
Optical coherence tomography in compressive lesions of the anterior visual pathway
Introduction
Optical coherence tomography (OCT) has revolutionized the clinical management of retinal and optic nerve disease. The strict anatomical structure of the retina and maintenance of retinotopic organization within the afferent visual pathway means that OCT is also relevant to central nervous system disease.
OCT allows objective segmental analysis of the retinal layers at the macula. The retinal ganglion cell (RGC) layer can be measured at the macula and the RGC axons can be measured as the retinal nerve fiber layer (RNFL) at the optic nerve. These RGC axons form into the optic nerve, traverse the optic chiasm and synapse at the lateral geniculate ganglion whilst strictly conforming to retinotopic organization. Compression of these axons anterior to the geniculate synapses can cause retrograde changes to the RGCs which can be quantified with OCT. As axons are more compact in the anterior visual pathway than the visual cortex, lesions affecting the anterior regions can cause substantial loss of visual function.
Compression of the anterior visual pathway most commonly occurs at the level of the optic chiasm. Mass lesions affecting this area include pituitary macroadenomas, craniopharyngiomas, Rathke’s cysts and aneurysms of the internal carotid and ophthalmic arteries. However, compression can also occur from other lesions including meningiomas of the tuberculum sella (and contiguous structures) and metastases. Within the orbit, compression can occur from infiltrative neoplastic lesions, optic nerve sheath meningiomas, systemic inflammatory conditions (i.e., ANCA positive disease or sarcoid), or the enlarged muscles of thyroid eye disease.
The anatomical changes on OCT and their relationship to visual function in patients with anterior visual pathway compression is explored in this review. The role of OCT as a prognosticator for visual recovery after treatment of these compressive lesions, is also detailed.
OCT as an ocular imaging technique
OCT is a non-invasive method of structurally assessing microscopic damage to RGCs and their axons by performing high-resolution cross-sectional imaging of macula and peripapillary retinal tissue. Low-coherence near-infrared light is transmitted to the retina and the magnitude and echo time delay of backscattered light from the retina is measured to construct a cross-sectional, three-dimensional, real-time tomographic retinal image. Time domain OCT has axial resolution up to 10 µm and scanning speeds of 400 A-scans per second. Spectral domain OCT is a more current technology with digital axial resolution of 4–6 µm and scan speeds of 50,000–85,000 A-scans per second. The techniques of OCT are explored in more detail in the ‘Overview of OCT’ in this focused issue.
OCT measurements are compared to a normative database but these comparisons do not necessarily consider age, sex, or race variables as Caucasian middle-aged subjects make up the bulk of the normative population. Ocular variables such as long or short axial length and optic disc area also alter RNFL measurements. Intraocular disease can hinder the accuracy of OCT such as media opacities, coexistent retinal disease, and other optic disc abnormalities like drusen. Machine factors such as segmentation inaccuracies and scan quality need to be scrutinized to minimize measurement error. Different OCT machines such as Spectralis (Heidelberg, Germany), Cirrus (Zeiss, Germany) and RS-3000 (Nidek, Japan) have different measurement protocols, so patients need to be reviewed on the same machine using the same scanning protocol for accurate comparisons over time.
OCT patterns of change with compressive lesions of the anterior visual pathway
Based on the specific anatomical course of RGC axons, compressive lesions along the anterior visual pathway can create certain predictable patterns on OCT. These patterns can sometimes detect visual pathway compression that may not be initially apparent on neuroimaging, or by standard ophthalmic assessments.
Axons at the level of the RNFL do not cross the horizontal meridian. The nerve fibers originating in the nasal hemiretina directly enter the nasal optic nerve. The macula, which lies temporal to the optic disc, has the highest density of RGCs which direct their axons through the “papillomacular bundle”. The remaining axons of the temporal retina approach the optic disc by curving around the papillomacular bundle and thus are compressed into the superotemporal and inferotemporal sectors of the optic nerve. Within the optic nerve, the papillomacular fibers travel centrally, therefore external compression will typically cause a loss of peripheral vision. At the optic chiasm the nasal fibers, which supply the temporal visual field, decussate to join the temporal fibers of the contralateral optic nerve to form the optic tract. The optic tract fibers carry visual information from the contralateral hemifield of each eye.
As the RGC axons are unmyelinated anterior to the lamina cribrosa, reduction in RNFL thickness can be attributed to axonal loss (1). The pathophysiological basis of retrograde RGC degeneration and axonal damage from anterior visual pathway compression is not well known. Mechanical axonal destruction, ischemia and metabolic mechanisms have all been suggested (2-4). Damage to the axons may occur through axon loss, axoplasmic stasis, blockage of conduction and/or demyelination.
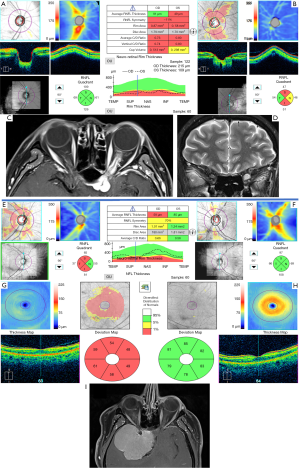
OCT assessment of lesions involving the optic chiasm
The chiasm is a common site for compression. Lesions abutting the optic chiasm superiorly or inferiorly will predominantly compress the decussating nasal fibers which results in retrograde RNFL loss on the nasal and temporal sides of the optic disc, clinically identified as bow tie or band atrophy of the optic disc (5,6). As a clinical sign, band atrophy can often be difficult to detect with ophthalmoscopy, whereas OCT segmentation techniques can quantify patterns of axonal loss objectively based on RNFL thinning.
Multiple studies have confirmed that patients with band atrophy tend to have RNFL loss in all quadrants around the optic disc, not just along the horizontal band (6-11). Monteiro et al. did not detect more RNFL thinning in the temporal and nasal regions compared to the vertical quadrants (12). However, ROC area under the curve analysis by Moura et al. showed preferential nasal and temporal RNFL loss in patients with band atrophy (13). Danesh-Meyer et al. also showed greater proportional thinning nasally and temporally in patients with bitemporal hemianopia from chiasmal compression (8).
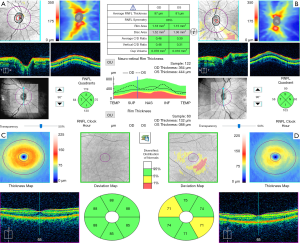
Global macular ganglion cell layer (GCL) thickness is also reduced in patients with anterior visual pathway compression, especially nasally (13-15). Some have compared the sensitivity of peripapillary RNFL versus macular GCL thickness in detecting visual pathway damage from chiasmal compression. Moura et al. found no difference in the degree of thinning between different sectors of the macular GCL and peripapillary RNFL (13). However, some studies have found macular RGC thinning to be more sensitive than RNFL loss in detecting chiasmal compression (16,17). Tieger et al. identified that the nasal RNFL and GCC thinning in patients with chiasm compression were both statistically significant, yet the effect size was much greater for GCC thinning (16). This discrepancy between RNFL and macular GCL thinning may reflect RNFL measurement variability in the peripapillary region due to variables such as optic disc area. Figure 1 demonstrates macular GCL thinning with normal RNFL in a case of left optic nerve compression.
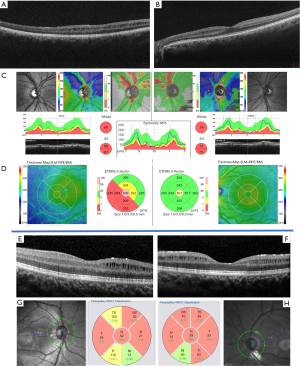
Macular microcystic changes in the inner nuclear layer may also be seen in anterior visual pathway compression (18,19). Inner nuclear layer thickening has also been reported (18). Figure 2 shows inner nuclear layer microcysts in a case of craniopharyngioma and giant prolactinoma where severe anterograde RNFL/RGC loss developed. Microcysts have also been found in optic neuritis (multiple sclerosis and neuromyelitis optica), glaucoma, Lebers hereditary optic neuropathy, dominant optic atrophy, and optic disc drusen (20-23). This finding has not been shown to be a disease specific biomarker but may rather reflect the severity of RGC loss and retinal thinning (24).
OCT angiography has been increasingly used to study perfusion of the macula and peripapillary retina at the level of the capillary microvasculature. A recent study found reduced circumpapillary and macular vessel density in eyes with band atrophy which correlated with RNFL thinning, GCL thinning and visual field loss (25). A smaller study of four patients with chiasmal compression also found reduced vessel density in peripapillary areas which correlated with visual field defects (26). The true benefit of OCT angiography as a biomarker in Neuro-Ophthalmological testing requires further research.
OCT and compressive lesions of the pre-chiasmatic optic nerves
Pre-chiasmal compression can also cause distinctive OCT changes. In unilateral optic nerve compression, asymmetry in RNFL and GCL thickness between the eyes is a major clue to the location of compression. RNFL may be increased from optic disc swelling or reduced in optic atrophy (27). Loo et al. looked at optic nerve compression by anterior visual pathway meningiomas (28). These eyes had significantly thinned peripapillary RNFL in all quadrants except temporally. However, RNFL can be normal in prechiasmal/chiasmal compression as exemplified in more than half the meningioma patients in another study (29). Also, Sibony et al. used OCT to identify an inward deformation of the retinal pigmented epithelial layer in patients with optic nerve sheath meningioma which worsened with larger tumors closer to the globe (27).
Apart from the aforementioned studies, mainly case reports document specific OCT changes in anterior optic nerve compression within the orbit. Convex retinal bowing and chorioretinal folds have been reported in retrobulbar cavernous hemangiomas and these OCT changes can persist even post tumor resection (30-32).
Figure 3 demonstrates a case of unilateral optic nerve sheath meningioma which presented with optic disc swelling. Whilst the OCT RNFL was thickened, GCL analysis showed thinning. In this case, OCT pointed towards a chronic pathogenic process of the anterior optic nerve.

Use of OCT to differentiate compressive optic neuropathies from glaucoma
In an Ophthalmology clinic setting, OCT can be an important diagnostic tool in distinguishing patients with compressive lesions from normotensive glaucoma which can both present with an enlarged cup to disc ratio. As band atrophy can be difficult to identify clinically, the predominantly horizontal peripapillary RNFL thinning is an important clue in compressive lesions which contrasts to the vertical RNFL thinning in glaucomatous optic neuropathy (33). Similarly, GCL loss in the nasal and temporal areas of the macula in chiasmal compressive lesions differs from the GCL thinning seen in glaucoma which tends to respect the horizontal meridian (14). Asymmetry in RNFL and GCL thinning between the eyes is also useful in distinguishing optic nerve compression from glaucoma. Figure 4 highlights two cases where OCT was used to identify optic nerve compression in patients who were mistakenly referred for glaucomatous optic disc cupping.
Relationship between OCT and visual function
Sellar masses can lead to visual dysfunction by causing progressive and often painless deterioration of visual acuity, color vision, and visual field. OCT augments the analysis of visual field testing in anterior compressive lesions by providing a structural-functional comparison. This is particularly important given the high test-retest variability and poor reliability of perimetry.
RNFL loss has shown to correlate with the severity of visual field loss from chiasmal compression (8). Sectoral analysis has shown strongest correlation between visual field mean deviation and temporal RNFL thinning (34,35). However, it is unwise to rely on RNFL alone as there are reports of severe visual field loss with intact peripapillary RNFL. This may occur in cases with more acute compression as axonal dysfunction may precede structural loss of axons as detected by OCT.
Macular GCL thickness has shown a greater relationship than RNFL thickness with visual field loss. Monteiro et al. found a stronger correlation (Rs 0.65–0.78) for macular thickness than RNFL thickness (Rs 0.60) with visual field loss (36). Moura et al. identified a correlation between nasal average macular thickness and visual field temporal mean deviation (R2=48%) (13). The stronger correlation with macular GCL thinning is plausible because it represents the central area of the visual field.
Different studies have shown RNFL and macular GCL thinning in patients with chronic mass lesions that radiologically appear to be compressing the anterior visual pathway despite no change in visual acuity or visual field (8,14,16,37). This suggests that the sensitivity of OCT supersedes perimetry testing. Thus, like in pre-perimetric glaucoma, OCT may have a role in identifying visual pathway damage from compressive lesions prior to functional loss.
Electrophysiological testing through visual evoked potentials (VEP), multifocal VEP (mfVEP) and pattern electroretinography (pERG) can quantify dysfunction along the visual pathway in compressive disease which can augment the interpretation of OCT structural analysis. VEP measures electrical signals received by the occipital cortex and the amplitude and velocity of these signals are diminished in lesions compressing any component of the visual pathway. In chiasmal compression, studies show reduced or delayed P100 during temporal hemifield stimulation which reflects dysfunction of the crossed RGC axons (crossed asymmetry distribution) (38). Topographical changes on mfVEP correspond to visual field defects in chiasmal compression (8,39,40). However, a relationship between VEP, mfVEP and OCT has not been shown, most likely because these electrophysiological tests reflect entire visual pathway function whereas OCT specifically focuses on RGC loss (41,42). PERG is thought to reflect RGC function in the central retinal area and in chiasmal compression, the N95 and b-wave can reduce (43). These changes have not shown correlation with OCT RNFL and GCL thinning (15,44), although multifocal pERG has (45).
OCT and compressive visual pathway lesions in pediatric patients
The use of OCT in children has been challenging. There is no normative data and data capture is dependent on patient age and cooperation. However, its role in monitoring optic nerve gliomas, the most common pediatric central nervous system tumor, has been increasingly studied.
Anatomical studies have shown that there is a decline in RNFL thickness with an increase in total glioma volume (46). However, the relationship of RNFL thickness with visual function has been less clear. In a study of children and young adults aged from 6 to 21 years with optic nerve glioma, RNFL thickness did not correlate well with visual acuity or visual field damage (46). The same research group has previously found RNFL to be predictive of vision loss (47).
Children with optic nerve gliomas who have normal RNFL, have demonstrated normal visual acuity and visual fields which can help with prognostication but limits the use of OCT in monitoring for progression before functional deficits occur (48,49). Another study showed RNFL thinning in patients with glioma growth regardless of vision change, meaning that OCT may be able to detect subclinical changes (50).
There has been growing interest in the use of OCT to identify choroidal abnormalities in neurofibromatosis associated optic nerve gliomas. These abnormalities are detected with the use of infrared reflectance retinography on spectral domain OCT (51).
OCT and visual prognostication after surgical intervention
RGC axonal structural and functional recovery post decompression surgery is not well understood. Visual field recovery likely reflects recovery of dysfunctioning axons. Many factors have been explored as predictors of visual acuity and visual field post-operative recovery such as symptom duration, age, optic disc appearance, severity of preoperative visual field loss, surgical technique, tumor size and volume and pattern electroretinography, however the results have been variable (28,52-56). Pre-operative OCT findings have proven to be the most consistent prognosticator.
Multiple studies, including a meta-analysis, have shown that preoperative RNFL thinning is a predictor of poor visual field recovery (8,29,35,57-59). The pooled odds ratio in the meta-analysis was 15.61 (95% CI: 4.09–59.61) for field recovery in eyes with normal RNFL compared to those with abnormal RNFL (57). In a large prospective study, visual field recovery was better in the patients with normal RNFL compared to those with abnormal RNFL (81% of eyes versus 37% respectively over one year postoperatively) (35). Garcia et al. showed that eyes with greater nasal, rather than global, RNFL thickness had more peripheral visual field recovery postoperatively (60). Jacob et al. demonstrated that temporal RNFL thinning below the 5th percentile was associated with poorer visual field recovery (59).
Multiple studies have also identified a strong association between preoperative GCL thinning and poorer visual field recovery (16,34,61). Tieger et al. found a greater correlation of visual field mean deviation with GCL than RNFL thickness (R2 0.25 vs. 0.15 respectively) (16).
In chiasmal decompression, eyes with normal RNFL have greater improvement in visual acuity as well (8). 98% of the eyes with normal RNFL achieved acuities 6/12 or better compared with 88% of the thin RNFL eyes postoperatively. Danesh-Meyer et al. suggested a presurgical threshold RNFL of 75 µm is associated with a worse post-operative visual prognosis. Loo et al. suggested a RNFL threshold of 70 µm but the focus was on optic nerve more than chiasmal compression (28).
RNFL and macular GCL thickness do not change significantly post-operatively despite visual acuity and field recovery over months to years (8). Thus, further thinning of these parameters can be useful in monitoring for recurrent compression of any residual tumor. However, the direct effect of surgery on OCT measurements needs to be considered when monitoring.
Conclusions
OCT has an emerging role in the management of patients with space occupying lesions compressing the anterior visual pathway. Peripapillary RNFL and the macular RGC complex have both proven important in diagnosis, preoperative prognostication and post-operative monitoring of these patients. The ease of access, resolution of detail, reliability and clinical objectivity of OCT heighten the need to incorporate it into routine neuro-ophthalmic assessment. Small study populations and tumor heterogeneity limit the external validity of many OCT studies. However, more research and technological advancement in OCT will shed more light into its role in areas such as pediatric visual pathway gliomas and indications for surgical tumor decompression.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Fiona Costello and Steffen Hamann) for the series “The Use of OCT as a Biomarker in Neuro-ophthalmology” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2019.12.07). The series “The Use of OCT as a Biomarker in Neuro-ophthalmology” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethics approval was not required as this was a review article of current literature. Written informed consent was obtained from the patient for publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Costello F, Coupland S, Hodge W, et al. Quantifying axonal loss after optic neuritis with optical coherence tomography. Ann Neurol 2006;59:963-9. [Crossref] [PubMed]
- Cottee LJ, Daniel C, Loh WS, et al. Remyelination and recovery of conduction in cat optic nerve after demyelination by pressure. Exp Neurol 2003;184:865-77. [Crossref] [PubMed]
- Gao Y, Weng C, Wang X. Changes in nerve microcirculation following peripheral nerve compression. Neural Regen Res 2013;8:1041-7. [PubMed]
- Cioffi GA. Ischemic model of optic nerve injury. Trans Am Ophthalmol Soc 2005;103:592-613. [PubMed]
- Unsöld R, Hoyt WF. Band atrophy of the optic nerve. The histology of temporal hemianopsia. Arch Ophthalmol 1980;98:1637-8. [Crossref] [PubMed]
- Monteiro ML, Leal BC, Rosa AA, et al. Optical coherence tomography analysis of axonal loss in band atrophy of the optic nerve. Br J Ophthalmol 2004;88:896-9. [Crossref] [PubMed]
- Kanamori A, Nakamura M, Matsui N, et al. Optical coherence tomography detects characteristic retinal nerve fiber layer thickness corresponding to band atrophy of the optic discs. Ophthalmology 2004;111:2278-83. [Crossref] [PubMed]
- Danesh-Meyer HV, Carroll SC, Foroozan R, et al. Relationship between retinal nerve fiber layer and visual field sensitivity as measured by optical coherence tomography in chiasmal compression. Invest Ophthalmol Vis Sci 2006;47:4827-35. [Crossref] [PubMed]
- Costa-Cunha LV, Cunha LP, Malta RF, et al. Comparison of Fourier-domain and time-domain optical coherence tomography in the detection of band atrophy of the optic nerve. Am J Ophthalmol 2009;147:56-63.e2. [Crossref] [PubMed]
- Monteiro ML, Cunha LP, Vessani RM. Comparison of retinal nerve fiber layer measurements using Stratus OCT fast and regular scan protocols in eyes with band atrophy of the optic nerve and normal controls. Arq Bras Oftalmol 2008;71:534-9. [Crossref] [PubMed]
- Sun M, Zhang Z, Ma C, et al. Quantitative analysis of retinal layers on three-dimensional spectral-domain optical coherence tomography for pituitary adenoma. PLoS One 2017;12:e0179532 [Crossref] [PubMed]
- Monteiro ML, Leal BC, Moura FC, et al. Comparison of retinal nerve fibre layer measurements using optical coherence tomography versions 1 and 3 in eyes with band atrophy of the optic nerve and normal controls. Eye (Lond) 2007;21:16-22. [Crossref] [PubMed]
- Moura FC, Medeiros FA, Monteiro ML. Evaluation of macular thickness measurements for detection of band atrophy of the optic nerve using optical coherence tomography. Ophthalmology 2007;114:175-81. [Crossref] [PubMed]
- Yum HR, Park SH, Park HY, et al. Macular Ganglion Cell Analysis Determined by Cirrus HD Optical Coherence Tomography for Early Detecting Chiasmal Compression. PLoS One 2016;11:e0153064 [Crossref] [PubMed]
- Cennamo G, Auriemma RS, Cardone D, et al. Evaluation of the retinal nerve fibre layer and ganglion cell complex thickness in pituitary macroadenomas without optic chiasmal compression. Eye (Lond) 2015;29:797-802. [Crossref] [PubMed]
- Tieger MG, Hedges TR, Ho J, et al. Ganglion Cell Complex Loss in Chiasmal Compression by Brain Tumors. J Neuroophthalmol 2017;37:7-12. [Crossref] [PubMed]
- Jeong AR, Kim EY, Kim NR. Preferential Ganglion Cell Loss in the Nasal Hemiretina in Patients With Pituitary Tumor. J Neuroophthalmol 2016;36:152-5. [Crossref] [PubMed]
- Monteiro ML, Hokazono K, Fernandes DB, et al. Evaluation of inner retinal layers in eyes with temporal hemianopic visual loss from chiasmal compression using optical coherence tomography. Invest Ophthalmol Vis Sci 2014;55:3328-36. [Crossref] [PubMed]
- Abegg M, Zinkernagel M, Wolf S. Microcystic macular degeneration from optic neuropathy. Brain 2012;135:e225 [Crossref] [PubMed]
- Barboni P, Carelli V, Savini G, et al. Microcystic macular degeneration from optic neuropathy: not inflammatory, not trans-synaptic degeneration. Brain 2013;136:e239 [Crossref] [PubMed]
- Balk LJ, Killestein J, Polman CH, et al. Microcystic macular oedema confirmed, but not specific for multiple sclerosis. Brain 2012;135:e226; author reply e7.
- Wolff B, Azar G, Vasseur V, et al. Microcystic changes in the retinal internal nuclear layer associated with optic atrophy: a prospective study. J Ophthalmol 2014;2014:395189 [Crossref] [PubMed]
- Kessel L, Hamann S, Wegener M, et al. Microcystic macular oedema in optic neuropathy: case series and literature review. Clin Exp Ophthalmol 2018;46:1075-86. [Crossref] [PubMed]
- Abegg M, Dysli M, Wolf S, et al. Microcystic macular edema: retrograde maculopathy caused by optic neuropathy. Ophthalmology 2014;121:142-9. [Crossref] [PubMed]
- Suzuki ACF, Zacharias LC, Preti RC, et al. Circumpapillary and macular vessel density assessment by optical coherence tomography angiography in eyes with temporal hemianopia from chiasmal compression. Correlation with retinal neural and visual field loss. Eye (Lond) 2019. [Epub ahead of print].
- Higashiyama T, Ichiyama Y, Muraki S, et al. Optical Coherence Tomography Angiography of Retinal Perfusion in Chiasmal Compression. Ophthalmic Surg Lasers Imaging Retina 2016;47:724-9. [Crossref] [PubMed]
- Sibony P, Strachovsky M, Honkanen R, et al. Optical coherence tomography shape analysis of the peripapillary retinal pigment epithelium layer in presumed optic nerve sheath meningiomas. J Neuroophthalmol 2014;34:130-6. [Crossref] [PubMed]
- Loo JL, Tian J, Miller NR, et al. Use of optical coherence tomography in predicting post-treatment visual outcome in anterior visual pathway meningiomas. Br J Ophthalmol 2013;97:1455-8. [Crossref] [PubMed]
- Park HH, Oh MC, Kim EH, et al. Use of optical coherence tomography to predict visual outcome in parachiasmal meningioma. J Neurosurg 2015;123:1489-99. [Crossref] [PubMed]
- Weir RE, Evans S, Hajdu SD, et al. The convex retina: optical coherence tomography in hypermetropic shift, without choroidal folds, from intraconal cavernous haemangioma. Orbit 2009;28:398-400. [Crossref] [PubMed]
- Jacobsen AG, Toft PB, Prause JU, et al. Long term follow-up of persistent choroidal folds and hyperopic shift after complete removal of a retrobulbar mass. BMC Res Notes 2015;8:678. [Crossref] [PubMed]
- Heisel CJ, Zacks DN, Kahana A. Persistent macular puckering following excision of causative orbital tumor. Am J Ophthalmol Case Rep 2018;10:196-7. [Crossref] [PubMed]
- Mwanza JC, Oakley JD, Budenz DL, et al. Ability of cirrus HD-OCT optic nerve head parameters to discriminate normal from glaucomatous eyes. Ophthalmology 2011;118:241-8.e1. [Crossref] [PubMed]
- Moon CH, Hwang SC, Ohn YH, et al. The time course of visual field recovery and changes of retinal ganglion cells after optic chiasmal decompression. Invest Ophthalmol Vis Sci 2011;52:7966-73. [Crossref] [PubMed]
- Danesh-Meyer HV, Wong A, Papchenko T, et al. Optical coherence tomography predicts visual outcome for pituitary tumors. J Clin Neurosci 2015;22:1098-104. [Crossref] [PubMed]
- Monteiro ML, Costa-Cunha LV, Cunha LP, et al. Correlation between macular and retinal nerve fibre layer Fourier-domain OCT measurements and visual field loss in chiasmal compression. Eye (Lond) 2010;24:1382-90. [Crossref] [PubMed]
- Blanch RJ, Micieli JA, Oyesiku NM, et al. Optical coherence tomography retinal ganglion cell complex analysis for the detection of early chiasmal compression. Pituitary 2018;21:515-23. [Crossref] [PubMed]
- Brecelj J. A VEP study of the visual pathway function in compressive lesions of the optic chiasm. Full-field versus half-field stimulation. Electroencephalogr Clin Neurophysiol 1992;84:209-18. [Crossref] [PubMed]
- Jayaraman M, Ambika S, Gandhi RA, et al. Multifocal visual evoked potential recordings in compressive optic neuropathy secondary to pituitary adenoma. Doc Ophthalmol 2010;121:197-204. [Crossref] [PubMed]
- Raz N, Bick AS, Klistorner A, et al. Physiological Correlates and Predictors of Functional Recovery After Chiasmal Decompression. J Neuroophthalmol 2015;35:348-52. [Crossref] [PubMed]
- Qiao N, Zhang Y, Ye Z, et al. Comparison of multifocal visual evoked potential, static automated perimetry, and optical coherence tomography findings for assessing visual pathways in patients with pituitary adenomas. Pituitary 2015;18:598-603. [Crossref] [PubMed]
- Ventura LM, Venzara FX, Porciatti V. Reversible dysfunction of retinal ganglion cells in non-secreting pituitary tumors. Doc Ophthalmol 2009;118:155-62. [Crossref] [PubMed]
- Holder GE. The pattern electroretinogram in anterior visual pathway dysfunction and its relationship to the pattern visual evoked potential: a personal clinical review of 743 eyes. Eye (Lond) 1997;11:924-34. [Crossref] [PubMed]
- Monteiro ML, Cunha LP, Costa-Cunha LV, et al. Relationship between optical coherence tomography, pattern electroretinogram and automated perimetry in eyes with temporal hemianopia from chiasmal compression. Invest Ophthalmol Vis Sci 2009;50:3535-41. [Crossref] [PubMed]
- Monteiro ML, Hokazono K, Cunha LP, et al. Correlation between multifocal pattern electroretinography and Fourier-domain OCT in eyes with temporal hemianopia from chiasmal compression. Graefes Arch Clin Exp Ophthalmol 2013;251:903-15. [Crossref] [PubMed]
- Avery RA, Mansoor A, Idrees R, et al. Optic pathway glioma volume predicts retinal axon degeneration in neurofibromatosis type 1. Neurology 2016;87:2403-7. [Crossref] [PubMed]
- Avery RA, Cnaan A, Schuman JS, et al. Longitudinal Change of Circumpapillary Retinal Nerve Fiber Layer Thickness in Children With Optic Pathway Gliomas. Am J Ophthalmol 2015;160:944-52.e1. [Crossref] [PubMed]
- Avery RA, Liu GT, Fisher MJ, et al. Retinal nerve fiber layer thickness in children with optic pathway gliomas. Am J Ophthalmol 2011;151:542-9.e2. [Crossref] [PubMed]
- Chang L, El-Dairi MA, Frempong TA, et al. Optical coherence tomography in the evaluation of neurofibromatosis type-1 subjects with optic pathway gliomas. J AAPOS 2010;14:511-7. [Crossref] [PubMed]
- Fard MA, Fakhree S, Eshraghi B. Correlation of optical coherence tomography parameters with clinical and radiological progression in patients with symptomatic optic pathway gliomas. Graefes Arch Clin Exp Ophthalmol 2013;251:2429-36. [Crossref] [PubMed]
- Parrozzani R, Clementi M, Frizziero L, et al. In Vivo Detection of Choroidal Abnormalities Related to NF1: Feasibility and Comparison With Standard NIH Diagnostic Criteria in Pediatric Patients. Invest Ophthalmol Vis Sci 2015;56:6036-42. [Crossref] [PubMed]
- Galal A, Faisal A, Al-Werdany M, et al. Determinants of postoperative visual recovery in suprasellar meningiomas. Acta Neurochir (Wien) 2010;152:69-77. [Crossref] [PubMed]
- Wang H, Sun W, Fu Z, et al. The pattern of visual impairment in patients with pituitary adenoma. J Int Med Res 2008;36:1064-9. [Crossref] [PubMed]
- Chabot JD, Chakraborty S, Imbarrato G, et al. Evaluation of Outcomes After Endoscopic Endonasal Surgery for Large and Giant Pituitary Macroadenoma: A Retrospective Review of 39 Consecutive Patients. World Neurosurg 2015;84:978-88. [Crossref] [PubMed]
- Barzaghi LR, Medone M, Losa M, et al. Prognostic factors of visual field improvement after trans-sphenoidal approach for pituitary macroadenomas: review of the literature and analysis by quantitative method. Neurosurg Rev 2012;35:369-78; discussion 378-9. [Crossref] [PubMed]
- Findlay G, McFadzean RM, Teasdale G. Recovery of vision following treatment of pituitary tumours; application of a new system of assessment to patients treated by transsphenoidal operation. Acta Neurochir (Wien) 1983;68:175-86. [Crossref] [PubMed]
- Zhang J, Zhang S, Song Y, et al. Predictive value of preoperative retinal nerve fiber layer thickness for postoperative visual recovery in patients with chiasmal compression. Oncotarget 2017;8:59148-55. [Crossref] [PubMed]
- Yoneoka Y, Hatase T, Watanabe N, et al. Early morphological recovery of the optic chiasm is associated with excellent visual outcome in patients with compressive chiasmal syndrome caused by pituitary tumors. Neurol Res 2015;37:1-8. [Crossref] [PubMed]
- Jacob M, Raverot G, Jouanneau E, et al. Predicting visual outcome after treatment of pituitary adenomas with optical coherence tomography. Am J Ophthalmol 2009;147:64-70.e2. [Crossref] [PubMed]
- Garcia T, Sanchez S, Litré CF, et al. Prognostic value of retinal nerve fiber layer thickness for postoperative peripheral visual field recovery in optic chiasm compression. J Neurosurg 2014;121:165-9. [Crossref] [PubMed]
- Ohkubo S, Higashide T, Takeda H, et al. Relationship between macular ganglion cell complex parameters and visual field parameters after tumor resection in chiasmal compression. Jpn J Ophthalmol 2012;56:68-75. [Crossref] [PubMed]
Cite this article as: Kaushik M, Fraser CL. Optical coherence tomography in compressive lesions of the anterior visual pathway. Ann Eye Sci 2020;5:15.


