
Myopia prevention in Taiwan
Over 22% of the global population has myopia, which affects 1.5 billion people (1). Around one fifth to one quarter of myopic people has high myopia (1,2). Myopia is not to be considered a simple refractive error, but should be considered as a disease because it increases the risk of serious eye disorders, such as retinal detachment, cataract, glaucoma, maculopathy, and even irreversible blindness (3-5). High myopia maculopathy is the number one cause of irreversible blindness in Taiwan, Japan, and China (6-8). In the West, it is the third leading cause of blindness in Denmark, the Netherlands, and in the Latino American population (9-11). Chauvaud has proposed that high myopia is a blinding orphan because most of the complications of myopia are incurable (12). Therefore, the prevention of myopia is an important public health issue.
In Taiwan, the government has paid much attention to the vision care of students starting from 30 years ago. The Taiwan Student Vision Care Program (TSVCP) is continued promoted by Ministry of Education (MOE). From 1980, the Executive Yuan considered myopia to be a serious public health issue and instructed relevant departments, including the MOE and the Department of Health (DOH) to initiate “enhancing important measures of student vision care”. Nationwide student vision screenings and referrals by school nurses were routinely performed each semester. In 1986, the DOH supported grants to set the center of child vision care in five medical centers to initiate myopia prevention and treatment. In addition, the DOH granted the “Epidemiology study of cycloplegic refraction status of 6–18 years old students in Taiwan” every 5 years. In 1995, the DOH promoted random dot stereopsis tests and vision screening for amblyopia and strabismus screening in 5 years old preschool children. In 1999, the Executive Yuan led the MOE, DOH, Ministry of the Interior, and associated departments to conduct “enhancing schoolchildren vision care—5 year program”. In 2007–2009, MOE granted the “schoolchildren and pre-schooler vision care program”. In 2010, MOE granted the “schoolchildren and pre-schooler vision care—3 year program”. From 2014 to the present, MOE granted the “schoolchildren vision care program”.
In the period of the “enhancing schoolchildren vision care—5 year program” (1999–2004), amblyopia & strabismus in kindergarten achieved a 95% population screen. Vision impairment referrals of over 80% were achieved. Both items achieved preset goals. During this period, the key items for myopia prevention included improving room lighting, adjusting table heights for individual students, encouraging distance gazing, eye exercise and promoting near work breaks. Even though this required significant manpower and budget, the results were still unsatisfactory. From the nationwide survey in 2006, myopia prevalence was 19.6% in 7 year-old students and 61.8% in 12 year-old students (13). Myopia prevalence was still high in compared to year 2000, 20.4% in 7 year-old students and 60.6% in 12 year-old students. The reason might be lack of strong evidence based strategies for myopia prevention at that time. The vision impairment rate of primary school in Taiwan also increased according to a MOE report. The vision impairment rate (cut-off point is Snellen visual acuity 20/25 or less) was considered to be high correlated with myopia prevalence (14,15). Despite great promotion of this 5-year program over 3,000 schools, the state of myopia in Taiwan still worsened. Most teachers were frustrated and considered the high prevalence of myopia as predestined in Taiwan.
In 1986, the myopia prevalence of 7 years old children was only 3%, but rose to 21% in 2010 (13). Over 60% of 12 years old students and over 85% of 18 years old high school students were myopic. The high myopia prevalence in 18 years old population increased from 9.2% in 1986 to 20.8% in 2000. Shih reported the effectiveness of atropine on myopia progression in Taiwanese schoolchildren in 1999 (16). Then, a large number of myopic children were prescribed the atropine eye drop treatment for myopia control (17). Thereafter in 2006, the high myopia prevalence in 18 years old slightly decreased to 16.9%.
After 2007–2009 when the “schoolchildren and pre-schooler vision care program” was performed, the vision impairment rate was still increasing almost up to 50% (Figure 1). In 2007, Jones et al. reported that 14 hours outdoors per week could reverse the risk of myopia due to parental myopia (18). In 2008, Rose et al. published an important paper about outdoor activity reducing the prevalence of myopia in children (19). Saw provided Singapore’s data compared to a Sydney myopia study that showed around 14 hours outdoors per week might be the main cause of low myopia prevalence in Sydney schoolchildren (20). The preliminary domestic data also showed outdoor activities might be an important protecting factor for myopia among rural school children in Taiwan (21). In the vision care advisory council of the MOE in 2009, the author (PC Wu) proposed the new concept in the council that outdoor activities should be added as an important item in TSVCP and suggested at least 2 hours outdoors for myopia prevention. It was demonstrated by the domestic and foreign studies mentioned above. The director general of the Sports Division of the MOE (Chun-Chuan Wang) then accepted the concept and implemented the 120 minutes of outdoor activity everyday “Tien Tien 120” for myopia prevention into TSVCP from 2010. There was a transition period that shifted from distance gazing to outdoor activities. Therefore, outdoor distance gazing for 120 minutes everyday was promoted in 2010 initially, and then replaced by 120 minutes of outdoor activities every day, regardless of the type of activity. Thirty minutes of near work followed by a 10 minute-break [3010], improved room lighting, and adjusting table heights continued to be promoted in schools. In 2013, Wu reported that outdoor activity during class recess has the effect of myopia prevention in schoolchildren (22). This study showed the recess outside classroom (ROC) program could decrease half of the new onsets of myopia and myopic shift, especially in non-myopic children. After that, classroom clearance during recess was promoted in schools. From 2014, spreading the important concept of “myopia disease” was additionally implemented into TSVCP and health education.
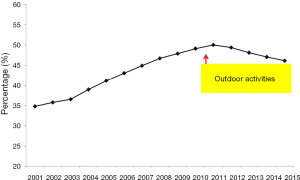
The vision impairment rate of primary school children in Taiwan dramatically decreased, unprecedentedly, and continued after the outdoor implementation from 2012 to 2015 to around 46% (Figure 1). This may represent that the outdoor activity implementation in TSVCP works in myopia prevention among schoolchildren in Taiwan. Outdoor recess is simple, free, and an effective intervention for children and is widely reported in the media. Although outdoor activity is promising for myopia prevention, the challenge of being glued to a screen (smartphone addiction) is coming. In any case, there is still a long way to fight against myopia. The silence of myopia is possible and can be anticipated.
Nowadays, the TSVCP is reiterating to teachers and students that myopia is an irreversible disease and progresses in children. In addition, outdoor activities and near work breaks are the main items for myopia prevention promoted in school. Meeting and looking for consensus between the educational, health, and medical care systems are held regularly for myopia prevention. For myopic children, the referral system to ophthalmologists is continuing to be monitored. Evidence-based effective treatments such as low concentration atropine or orthokeratology are the treatments of choice for the control of myopia.
In conclusion, complications of myopia have become an important public health issue with serious socio-economic burdens. Prevention and treatment are both important. Evidence-based protective and risk factors have become clearer. Proper conceptualization of myopic disease, preventing the onset of myopia, prompt diagnosis, and early treatment to control progression are all important. The aim of the TSVCP is to decrease the prevalence of myopia, in order to decrease the high myopia related blind population in the near future.
Acknowledgments
The authors thank all the contributors in the Taiwan Student Vision Care Program.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ian G. Morgan, Xiaohu Ding and Xinxing Guo) for the series “Managing Myopia in East Asia Myopia Crisis” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.01.05). The series “Managing Myopia in East Asia Myopia Crisis” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036-42. [Crossref] [PubMed]
- Lin LL, Shih YF, Hsiao CK, et al. Epidemiologic study of the prevalence and severity of myopia among schoolchildren in Taiwan in 2000. J Formos Med Assoc 2001;100:684-91. [PubMed]
- Pruett RC. Complications associated with posterior staphyloma. Curr Opin Ophthalmol 1998;9:16-22. [Crossref] [PubMed]
- Saw SM, Gazzard G, Shih-Yen EC, et al. Myopia and associated pathological complications. Ophthalmic Physiol Opt 2005;25:381-91. [Crossref] [PubMed]
- Saw SM. How blinding is pathological myopia? Br J Ophthalmol 2006;90:525-6. [Crossref] [PubMed]
- Hsu WM, Cheng CY, Liu JH, et al. Prevalence and causes of visual impairment in an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology 2004;111:62-9. [Crossref] [PubMed]
- Iwase A, Araie M, Tomidokoro A, et al. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology 2006;113:1354-62. [Crossref] [PubMed]
- Xu L, Wang Y, Li Y, et al. Causes of blindness and visual impairment in urban and rural areas in Beijing: the Beijing Eye Study. Ophthalmology 2006;113:1134.e1-11. [Crossref] [PubMed]
- Buch H, Vinding T, La Cour M, et al. Prevalence and causes of visual impairment and blindness among 9980 Scandinavian adults: the Copenhagen City Eye Study. Ophthalmology 2004;111:53-61. [Crossref] [PubMed]
- Klaver CC, Wolfs RC, Vingerling JR, et al. Age-specific prevalence and causes of blindness and visual impairment in an older population: the Rotterdam Study. Arch Ophthalmol 1998;116:653-8. [Crossref] [PubMed]
- Cotter SA, Varma R, Ying-Lai M, et al. Causes of low vision and blindness in adult Latinos: the Los Angeles Latino Eye Study. Ophthalmology 2006;113:1574-82. [Crossref] [PubMed]
- Chauvaud D. A blinding orphan disease: high myopia. Bull Acad Natl Med 2005;189:867-72; discussion 872. [PubMed]
- Ding BY, Shih YF, Lin LL, et al. Myopia among schoolchildren in East Asia and Singapore. Surv Ophthalmol 2017;62:677-97. [Crossref] [PubMed]
- Leone JF, Mitchell P, Morgan IG, et al. Use of visual acuity to screen for significant refractive errors in adolescents: is it reliable? Arch Ophthalmol 2010;128:894-9. [Crossref] [PubMed]
- Zhao J, Pan X, Sui R, et al. Refractive Error Study in Children: results from Shunyi District, China. Am J Ophthalmol 2000;129:427-35. [Crossref] [PubMed]
- Shih YF, Chen CH, Chou AC, et al. Effects of different concentrations of atropine on controlling myopia in myopic children. J Ocul Pharmacol Ther 1999;15:85-90. [Crossref] [PubMed]
- Fang YT, Chou YJ, Pu C, et al. Prescription of atropine eye drops among children diagnosed with myopia in Taiwan from 2000 to 2007: a nationwide study. Eye (Lond) 2013;27:418-24. [Crossref] [PubMed]
- Jones LA, Sinnott LT, Mutti DO, et al. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci 2007;48:3524-32. [Crossref] [PubMed]
- Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008;115:1279-85. [Crossref] [PubMed]
- Rose KA, Morgan IG, Smith W, et al. Myopia, lifestyle, and schooling in students of Chinese ethnicity in Singapore and Sydney. Arch Ophthalmol 2008;126:527-30. [Crossref] [PubMed]
- Wu PC, Tsai CL, Hu CH, et al. Effects of outdoor activities on myopia among rural school children in Taiwan. Ophthalmic Epidemiol 2010;17:338-42. [Crossref] [PubMed]
- Wu PC, Tsai CL, Wu HL, et al. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 2013;120:1080-5. [Crossref] [PubMed]
Cite this article as: Wu PC, Chang LC, Niu YZ, Chen ML, Liao LL, Chen CT. Myopia prevention in Taiwan. Ann Eye Sci 2018;3:12.


