biggs D, Barron E, et al. Retinal amyloid pathology and proof-of-concept imaging trial in Alzheimer's disease. JCI Insight 2017; [Crossref] [PubMed]
- de Lau LM, Breteler MM. Epidemiology of Parkinson's disease. Lancet Neurol 2006;5:525-35. [Crossref] [PubMed]
- Lotharius J, Brundin P. Pathogenesis of Parkinson's disease: dopamine, vesicles and alpha-synuclein. Nat Rev Neurosci 2002;3:932-42. [Crossref] [PubMed]
- Chaudhuri KR, Healy DG, Schapira AH. Non-motor symptoms of Parkinson's disease: diagnosis and management. Lancet Neurol 2006;5:235-45. [Crossref] [PubMed]
- Ming W, Palidis DJ, Spering M, et al. Visual Contrast Sensitivity in Early-Stage Parkinson's Disease. Invest Ophthalmol Vis Sci 2016;57:5696-704. [Crossref] [PubMed]
- Chrysou A, Jansonius NM, van Laar T. Retinal layers in Parkinson's disease: A meta-analysis of spectral-domain optical coherence tomography studies. Parkinsonism Relat Disord 2019;64:40-9. [Crossref] [PubMed]
- Harnois C, Di PT. Decreased dopamine in the retinas of patients with Parkinson's disease. Invest Ophthalmol Vis Sci 1990;31:2473-5. [PubMed]
- Ortuño-Lizarán I, Beach TG, Serrano GE, et al. Phosphorylated alpha-synuclein in the retina is a biomarker of Parkinson's disease pathology severity. Mov Disord 2018;33:1315-24. [Crossref] [PubMed]
- Sari ES, Koc R, Yazici A, et al. Ganglion cell-inner plexiform layer thickness in patients with Parkinson disease and association with disease severity and duration. J Neuroophthalmol 2015;35:117-21. [PubMed]
- Bayhan HA, Aslan BS, Tanik N, et al. The association of spectral-domain optical coherence tomography determined ganglion cell complex parameters and disease severity in Parkinson's disease. Curr Eye Res 2014;39:1117-22. [Crossref] [PubMed]
Cite this article as: Airen S, Shi C, Liu Z, Levin BE, Signorile JF, Wang J, Jiang H. Focal alteration of the intraretinal layers in neurodegenerative disorders. Ann Eye Sci 2020;5:8.


