
Commentary on effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE)
Background
Relative pupil block is the most common mechanism of intraocular pressure (IOP) elevation in primary angle-closure glaucoma (PACG) and primary angle closure (PAC). The standard approach of treating PACG and PAC is laser peripheral iridotomy (LPI) with or without additional IOP-lowering agents. If IOP remains poorly controlled, lens removal could be considered, especially if the patient has co-existing symptomatic cataract. The efficacy of lowering IOP by lens extraction for patients with co-existing cataract and PACG or PAC is known (1-4). Some authors had suggested an early lens extraction approach as the treatment of choice for PACG (5,6). However, the justification of performing clear-lens extraction as first-line treatment instead of LPI for this group of patients, who have satisfactory visual acuity, is often obviated by the concern of potentially serious complications, such as malignant glaucoma. There has been no randomised control trial to justify clear-lens extraction as the first-line treatment in clinical practice.
The effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE) study is a multicentred, comparative, randomised control trial to assess the efficacy, safety and cost-effectiveness of clear lens extraction compared with the standard approach as first-line treatment for newly diagnosed PAC with raised IOP or PACG (7). The EAGLE study group has recently published their data from Jan 8, 2009 to Dec 28, 2011.
Design and results
The study recruited patients who were phakic, aged ≥50 years old, and had newly diagnosed PAC with IOP ≥30 mmHg or PACG. Patients with symptomatic cataract, advanced glaucoma (mean deviation worse than −15 dB or cup-to-disc ratio ≥0.9), or had previous laser or ocular surgery were excluded. After assessing 805 potential subjects in 30 hospitals of 5 different countries, 386 patients were ineligible or chose not to participate, 419 patients were found eligible and were randomised to either undergo clear lens extraction (208 patients) or the standard care (211 patients). The interventions were performed within 60 days of diagnosis and topical medications were given during this interval. Patients who only had one eye eligible were recruited. If both eyes were eligible, the eye with more severe disease was chosen. The target IOP was set at 15–20 mmHg, depending on the degree of optic nerve damage. Additional topical medication could be used to control the IOP. For the clear-lens extractions group, additional synechialysis was allowed according to local practice. Laser iridoplasty was allowed after standard care, if appositional angle closure persisted. Health status and visual function were also assessed. Health status was measured by the European Quality of Life-5 Dimensions (EQ-5D) questionnaire; whereas vision problems on vision-targeted functioning and health-related quality of life were measured by National Eye Institute Visual Function Questionanaire-25 (NEI-VFO-25).
The study demonstrated that clear-lens extraction resulted in greater efficacy, better health status score, better visual quality, higher reduction of needs of medication and prevent further glaucoma surgery compared to the standard treatment. Authors concluded that clear-lens extraction was more cost-effective than laser peripheral iridotomy, and should be considered as an option for first-line treatment.
Commentary
The EAGLE study design has many strengths, including a pragmatic study design, large sample size with involvement of centres in United Kingdom and Asia, strictly applied enrolment protocols, computerised randomisation process, masking of clinical assessment of IOP measurement, visual acuity and visual fields. It is a prospective, longitudinal assessment with determinate endpoints, including the consideration of quality of life and cost-effectiveness aspect.
Ophthalmologists are often reluctant to perform lens extraction for patients with PACG or PAC if they have good visual acuity and adequate IOP control after laser iridotomy. Results of the EAGLE study evidently support the more radical approach of clear-lens extraction as the first-line treatment, if the operation is performed by highly trained specialist. Indeed, the apparent “clear-lens” in this group of patients should not be considered as having a normal lens because age-related lens changes has already led to narrowing of the angle and a consequential IOP elevation in these situations. In the study, the mean baseline best correct visual acuity were 80.0 and 79.0 ETDRS letters for the clear-lens extraction group and the LPI group respectively, suggesting that the cohort had at least some mild age-related changes in the lens transparency. Hence, the visual benefit of removing the “clear-lens” as demonstrated in the study.
We should also keep in mind some of the limitations of the study. The study targeted a very specific group of patients—aged ≥50 years old, with PAC and IOP of ≥30 mmHg or mild to moderate PACG (visual field with median deviation of >−15 dB or cup-to-disc ratio of <0.9). Patients younger than 50, with PAC that have IOP <30 mmHg were excluded. The study also demonstrated an improvement in quality of life likely to be due to improvement of visual function, correction of refractive error, and reduced need for glaucoma medication/surgery after clear-lens extraction. However, one should also be aware of the potential sampling bias during the recruitment stage; almost half of the patients (386/805; 48.0%) were excluded during the recruitment stage because of ineligibility or chose not to participate. The strict inclusion criteria may explain the large number of exclusion. There could also be numerous reasons for the refusal of participation. For instance, it is logical to suggest that at least some of those patients who refused to participate were already satisfied with their visual function and health status, including their acceptance of the potential needs of medication after undergoing the standard treatment (i.e., LPI). These were patients who might be reluctant to put themselves under the possibility to undergoing lens extraction, which is a more risky procedure – at least in the patients’ point of views. In that sense, the study had effectively selected participants with more proactive characters, who would have expected an improvement in their visual function and quality of life should they be randomised into the clear-lens extraction group. Since the ED-5D and NEI-VFO-25 questionnaires results rely on patients’ own perceptions, and given that it was impossible to mask the patients from knowing which treatment arm they underwent, there could be another potential bias during the post-operative ED-5D and NEI-VFO-25 questionnaire assessments.
The study did not show any significant difference in the degree of synechial angle closure at 36 months between the two treatments group. However, the result was compromised by a large amount of missing data (123 or 59.1% for the clear lens extraction group and 132 or 62.6% of the LPI group). There was also no significant difference in the visual field test results between the two groups; whether there would be any difference in the longer term requires further publication from the EAGLE study group. This is important to address, because the beneficial effects of clear-lens extraction was based on the low surgical complication rate of the highly trained specialists. Potentially more severe complications in clear-lens extraction, such as ruptured posterior capsule and malignant glaucoma, should be taken into account from the perspective of individual patients, rather than merely as a net effect of the cohort, especially if less experienced surgeons perform the surgery. Notice that the major advantage of clear lens extraction that were demonstrated throughout the 3-year horizon were improvement in health status, reduction of medication, and reduction of the needs of further operations. For the latter, only one trabeculectomy was performed for the clear lens extraction group. Whereas for the standard care group, 24 additional operations were performed, including 16 (67%) lens extractions, 6 (25%) trabeculectomies, 1 (4%) i-stent insertion, and 1 (4%) Ahmed tube insertion. Twelve of the 16 lens extractions were performed because of the development of clinically relevant cataracts. The rest of the operations were chosen according to the treating ophthalmologists’ judgments. Therefore, whether or not these patients could benefit from lens extraction, instead of other glaucoma surgeries, is not known. Similarly, whether or not such “delay” in lens extraction to lower the IOP could lead to disadvantage in the longer term is also unknown. In the clinical and public health care point of view, reader should consider clear lens extraction only after weighting the risk and benefit in the context of their own localities and health care system. This timing aspect of lens extraction could be potentially important, especially in countries with long waiting list for cataract operation. Inappropriately prioritising clear lens extraction for patients with PAC and mild to moderate PACG could mean an opportunity cost to others who require cataract operation for other reasons.
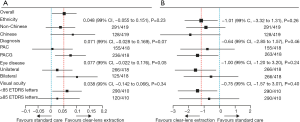
For the subgroup analyses (Figure 1) in the EAGLE study, no statistical difference of EQ-5D and IOP was noted between the subgroups. However, there is a tendency of neutral favourability between the choice of clear-lens extraction and standard care when considering the EQ-D5 score and the magnitude of IOP lowering for the subgroup of patients with PAC and the subgroup with visual acuity of ≥85 ETDRS letters (Figure 1). The ranges of confidence interval actually crossed the zero point. This is not the case in either the subgroup with PACG, or the subgroup with visual acuity of <85 ETDRS letters. This could reflect a tendency of that clear-lens extraction is more effective in more advanced disease status, though not reviewed in the study. It will be useful if there are factors that could predict the degree of effectiveness for clear-lens extraction in this group of patients. We should also bear in mind that other important angle closure mechanisms, such as plateau iris configuration, are also important and might not be entirely reversed by lens extraction. The EAGLE study did not specifically evaluate the mechanisms of angle closure for each patient. Clinician should treat their patients according to individual needs.
In the study, the incremental cost-effectiveness ratio was £14,284 for initial lens extraction versus standard care. At a ceiling willingness-to-pay ratio (WTP ratio) of £20,000 per quality adjusted life year (QALY) the probably of early clear-lens extraction being cost-effective is 67% based on complete case data, or 89% based on the multiple imputation analysis. One would need to interpret the cost-effectiveness aspect of the study with great care. Firstly, the clinical course of the cohort in a longer period of time (e.g., 5 years) is uncertain until further publication. Longer term data would allow a formal cost-effectiveness analysis using stochastic model, such as Markov model, which would be beneficial for health care policy decision-making. Secondary, the cost were assessed only for subset of patients treated in the United Kingdom; many other patients were not included. For this reason, it cannot be applied for other countries or health systems (8). It is important to note that the cost-effectiveness of a procedure in treating a particular condition depends on the country’s Per Capita Gross domestic production (Per Capita GDP). This is calculated by the total output of a country that takes GDP and divided by the total population of the country. The WTP ratio of £20,000 per QALY is acceptable in countries such as the United Kingdom, where the Per Capita GDP in the year 2015 was 43,734 US dollar (9). However, this might be different in other territories where the WTP ratios are lower because of different living standards. For instance, China has a Per-Capita GDP of 7,925 US dollar in the year 2015 (9); the WTP ratio would be expectedly lower in that case, though the cost of performing cataract operation might also be lower in China. Therefore, readers should consider the health economical aspect of this study in the context of their own localities, rather than simply implementing the conclusion of the study without further interpretation.
Conclusions
The EAGLE study has achieved its primary aim to demonstrate that initial clear-lens extraction would be associated with better quality of life, lower IOP, and less need for glaucoma surgery at 36 months than standard care. The strength of the study design supports clear-lens extraction as the more advantageous treatment option for patients with PACG and patients with PAC who had elevated IOP of >30 mmHg.
However, surgical decision is still an art. Until further study that provides predictive factors that would help us to identify individuals who are more likely to benefit from clear-lens extraction as first line treatment, the decision should be made carefully after thorough evaluation and discussion with individual patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by Section Editor Yi Sun, MD (Department of Ophthalmology, The Third Affiliated Hospital of Sun Yat-sen University, Guangzhou, China).
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.03.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen PP, Lin SC, Junk AK, et al. The Effect of Phacoemulsification on Intraocular Pressure in Glaucoma Patients: A Report by the American Academy of Ophthalmology. Ophthalmology 2015;122:1294-307. [Crossref] [PubMed]
- Tham CC, Kwong YY, Baig N, et al. Phacoemulsification versus trabeculectomy in medically uncontrolled chronic angle-closure glaucoma without cataract. Ophthalmology 2013;120:62-7. [Crossref] [PubMed]
- Tham CC, Kwong YY, Leung DY, et al. Phacoemulsification versus combined phacotrabeculectomy in medically uncontrolled chronic angle closure glaucoma with cataracts. Ophthalmology 2009;116:725-31,731.e1-3.
- Tham CC, Kwong YY, Leung DY, et al. Phacoemulsification versus combined phacotrabeculectomy in medically controlled chronic angle closure glaucoma with cataract. Ophthalmology 2008;115:2167-73.e2. [Crossref] [PubMed]
- Thomas R, Walland MJ, Parikh RS. Clear lens extraction in angle closure glaucoma. Curr Opin Ophthalmol 2011;22:110-4. [Crossref] [PubMed]
- Dada T, Rathi A, Angmo D, et al. Clinical outcomes of clear lens extraction in eyes with primary angle closure. J Cataract Refract Surg 2015;41:1470-7. [Crossref] [PubMed]
- Azuara-Blanco A, Burr J, Ramsay C, et al. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet 2016;388:1389-97. [Crossref] [PubMed]
- Traverso CE. Clear-lens extraction as a treatment for primary angle closure. Lancet 2016;388:1352-4. [Crossref] [PubMed]
- The World Bank group [Internet] Washington: The World Bank open data 2016 [cited 2016 Nov 22]. Available online: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD
Cite this article as: Chan PP, Tham CC. Commentary on effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE). Ann Eye Sci 2017;2:21.


