Pediatric neuro-ophthalmology: not simply neuro-ophthalmology for small adults
Introduction
Pediatric neuro-ophthalmology is a distinct subspecialty from adult neuro-ophthalmology, despite sharing many of the same diagnoses, due to the distinctive nature of the examination, clinical presentations, and management choices. In addition, pediatric neuro-ophthalmic disorders are less commonly seen and less well understood than their adult counterparts. In fact, “Children are not simply little adults” is a frequently quoted mantra of pediatric neuro-ophthalmologists.
The aim of this manuscript is to highlight four common pediatric neuro-ophthalmic disorders by describing common clinical presentations, recommended management, and highlighting recent developments. There has been a recent surge in interest in the management of pediatric neuro-ophthalmic diseases, and therefore a rapid escalation in knowledge has taken place of late. This review will highlight both the standard clinical information required to care for these patients as well as emphasize recent novel research findings.
Pediatric idiopathic intracranial hypertension (IIH)
Epidemiology
The estimated overall annual incidence rate of IIH is approximately 0.9 per 100,000 in combined pediatric and adult populations (1-3). However, the demographics of pediatric IIH are different than that of adults. In adult patients, there is a preponderance of female gender and obesity, yet in pre-pubertal pediatric patients, there is an equal distribution of male and female gender, and obesity does not appear to be associated (4-6). Post-pubertal pediatric patients display demographic characteristics more similar to adult patients, with female gender and obesity showing a stronger association (7). Recently, Sheldon and colleagues (8) evaluated anthropometrics of pediatric IIH patients in a multi-center international cohort. Their findings revealed that younger pseudotumor patients (females under the age of 7 years and males under the age of 8.5 years) had normal height and weight, while adolescent patients were more likely to be taller and overweight, and late adolescent children were more typically obese and normal height. The anthropometrics of children with secondary IIH, when due to medication exposure or other systemic factors has not been well evaluated.
Pathophysiology
In general, the pathophysiology of IIH is related to abnormal cerebrospinal fluid (CSF) dynamics either due to impaired outflow, excessive production, or both. Although adiposity seems to be a predisposing factor for IIH in adults and post-pubertal children, it is not a driving factor in younger children. The pathophysiology in both age groups is still under investigation. One hypothesis involves a unifying mineralocorticoid pathway involving aldosterone, which includes explanations for why elevated vitamin A, obesity and growth hormone are all associated with pseudotumor in children (9). A second theory suggests that altered glucocorticoid metabolism may be the etiology (10). Recent research has revealed that pre-pubertal children with pseudotumor often have low CSF protein concentration, suggesting that increased CSF production may play a role in these children (11). Secondary IIH can be caused by a variety of identifiable causes including medications, medical conditions, structural brain abnormalities, and medication withdrawal (Table 1).
Table 1
| Medications |
| Tetracycline class of antibiotics |
| Nalidixic acid |
| Vitamin A derivatives |
| Growth hormone |
| Thyroxine |
| Lithium |
| Corticosteroids |
| Corticosteroid withdrawal |
| Medical and genetic conditions |
| Down syndrome |
| Turner syndrome |
| Renal failure |
| Anemia |
| Addison disease |
| Sleep apnea/hypercapnia |
| Vascular abnormalities |
| Cerebral venous sinus thrombosis |
| Jugular vein thrombosis or occlusion |
| Arteriovenous fistulas |
| Remote subarachnoid hemorrhage leading to decreased cerebrospinal fluid absorption |
| Hypercoagulable states |
| Antiphospholipid antibodies |
| Hyperfibrinogenemia |
| Systemic lupus erythematosus |
| Cardiac abnormalities |
| Increased right heart pressure |
| Superior vena cava syndrome |
Presentation and management
Clinical symptoms in pediatric pseudotumor patients may be similar to those found in adult patients such as headache, nausea, vomiting, diplopia, transient visual obscuration and pulsatile tinnitus. However, unlike their adult counterparts, pediatric patients can also commonly present with vague symptoms such as irritability or change in behavior, or they may also present without any symptoms in up to 30% of cases (7). Pediatric patients are often referred for evaluation after papilledema or an ocular motility disturbance are noted on routine examination.
Neuro-ophthalmic examination of pediatric patients frequently shows ocular motility abnormalities such as sixth nerve palsies, occurring in 10-40% of patients, or less commonly comitant esotropia or third or fourth cranial nerve palsies (5,7). By far the most common clinical exam finding in these patients is papilledema, which is seen in the majority of cases. Diagnostic criteria for IIH have recently been updated in 2013 (12) in order to include common radiologic characteristics of increased intracranial pressure as well as recent data regarding normal CSF pressure in children. These criteria include (12):
- Definite IIH
- Papilledema;
- Normal MRI or CT of the brain parenchyma;
- Normal venous system on MRV or CTV;
- Normal CSF composition;
- Elevated intracranial pressure by lumbar puncture (>28 cm water for pediatric patients, >25 cm water if patient is not sedated or obese) or;
- Lack of papilledema with presence of sixth nerve palsy and #2–5 from above.
- Probable IIH
- All characteristics of definite IIH except normal measured intracranial pressure by lumbar puncture.
- Suggested IIH
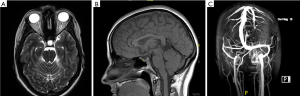
- Lack of papilledema and lack of sixth nerve palsy but presence of #2–5 and neuroimaging findings (Figure 1) such as distension of the perioptic subarachnoid space with or without optic nerve tortuosity, flattening of the posterior aspect of the globe, empty sella, and transverse venous sinus stenosis.
Given the above diagnostic criteria, MRI of the brain combined with MRV is indicated for all cases of suspected IIH syndrome in children. Several recent studies have delved into the MRI findings in children with IIH (13-16). These studies have shown that the most common finding on MRI is optic nerve sheath enlargement (64%) and tortuosity (30–90%) followed by intraocular protrusion of the optic nerve (17–27%), empty sella (26%) and flattening of the posterior globe (45–60%) (13,17). After the MRI/MRV is performed, a lumbar puncture is then indicated both to determine the intracranial pressure and to ensure a normal CSF profile. In addition, recent research has suggested a role for other ancillary tests such as optical coherence tomography (OCT) of the optic nerve and macula. OCT has been suggested as a surrogate for subsequent lumbar puncture in cases where response to treatment is unclear. For example, one study found that optic atrophy and photoreceptor dropout were highly correlated with vision loss and progression of disease (18). A similar study indicated that increased retinal nerve fiber layer (rNFL) and macular thickness can be seen by OCT and used as a tool for assessing and monitoring disease (19). Despite these findings, the optimal OCT parameters for use in monitoring disease progression are still debatable and may include the amount of inward deflection of Bruch membrane (20,21), the macular ganglion cell layer inner plexiform layer (20), optic nerve volume (22), or the retinal nerve fiber layer.
Once the diagnosis of IIH is established, treatment is based on the severity of the individual patient’s presentation. Treatment goals include alleviation of symptoms such as headache, diplopia, and visual changes as well as prevention of permanent vision loss from papilledema. Typically, asymptomatic patients with normal visual acuity and visual fields can be managed conservatively with observation or low dose acetazolamide. In addition, in cases of secondary IIH, the predisposing factor must also be addressed. In cases where there are bothersome symptoms or mild visual compromise, medical management with acetazolamide 15–25 mg/kg/day divided into two or three dosages, increasing as necessary up to 100 mg/kg/day (up to 2 grams per day) is typically the first line therapy. If acetazolamide is not tolerated due to side effects, then alternative medications such as topiramate and furosemide can be considered. Medications can be tapered once the papilledema resolves and the visual field normalizes. Frequent monitoring of visual acuity, visual field and optic nerve appearance is crucial to avoid untreated worsening of disease. In fulminant or severe acute cases, occasionally surgical intervention is required. As a temporizing measure in some patients, intravenous steroids are utilized in attempt to minimize severe visual loss. Surgical intervention may include optic nerve sheath fenestration or CSF shunting depending on the patient’s symptomatology as well as the preference of the treating center. In all cases, attention should be given to the patient’s body mass index and weight loss encouraged in cases of obesity or overweight status.
Future directions
The Idiopathic Intracranial Hypertension Treatment Trial was the first randomized controlled trial for treatment of IIH in adults (23). Although no children were enrolled in this study, the data gleaned from it may have important implications for pediatric patients. For example, this study determined that worse visual acuity or papilledema at presentation was associated with worse outcomes—this could possibly be extrapolated to children and may encourage clinicians to treat these patients more aggressively at disease onset. In addition, on the horizon for the management of IIH are more studies evaluating the use of various OCT parameters to monitor and diagnose IIH, potentially avoiding invasive testing such as lumbar puncture. Lastly, the pathophysiology of IIH must still be elucidated in order to create relevant treatments especially in those patients with the most severe presentations.
Pediatric pseudopapilledema and optic disk drusen (ODD)
Epidemiology
Pseudopapilledema in children is a common diagnosis on the differential diagnosis of possible papilledema. A common cause of pseudopapilledema is ODD, which are benign congenital deposits in the optic nerve head. ODD are most commonly buried in the substance of the optic nerve head, and therefore not clearly visible in pediatric patients. Pseudopapilledema may be mistaken for true papilledema in up to 76% of cases (24), leading to unnecessary, expensive and invasive testing. Therefore, it is crucial for ophthalmologists to be able to differentiate true papilledema from pseudopapilledema. The prevalence of ODD in children is estimated at approximately 0.4%; however, in adults estimates are higher and range from 0.5% to 2.4%, probably because they are easier to detect in adults (25-27). ODD prevalence also varies by race, with a higher prevalence in white patients (28). ODD tend to occur more commonly in children with a family history of ODD and may be inherited as part of genetic syndromes such as retinitis pigmentosa, pseudoxanthoma elasticum (29,30), and Alagille syndrome (31).
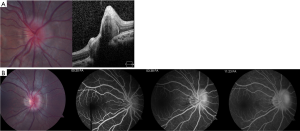
ODD appear different in pediatric patients compared to adults. In children, ODD are frequently buried within the substance of the optic nerve (Figure 2) while in adults, they are situated on the surface of the disk and are often calcified. Due to these differences in appearance, ODD in children is more difficult to visualize and diagnose.
Pathophysiology
The exact cause of ODD is not known but there are several theories proposed to explain their presence. The two most commonly accepted theories are that the drusen are caused by (I) a disturbance of axonal metabolism with slow axoplasmic flow (32,33) or (II) congenitally small or dysplastic disks with a propensity for altered axoplasmic flow and subsequent drusen formation (34,35). The unifying feature of many hypotheses is that patients with drusen are anatomically predisposed due to a small scleral canal (or disturbed axonal flow in cases of normal-sized scleral canals) (25).
Presentation and management
ODD in children are almost always found incidentally on routine eye examination, as the majority of cases are asymptomatic. Previous series have revealed that approximately half of children evaluated for ODD present with symptoms of increased ICP such as headache, nausea, or vomiting, while the other half of patients are diagnosed as part of an ophthalmic examination for unrelated issues (36). Rarely, children can present with symptoms from ODD that can include transient visual obscuration or visual field defects (37-39). Visual field defects occur with increasing frequency as the age of the patient increases, as visual field defects are more commonly seen with surface drusen (40,41). The incidence of visual field defects in young (<10 years) patients with ODD is estimated at 11% compared to 51% in older children (28). The most common visual field defect seen in these cases are nasal steps, arcuate defects, enlarged blind spots, and generalized constriction (38). Aside from visual field defects, possible examination findings in children with ODD include anomalous retinal vasculature, disk hemorrhage, relative afferent pupillary defect and very rarely choroidal neovascular membrane.
The difficulty in the management of children with pseudopapilledema is differentiating their presentation from true papilledema. For this reason, there are many studies evaluating various diagnostic tests in attempt to determine the most accurate way to differentiate these diagnoses without requiring expensive or invasive tests such as MRI or lumbar puncture. Ancillary tests vary in their level of accuracy in differentiating true edema from pseudopapilledema in children (Table 2).
Table 2
| Diagnostic test | Buried (%) | Surface (%) |
|---|---|---|
| Fundus autofluorescence | 56 | 100 |
| Fluorescein angiography | 95 | 100 |
| Optical coherence tomography | SD: 82 | SD: 100 |
| EDI: 76 | EDI: 100 | |
| RNFL: 79 | RNFL: 67 | |
| B-scan ultrasonography | 84 | 100 |
*, data from Chang
B-scan ultrasonography
B-scan ultrasonography is an inexpensive and non-invasive modality that is very useful in diagnosing ODD in adults (43,44). The diagnosis is based upon a hyperechoic mass within the substance of the optic nerve associated with posterior shadowing. However, this finding is only seen when ODD are calcified, and therefore has been found to have a sensitivity of approximately 48% in adult populations (43). The sensitivity in children is likely lower due to the lack of calcifications; however, in a recent pediatric study, B-scan was found to have a 74% accuracy in differentiating true papilledema from pseudopapilledema (42).
Fundus autofluorescence
ODD tend to autofluoresce on pre-injection control photography and scanning laser ophthalmoscopy (28). Similar to B-scan, autofluorescence has a higher utility in surface, calcified ODD as the autofluorescent nature of buried drusen is obscured by the overlying optic nerve tissue. In children with surface drusen confirmed by B-scan, autofluorescence is 94% sensitive (45). However, in studies that did not require B-scan confirmation (and are therefore likely to include more children with buried drusen), the detection of buried drusen by autofluorescence ranged from 27–56% (42,43).
Fluorescein angiography (FA)
FA is a useful but more invasive test that is often helpful in differentiating true from pseudopapilledema. ODD demonstrate several common characteristics on FA, including optic disk staining, delayed filling of the peripapillary choriocapillaris, lack of early or late disk leakage, and staining of the ODD (Figure 2) (46). FA has been shown to have the highest accuracy (97%) of all tested modalities in differentiating ODD from true papilledema in a recent study of pediatric patients (42). Limitations of FA include the need for intravenous injection which may be obviated by the use of oral fluorescein (47).
OCT
There has been a surge of interest in the use of OCT to diagnose ODD and differentiate it from true papilledema. Modalities of OCT that have been suggested include retinal nerve fiber layer analysis and direct visualization using enhanced depth imaging (EDI) or swept source OCT. On OCT, ODD appear as focal masses with a hyporeflective core and hyperreflective border (Figure 2). There has been some controversy as to whether OCT is able to accurately differentiate ODD from true papilledema. Recently, the Optic Disc Drusen Studies Consortium has published recommendations for the diagnosis of ODD using OCT (48). Their recommendations include a standardized protocol for pre-scanning and acquisition of scans, and specify specific parameters for dense optic nerve scans, radial optic nerve scans, peripapillary scans, and macula scans (48). The purpose of these recommendations is to establish reliable and consistent diagnosis of ODD both for researchers and clinicians. Although their recommendations are crucial, they may not be directly applicable to pediatric patients as their standardization steps were based on adult patients with less than 50% harboring buried drusen (vs. surface drusen). Their findings suggest that on EDI OCT, ODD are always located above the lamina cribosa, have a signal-poor core and are often seen with a hyperreflective margin (48).
Studies that have focused specifically on pediatric patients have shown conflicting results as to whether OCT is useful in differentiating ODD from papilledema. In one series, EDI OCT detected 17/25 cases of buried ODD (49). In a more recent study of EDI-OCT in pediatric patients, the accuracy was 67% for differentiating papilledema from ODD (42).
Studies comparing various diagnostic modalities
Few studies have compared various modalities for the diagnosis of ODD (42,43). Recently, Chang et al. published a study comparing B-scan, autofluorescence, FA, and OCT in the differentiation of pediatric pseudopapilledema and true papilledema cases (42). The findings of this study (Table 2) revealed that FA had the highest diagnostic accuracy in differentiation the two entities (97%), followed by ultrasonography (74%), OCT (67–71%), fundus photography (66%), and autofluorescence (62%).
Complications and management
Despite ODD being a benign entity, there are rare complications that may cause loss of vision in some patients. As discussed above, visual field defects occur in some children with ODD and increase with age. ODD may also be associated with vascular complications such as hemorrhages (50-52), choroidal neovascular membrane (53), vascular occlusions and even ischemic optic neuropathy (54). These vascular complications are rare but have been reported.
Given the risk of visual field defects and other rare complications, it is recommended that children with ODD undergo at least annual ophthalmic examinations and visual field testing. In cases where visual field loss is detected, one can consider ocular hypotensive drops although no studies have been performed to support this recommendation (28). Clinicians must keep in mind that alpha agonists are contraindicated in young children due to the risk of respiratory depression.
Future directions
Several groups have also identified changes in the Bruch’s membrane opening on OCT as an aid to differentiating true papilledema from pseudopapilledema (18,55,56). This area is still one of active investigation but appears promising in that the horizontal diameter of the Bruch membrane opening appears enlarged in patients with true papilledema compared to pseudopapilledema patients. In addition, future studies may evaluate neuroprotective agents for use in ODD patients who appear at risk for visual field loss.
Pediatric optic neuritis (ON)
Epidemiology
ON is a clinical diagnosis defined as an idiopathic, demyelinating inflammatory condition of the optic nerve. Non-idiopathic cases, such as those caused by autoimmune and inflammatory disorders like sarcoidosis or systemic lupus erythematosus are often grouped into the same diagnostic categories. Pediatric ON may occur in isolation or as part of an inflammatory central nervous system disorder such as acute disseminated encephalomyelitis (ADEM), multiple sclerosis (MS) or neuromyelitis optica (NMO), and it accounts for approximately 25% of acute demyelinating events in children (57). The overall incidence of pediatric ON has been estimated at 0.2 per 100,000 in Canada (57). In pre-pubertal children, there does not appear to be a gender predilection; however, in post-pubertal children, there is a preponderance of female patients (58,59).
Presentation and management
The typical presentation of pediatric ON includes decreased visual acuity, dyschromatopsia, and visual field defects. Unilateral or bilateral involvement may occur, and bilateral involvement may be simultaneous (within 2 weeks) or sequential (2–12 weeks). Bilateral involvement is more common in younger children (72% <10 years) than in older children (30%) (60). Pain with eye movements or headache is a presenting symptom in 30–77% of patients (61-64). The most common visual field defects in those patients who are able to perform automated visual field testing are central or cecocentral scotoma (61,65).
Visual acuity at presentation may be relatively normal with approximately 20% of children presenting with visual acuity better than 20/40. More commonly, it is severely affected, with 60% of children presenting with VA worse than 20/200 (64,66). In case series that include only pre-pubertal children, visual acuity at presentation is worse, with approximately 90% of children presenting with VA worse than 20/200 (67). Common examination features include optic disk edema (40–70%) (61,64,68), relative afferent pupillary defect, or optic nerve pallor if recurrent or late stage. Long-term outcomes after ON in children are typically favorable. Most (58–97%) children recover visual acuity better than 20/40 (58,64,66,69), and in the most recent study of children requiring a minimum of one-year follow up, 89% of patients recovered vision better than 20/40 at 1 year (63). Structural rNFL outcomes vary depending on the underlying etiology, with ADEM patients faring the worst (70).
There are several important differences between pediatric and adult patients with ON. With regard to presentation, adult patients more frequently present with pain on eye movements than children (90% vs. 53%) (68). In addition, the majority of adult patients present with unilateral retrobulbar involvement, in contrast to pediatric patients who typically present with bilateral optic nerve edema (one-third vs. 40–70%) (61,66,71). Presenting VA is typically better in adults than children, with 36% of adults in the Optic Neuritis Treatment Trial presenting with VA worse than 20/200 compared to 90% of pre-pubertal ON patients (67,72).
Although ON is a clinical diagnosis, it requires a work-up to rule out other causes of optic disk edema in children (Table 3).
Table 3
| Demyelinating optic neuritis |
| Acute disseminated encephalomyelitis (ADEM) |
| Neuromyelitis optica spectrum disorder(NMOSD) |
| Multiple sclerosis (MS) |
| Isolated optic neuritis (post-viral, post-vaccine) |
| Systemic rheumatologic condition |
| Systemic lupus erythematosus |
| Sarcoidosis |
| Small vessel vasculitis |
| Chronic relapsing inflammatory optic neuropathy |
| Genetic optic atrophy e.g., Leber hereditary optic neuropathy |
| Infectious etiologies |
| Syphilis |
| Lyme |
| Bartonella |
| Toxoplasma |
| Orbital cellulitis |
| Sinusitis |
| Infiltrative disease |
| Leukemia |
| Lymphoma |
| Papilledema |
| Pseudopapilledema |
| Non-accidental trauma |
| Optic nerve or nerve sheath tumor e.g., meningioma, glioma |
Typical investigations include magnetic resonance imaging (MRI) of the brain and orbits as well as a lumbar puncture with opening pressure, CSF analysis for protein, glucose, cells, oligoclonal bands, IgG index and cultures. MRI testing typically reveals optic nerve thickening on T1-weighted images and bright signal on T2-weighted images. Of note, lumbar puncture opening pressure may be elevated in cases of ON, occasionally causing difficulty in differentiating bilateral ON from IIH (73,74). Laboratory testing can be guided by the presentation but typically includes testing for biomarkers of sarcoidosis, tuberculosis, syphilis, Lyme disease, Bartonella henselae infection, and systemic lupus erythematosus. If there is suspicion for NMO, an MRI of the spine as well as aquaporin-4 testing can be performed.
Associated neurologic and inflammatory syndromes
ON in children may be an isolated monophasic event or it may be post-infectious, inflammatory or part of a systemic demyelinating disorder. In younger children, ON is more likely to occur as a post-viral or post-vaccination syndrome or in association with ADEM, while older children tend to present more commonly as an initial manifestation of a systemic demyelinating disease such as MS or NMO.
Isolated ON is more common in children than adults and is often associated with an antecedent viral infection, vaccination or non-viral infection such as Lyme disease or Mycoplasma pneumonia (59,75). Recurrent ON in children without anti-aquaporin-4 antibody positivity may be associated with positive oligoclonal bands or anti-MOG. Recurrent ON in isolation is uncommon, occurring in 5% of Canadian pediatric ON patients (57). Multiple recurrences of ON that are associated with objective loss of visual function, negative anti-NMO status, and are responsive to steroids, with relapse upon their withdrawal may be known as chronic relapsing inflammatory optic neuropathy (CRION).
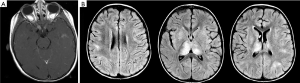
ADEM is a monophasic (typically) multifocal acute demyelinating disease that presents mostly in prepubertal children typically following a viral illness or vaccination (76). ADEM is characterized by encephalopathy, fever, and meningeal signs as well as MRI findings of T2 and flair hyperintense large white matter lesions characterized by uniformity in time of onset (Figure 3) (77). ADEM is typically differentiated from MS by its lack of dissemination in time and lack of recurrence although multi-phasic ADEM does rarely occur (76).
MS in children is diagnosed similarly to adults, using the McDonald criteria. However, when children present with ON prior to the age of 12 years, the positive predictive value of the McDonald criteria is lower (76). ON is the presenting feature of MS in 10–20% of pediatric MS cases (78). The risk of developing MS after an initial episode of ON is highly dependent on the age at presentation, MRI findings, and CSF findings (OCB positivity) Although it is estimated that 13–36% of pediatric patients presenting with ON will eventually be diagnosed with MS (62,66,71), this risk is highly dependent on the age at presentation as well as the presence or absence of white matter lesions on the initial brain MRI (64,71). For every 1-year increase in age, it has been estimated that there is a 32% increased risk of MS. In addition, a recent meta-analysis revealed that the presence of one white matter lesion on brain MRI increased the odds ratio of an eventual diagnosis of MS to 28.0 (60). In a European study, the hazard ratio for MS was 1.08/year of age (79). However, the risk of MS also depends upon racial and geographic features (59).
NMO is traditionally characterized by ON and transverse myelitis with characteristic MRI findings of longitudinally extensive optic nerve and transverse myelitis lesions. A recent revision of the international consensus diagnostic criteria for NMO spectrum disorder was categorized by anti-aquaporin-4 antibody status, and included the presence of hyperintense optic nerve lesions on T2-weighted imaging (or T1-weighted gadolinium enhancing lesions) extending more than 50% of the length of the optic nerve and transverse myelitis lesions spanning at least 3 contiguous spinal segments (80). The consensus group noted that spinal lesions are less diagnostic in children as they can also occur in ADEM and pediatric MS. ON associated with NMO in children is frequently associated with poorer visual outcomes with the median time from onset of NMO to severe vision loss of <20/200 estimated to be only 1.3 years (81).
Treatment
The decision to treat pediatric ON varies amongst physicians and is often dependent upon the age of the patient, systemic comorbidities laterality, MRI findings, and severity of vision loss. Acute treatment typically includes the administration of corticosteroids, commonly intravenous methylprednisolone for a course of 3–5 days (20–30 mg/kg/day up to 1 g/day) extrapolated from the adult ON treatment trial (82). Whether a longer (>2 weeks) vs. shorter (<2 weeks) oral steroid taper affects outcome is still debatable (83). Since there are no prospective randomized trials, it is unclear what benefit corticosteroid treatment in general may provide in the long-term. In cases of severe steroid-resistant ON, IVIG and plasma exchange can be considered. If a diagnosis of MS or NMO is made, systemic disease-modifying therapy is recommended.
Future directions
Several ancillary tests are still under investigation for their utility in the diagnosis and management of pediatric ON. For example, OCT measurements of the rNFL and ganglion cell layer may have a role in long-term follow up for patients with and without MS (84-86). Structure-function studies will help to determine the patient-related nature of these findings. Additionally, anti-myelin oligodendrocyte glycoprotein antibody (anti-MOG), an antibody that is prevalent in younger ON patients with encephalopathy, may be a useful adjunct test in cases where the presentation is not typical for MS, ADEM or NMO (87). Preliminary studies have shown that anti-MOG positivity may be associated with better outcomes compared to other demyelinating diseases in children (88,89). The relationship between anti-MOG antibody and ADEM as well as recurrent ON in children remains to be examined.
The lack of prospective data on the natural history and treatment of children with ON limits our ability to practice evidence-based management in these cases. A recently launched collaborative study between the Pediatric Eye Disease Investigator Group (PEDIG) and the Neuro Ophthalmology Research Disease Investigator Consortium (NORDIC) aims to enroll 100 children with acute ON amongst 45 sites over a period of 2 years. This prospective data collection study will determine the group’s ability to enroll children for a potential future prospective treatment study as well as to estimate visual acuity outcomes at 6 months, and numerous secondary outcomes such as quality of life metrics, OCT, low contrast acuity, MRI findings and NMO antibody status.
Pediatric optic pathway gliomas (OPG)
Epidemiology
OPG are low-grade glial neoplasms composed of astrocytes involving the visual pathway anywhere along the path from the optic nerves to the optic radiations. OPGs are typically diagnosed based on their characteristic appearance on neuroimaging (see below) but have also been examined pathologically. The histological appearance of these tumors is benign and includes Type 1 astrocytes with similar molecular genetic makeup to other low-grade astrocytomas in the CNS (90-93). Recent debate in the literature as to whether these tumors should be considered “benign hamartomas” instead of “pilocytic astrocytomas” has been discussed; most experts agree that the identical molecular make-up of the tumors to other CNS astrocytomas as well as their immunohistochemical profile determines that the most accurate name for the lesions is pilocytic astrocytoma (93).
OPGs are relatively common in children with neurofibromatosis-1 (NF1) occurring in 15–20% of them, but in the general population are more rare, accounting for approximately 1% of all intracranial tumors and 3–5% of pediatric brain tumors (93,94). The majority (70%) of OPGs present in the first decade of life (median age 6.5 years) although rarely elderly patients have been reported to present with a seemingly new onset OPG (95-97).
Presentation and management
The clinical presentation of OPGs is dependent upon the age at presentation, laterality and location of the lesion. Unilateral anterior optic nerve gliomas are typically associated with decreased visual acuity, dyschromatopsia, and visual field defects. Examination findings may include a relative afferent pupillary defect, proptosis, strabismus, or optic disk edema. More posterior optic nerve tumors may present more insidiously with optic atrophy and less external findings. OPGs of the chiasm are frequently diagnosed later than anterior tumors since there are less external features, and the visual loss is more peripheral and has a slower onset. Visual loss is bilateral and typically associated with bitemporal hemianopia. Hemianopic defects in these cases are typically asymmetric and many patients present with a junctional scotoma, with central vision loss in one eye and a temporal field defect in the fellow eye. Examination findings include optic atrophy and rarely proptosis if the tumor extends anteriorly into one or both optic nerves. Other possible presenting examination findings include sensory strabismus, asymmetric nystagmus, and hypothalamic dysfunction. Nystagmus associated with chiasmal gliomas can occasionally appear similarly to spasmus nutans with an asymmetric horizontal shimmering waveform.
Anterior OPGs are typically diagnosed based on neuroimaging characteristics which include fusiform enlargement and kinking of the optic nerve. OPGs are iso- or hypointense on T1-weighted imaging with enhancement after IV contrast administration, and are hyperintense on T2-weighted images. These imaging characteristics are consistent across all possible locations of OPGs. In diagnosing OPGs, it is important to look for other MRI findings seen in NF1 if the patient’s NF1-status is not known. These findings may include focal areas of abnormal signal intensity (previously known as “unidentified bright objects”) which are thought to be the result of neural dysplasia or dysmyelination with associated focal edema (98). In addition, physical examination should include an assessment for other findings seen in patients with NF1 such as café-au-lait spots, neurofibromas, axillary or inguinal freckling, Lisch nodules, and bone changes such as bowing of the long bones, and a genetics consultation if indicated.
Once diagnosed, the natural history of OPGs is typically characterized by slow growth, minimal effect on visual acuity, and exceedingly rare potential for malignant transformation (93). Interestingly, OPGs that are isolated and not associated with NF1 seem to have a more aggressive course with worse visual outcomes. Children with sporadic OPGs have an approximate rate of vision loss of 70% while patients with NF1-related OPGs have a lower rate of vision loss of approximately 25% (99-105). Isolated optic nerve lesions are known to be associated with the presence of some cells in the chiasm, even if not visible radiographically (106). However, the risk of radiographically visible progression of an isolated optic nerve tumor to “invade” the chiasm is rare, occurring in 7 of 35 patients followed in a national clinical trial (107). Negative prognostic factors for visual acuity that have been posited but not confirmed in a large randomized trial include female gender, earlier age of presentation (108), and more anterior location of the tumor (99,109-113). Chiasmal gliomas are typically less aggressive than optic nerve tumors, but may be associated with more systemic complications such as hypopituitarism. The most posterior lesions (optic tract and radiations) appear to be the least aggressive lesions in terms of growth (99,111-113).
The management of OPGs is still controversial as their natural history is not completely agreed upon, and there are case reports of spontaneous improvement (114). However, treatment is indicated to reduce visual morbidity in children who are at risk. Furthermore, in patients with NF1, it has been shown that vision loss, endocrinopathy, impaired social interactions, and difficulties with activities of daily living are all associated with OPGs (115). Recently, there has been a paradigm shift away from tumor size increase as an indication for treatment, with more emphasis placed on visual acuity loss (or its biomarkers) as the primary indication for treatment (115). Although there is no clear consensus for treatment indications, most clinicians agree that the best indication for treatment is significant vision loss (a change of 0.2 logMAR or progression of visual field defects) (115). Other less common scenarios that may indicate the need for treatment include abnormal vision in the fellow eye of an already blind eye, suspected vision loss in the absence of an obtainable visual acuity, or visual acuity at or near a functional threshold (100,115). Tumor growth without a change in visual acuity does not indicate a need for treatment; however, progression on MRI along with changes to the physical examination may be an indication for closer surveillance or treatment.
The first line treatment for OPGs is typically chemotherapy, as radiation carries a risk of secondary malignancy, moyamoya-like disease and neurocognitive deterioration in young children. Common chemotherapeutic options include vincristine, vinblastine, carboplatin, temozolomide, and most recently bevacizumab (116). Surgery is reserved for extreme cases, such as physical deformity or encroachment onto vital CNS structures. Despite the use of chemotherapy in children with progressive vision loss, some children continue to deteriorate with 28% of children deteriorating by at least 2 logMAR lines after the completion of chemotherapy in one study (110).
Surveillance and ancillary testing
In patients with NF1 without a known OPG, current recommendations include a yearly comprehensive ophthalmologic examination assessing VA, visual fields, pupillary testing, eye movements, and fundus examination annually until the age of 8 years and then every other year until 18 years of age (100). In those NF1 patients with known associated OPGs, the current recommendation for surveillance by ophthalmology and MRI is every 3 months for the first year and then every 6 months for 2 years and after the age of 8 years, and then annually until 18 years of age (MRI can be less frequent after the first 5 years if there is no progression) (115). Visual acuity testing should be performed when possible using age-appropriate optotypes. However, given the variable nature of visual acuity testing in children, investigators have sought other biomarkers for vision loss. Modalities that have received recent attention include visual evoked potential (117-119), OCT (120-124), diffusion tensor imaging (125,126), and volumetric MRI (127). The two most promising of these modalities appear to be OCT for anterior lesions and diffusion tensor imaging for lesions of the optic tract and radiations.
OCT has been demonstrated to reveal reduced rNFL in children with OPGs, with an apparent threshold near 80 µm, below which patients are more likely to have abnormal visual function (VA or visual field). This threshold may be potentially useful in children who cannot participate with VA testing. Longitudinal studies have also reported the utility of OCT in diagnosing vision loss from OPGs, with a 10% decrease in rNFL thickness indicating vision loss with 70% sensitivity. The overall role of OCT in the management of patients with OPG is still under investigation. Diffusion tensor imaging is an MRI technique that is useful in diagnosing white matter damage. This technique has been shown in a recent study to correlate with vision loss in patients with OPGs of the optic radiations (115). In a small study, this technique was also useful in predicting visual acuity change one year after imaging (126).
Future directions
A multicenter NF1-OPG study examining the natural history of OPGs has recently launched. This study will help to define visual acuity outcomes as well as biomarkers that may be useful in future treatment trials. In addition, a randomized treatment trial comparing vinblastine and bevacizumab to vinblastine alone has also recently been launched. Subsequent treatment trials comparing various modalities are likely to follow suit. Our understanding of the molecular alterations that underlie OPGs has led to the establishment of newer targeted treatments such as mitogen-activated protein kinase (MEK) inhibitors. Future trials will delineate whether MEK inhibitors, as well as other therapies such as mammalian target of rapamycin complex (mTOR) inhibitors and farnesyl transferase inhibitors are effective the treatment of these tumors (128).
Acknowledgments
Research to Prevent Blindness, Unrestricted Grant: SL Pineles.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Karl C. Golnik and Andrew G. Lee) for the series “Neuro-ophthalmology” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.03.01). The series “Neuro-ophthalmology” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bursztyn LL, Sharan S, Walsh L, et al. Has rising pediatric obesity increased the incidence of idiopathic intracranial hypertension in children? Can J Ophthalmol 2014;49:87-91. [Crossref] [PubMed]
- Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. Arch Neurol 1988;45:875-7. [Crossref] [PubMed]
- Gordon K. Pediatric pseudotumor cerebri: descriptive epidemiology. Can J Neurol Sci 1997;24:219-21. [Crossref] [PubMed]
- Cinciripini GS, Donahue S, Borchert MS. Idiopathic intracranial hypertension in prepubertal pediatric patients: characteristics, treatment, and outcome. Am J Ophthalmol 1999;127:178-82. [Crossref] [PubMed]
- Phillips PH, Repka MX, Lambert SR. Pseudotumor cerebri in children. J AAPOS 1998;2:33-8. [Crossref] [PubMed]
- Rangwala LM, Liu GT. Pediatric idiopathic intracranial hypertension. Surv Ophthalmol 2007;52:597-617. [Crossref] [PubMed]
- Balcer LJ, Liu GT, Forman S, et al. Idiopathic intracranial hypertension: relation of age and obesity in children. Neurology 1999;52:870-2. [Crossref] [PubMed]
- Sheldon CA, Paley GL, Xiao R, et al. Pediatric Idiopathic Intracranial Hypertension: Age, Gender, and Anthropometric Features at Diagnosis in a Large, Retrospective, Multisite Cohort. Ophthalmology 2016;123:2424-31. [Crossref] [PubMed]
- Salpietro V, Polizzi A, Berte LF, et al. Idiopathic intracranial hypertension: a unifying neuroendocrine hypothesis through the adrenal-brain axis. Neuro Endocrinol Lett 2012;33:569-73. [PubMed]
- Sinclair AJ, Onyimba CU, Khosla P, et al. Corticosteroids, 11beta-hydroxysteroid dehydrogenase isozymes and the rabbit choroid plexus. J Neuroendocrinol 2007;19:614-20. [Crossref] [PubMed]
- Margeta MA, Buckley EG, El-Dairi MA. Low cerebrospinal fluid protein in prepubertal children with idiopathic intracranial hypertension. J AAPOS 2015;19:135-9. [Crossref] [PubMed]
- Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 2013;81:1159-65. [Crossref] [PubMed]
- Hirfanoglu T, Aydin K, Serdaroglu A, et al. Novel Magnetic Resonance Imaging Findings in Children With Intracranial Hypertension. Pediatr Neurol 2015;53:151-6. [Crossref] [PubMed]
- Gorkem SB, Doganay S, Canpolat M, et al. MR imaging findings in children with pseudotumor cerebri and comparison with healthy controls. Childs Nerv Syst 2015;31:373-80. [Crossref] [PubMed]
- Dwyer CM, Prelog K, Owler BK. The role of venous sinus outflow obstruction in pediatric idiopathic intracranial hypertension. J Neurosurg Pediatr 2013;11:144-9. [Crossref] [PubMed]
- Shofty B, Ben-Sira L, Constantini S, et al. Optic nerve sheath diameter on MR imaging: establishment of norms and comparison of pediatric patients with idiopathic intracranial hypertension with healthy controls. AJNR Am J Neuroradiol 2012;33:366-9. [Crossref] [PubMed]
- Lim MJ, Pushparajah K, Jan W, et al. Magnetic resonance imaging changes in idiopathic intracranial hypertension in children. J Child Neurol 2010;25:294-9. [Crossref] [PubMed]
- Gospe SM 3rd, Bhatti MT, El-Dairi MA. Anatomic and visual function outcomes in paediatric idiopathic intracranial hypertension. Br J Ophthalmol 2016;100:505-9. [Crossref] [PubMed]
- El-Dairi MA, Holgado S, O'Donnell T, et al. Optical coherence tomography as a tool for monitoring pediatric pseudotumor cerebri. J AAPOS 2007;11:564-70. [Crossref] [PubMed]
- Chen JJ, Trobe JD. Optical Coherence Tomography Should Be Used Routinely to Monitor Patients With Idiopathic Intracranial Hypertension. J Neuroophthalmol 2016;36:453-9. [Crossref] [PubMed]
- OCT Sub-Study Committee for NORDIC Idiopathic Intracranial Hypertension Study Group. Baseline OCT measurements in the idiopathic intracranial hypertension treatment trial, part I: quality control, comparisons, and variability. Invest Ophthalmol Vis Sci 2014;55:8180-8. [Crossref] [PubMed]
- Optical Coherence Tomography Substudy Committee. Papilledema Outcomes from the Optical Coherence Tomography Substudy of the Idiopathic Intracranial Hypertension Treatment Trial. Ophthalmology 2015;122:1939-45.e2. [Crossref] [PubMed]
- Committee NIIHSGW, Wall M, McDermott MP, et al. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. JAMA 2014;311:1641-51. [Crossref] [PubMed]
- Kovarik JJ, Doshi PN, Collinge JE, et al. Outcome of pediatric patients referred for papilledema. J AAPOS 2015;19:344-8. [Crossref] [PubMed]
- Auw-Haedrich C, Staubach F, Witschel H. Optic disk drusen. Surv Ophthalmol 2002;47:515-32. [Crossref] [PubMed]
- Erkkila H. Clinical appearance of optic disc drusen in childhood. Albrecht Von Graefes Arch Klin Exp Ophthalmol 1975;193:1-18. [Crossref] [PubMed]
- Erkkila H, Raitta C, Niemi KM. Ocular findings in four siblings with pseudoxanthoma elasticum. Acta Ophthalmol (Copenh) 1983;61:589-99. [Crossref] [PubMed]
- Chang MY, Pineles SL. Optic disk drusen in children. Surv Ophthalmol 2016;61:745-58. [Crossref] [PubMed]
- Mansour AM. Is there an association between optic disc drusen and angioid streaks? Graefes Arch Clin Exp Ophthalmol 1992;230:595-6. [Crossref] [PubMed]
- Pierro L, Brancato R, Minicucci M, et al. Echographic diagnosis of Drusen of the optic nerve head in patients with angioid streaks. Ophthalmologica 1994;208:239-42. [Crossref] [PubMed]
- Nischal KK, Hingorani M, Bentley CR, et al. Ocular ultrasound in Alagille syndrome: a new sign. Ophthalmology 1997;104:79-85. [Crossref] [PubMed]
- Spencer WH. Drusen of the optic disk and aberrant axoplasmic transport. The XXXIV Edward Jackson memorial lecture. Am J Ophthalmol 1978;85:1-12. [Crossref] [PubMed]
- Tso MO. Pathology and pathogenesis of cystoid macular edema. Ophthalmologica 1981;183:46-54. [Crossref] [PubMed]
- Mustonen E, Kallanranta T, Toivakka E. Neurological findings in patients with pseudopapilloedema with and without verified optic disc drusen. Acta Neurol Scand 1983;68:218-30. [Crossref] [PubMed]
- Sacks JG, O'Grady RB, Choromokos E, et al. The pathogenesis of optic nerve drusen. A hypothesis. Arch Ophthalmol 1977;95:425-8. [Crossref] [PubMed]
- Erkkila H. Optic disc drusen in children. Acta Ophthalmol Suppl 1977;3-44. [PubMed]
- Lorentzen SE. Drusen of the optic disk. A clinical and genetic study. Acta Ophthalmol (Copenh) 1966;1-180. [PubMed]
- Noval S, Visa J, Contreras I. Visual field defects due to optic disk drusen in children. Graefes Arch Clin Exp Ophthalmol 2013;251:2445-50. [Crossref] [PubMed]
- Sarkies NJ, Sanders MD. Optic disc drusen and episodic visual loss. Br J Ophthalmol 1987;71:537-9. [Crossref] [PubMed]
- Mustonen E. Pseudopapilloedema with and without verified optic disc drusen. A clinical analysis I. Acta Ophthalmol (Copenh) 1983;61:1037-56. [Crossref] [PubMed]
- Savino PJ, Glaser JS, Rosenberg MA. A clinical analysis of pseudopapilledema. II. Visual field defects. Arch Ophthalmol 1979;97:71-5. [Crossref] [PubMed]
- Chang MY, Velez FG, Demer JL, et al. Accuracy of Diagnostic Imaging Modalities for Classifying Pediatric Eyes as Papilledema Versus Pseudopapilledema. Ophthalmology 2017;124:1839-48. [Crossref] [PubMed]
- Kurz-Levin MM, Landau K. A comparison of imaging techniques for diagnosing drusen of the optic nerve head. Arch Ophthalmol 1999;117:1045-9. [Crossref] [PubMed]
- Noel LP, Clarke WN, MacInnis BJ. Detection of drusen of the optic disc in children by B-scan ultrasonography. Can J Ophthalmol 1983;18:266-8. [PubMed]
- Gili P, Flores-Rodriguez P, Yanguela J, et al. Using autofluorescence to detect optic nerve head drusen in children. J AAPOS 2013;17:568-71. [Crossref] [PubMed]
- Pineles SL, Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. J Neuroophthalmol 2012;32:17-22. [Crossref] [PubMed]
- Ghose S, Nayak BK. Role of oral fluorescein in the diagnosis of early papilloedema in children. Br J Ophthalmol 1987;71:910-5. [Crossref] [PubMed]
- Malmqvist L, Bursztyn L, Costello F, et al. The Optic Disc Drusen Studies Consortium Recommendations for Diagnosis of Optic Disc Drusen Using Optical Coherence Tomography. J Neuroophthalmol 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Merchant KY, Su D, Park SC, et al. Enhanced depth imaging optical coherence tomography of optic nerve head drusen. Ophthalmology 2013;120:1409-14. [Crossref] [PubMed]
- Borruat FX, Sanders MD. Vascular anomalies and complications of optic nerve drusen. Klin Monbl Augenheilkd 1996;208:294-6. [Crossref] [PubMed]
- Lee KM, Hwang JM, Woo SJ. Hemorrhagic complications of optic nerve head drusen on spectral domain optical coherence tomography. Retina 2014;34:1142-8. [Crossref] [PubMed]
- Sanders TE, Gay AJ, Newman M. Drusen of the optic disk-hemorrhagic complications. Trans Am Ophthalmol Soc 1970;68:186-218. [PubMed]
- Mustonen E. Optic disc drusen and tumours of the chiasmal region. Acta Ophthalmol (Copenh) 1977;55:191-200. [Crossref] [PubMed]
- Nanji AA, Klein KS, Pelak VS, et al. Nonarteritic anterior ischemic optic neuropathy in a child with optic disk drusen. J AAPOS 2012;16:207-9. [Crossref] [PubMed]
- Lee YA, Tomsak RL, Sadikovic Z, et al. Use of Ocular Coherence Tomography in Children With Idiopathic Intracranial Hypertension-A Single-Center Experience. Pediatr Neurol 2016;58:101-6.e1. [Crossref] [PubMed]
- Thompson AC, Bhatti MT, El-Dairi MA. Bruch's membrane opening on optical coherence tomography in pediatric papilledema and pseudopapilledema. J AAPOS 2018;22:38-43.e3. [Crossref] [PubMed]
- Banwell B, Kennedy J, Sadovnick D, et al. Incidence of acquired demyelination of the CNS in Canadian children. Neurology 2009;72:232-9. [Crossref] [PubMed]
- Absoud M, Cummins C, Desai N, et al. Childhood optic neuritis clinical features and outcome. Arch Dis Child 2011;96:860-2. [Crossref] [PubMed]
- Chang MY, Pineles SL. Pediatric Optic Neuritis. Semin Pediatr Neurol 2017;24:122-8. [Crossref] [PubMed]
- Waldman AT, Stull LB, Galetta SL, et al. Pediatric optic neuritis and risk of multiple sclerosis: meta-analysis of observational studies. J AAPOS 2011;15:441-6. [Crossref] [PubMed]
- Lana-Peixoto MA, Andrade GC. The clinical profile of childhood optic neuritis. Arq Neuropsiquiatr 2001;59:311-7. [Crossref] [PubMed]
- Lucchinetti CF, Kiers L, O'Duffy A, et al. Risk factors for developing multiple sclerosis after childhood optic neuritis. Neurology 1997;49:1413-8. [Crossref] [PubMed]
- Wan MJ, Adebona O, Benson LA, et al. Visual outcomes in pediatric optic neuritis. Am J Ophthalmol 2014;158:503-7.e2. [Crossref] [PubMed]
- Wilejto M, Shroff M, Buncic JR, et al. The clinical features, MRI findings, and outcome of optic neuritis in children. Neurology 2006;67:258-62. [Crossref] [PubMed]
- Kennedy C, Carroll FD. Optic neuritis in children. Trans Am Acad Ophthalmol Otolaryngol 1960;64:700-12. [PubMed]
- Bonhomme GR, Waldman AT, Balcer LJ, et al. Pediatric optic neuritis: brain MRI abnormalities and risk of multiple sclerosis. Neurology 2009;72:881-5. [Crossref] [PubMed]
- Borchert M, Liu GT, Pineles S, et al. Pediatric Optic Neuritis: What Is New. J Neuroophthalmol 2017;37:S14-S22. [Crossref] [PubMed]
- Yeh EA, Graves JS, Benson LA, et al. Pediatric optic neuritis. Neurology 2016;87:S53-8. [Crossref] [PubMed]
- Malik MT, Healy BC, Benson LA, et al. Factors associated with recovery from acute optic neuritis in patients with multiple sclerosis. Neurology 2014;82:2173-9. [Crossref] [PubMed]
- Yeh EA, Weinstock-Guttman B, Lincoff N, et al. Retinal nerve fiber thickness in inflammatory demyelinating diseases of childhood onset. Mult Scler 2009;15:802-10. [Crossref] [PubMed]
- Morales DS, Siakowski RM, Howard CW, et al. Optic neuritis in children. J Ophthalmic Nurs Technol 2000;19:270-4; quiz 5-6. [PubMed]
- . Visual function 5 years after optic neuritis: experience of the Optic Neuritis Treatment Trial. The Optic Neuritis Study Group. Arch Ophthalmol 1997;115:1545-52. [Crossref] [PubMed]
- Avery RA, Shah SS, Licht DJ, et al. Reference range for cerebrospinal fluid opening pressure in children. N Engl J Med 2010;363:891-3. [Crossref] [PubMed]
- Narula S, Liu GT, Avery RA, et al. Elevated cerebrospinal fluid opening pressure in a pediatric demyelinating disease cohort. Pediatr Neurol 2015;52:446-9. [Crossref] [PubMed]
- Rappoport D, Goldenberg-Cohen N, Luckman J, et al. Parainfectious optic neuritis: manifestations in children vs adults. J Neuroophthalmol 2014;34:122-9. [Crossref] [PubMed]
- Brenton JN, Banwell BL. Therapeutic Approach to the Management of Pediatric Demyelinating Disease: Multiple Sclerosis and Acute Disseminated Encephalomyelitis. Neurotherapeutics 2016;13:84-95. [Crossref] [PubMed]
- Young NP, Weinshenker BG, Lucchinetti CF. Acute disseminated encephalomyelitis: current understanding and controversies. Semin Neurol 2008;28:84-94. [Crossref] [PubMed]
- Dale RC, Brilot F, Banwell B. Pediatric central nervous system inflammatory demyelination: acute disseminated encephalomyelitis, clinically isolated syndromes, neuromyelitis optica, and multiple sclerosis. Curr Opin Neurol 2009;22:233-40. [Crossref] [PubMed]
- Heussinger N, Kontopantelis E, Gburek-Augustat J, et al. Oligoclonal bands predict multiple sclerosis in children with optic neuritis. Ann Neurol 2015;77:1076-82. [Crossref] [PubMed]
- Wingerchuk DM, Banwell B, Bennett JL, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 2015;85:177-89. [Crossref] [PubMed]
- Collongues N, Marignier R, Zephir H, et al. Long-term follow-up of neuromyelitis optica with a pediatric onset. Neurology 2010;75:1084-8. [Crossref] [PubMed]
- Waldman AT, Gorman MP, Rensel MR, et al. Management of pediatric central nervous system demyelinating disorders: consensus of United States neurologists. J Child Neurol 2011;26:675-82. [Crossref] [PubMed]
- Jayakody H, Bonthius DJ, Longmuir R, et al. Pediatric optic neuritis: does a prolonged course of steroids reduce relapses? A preliminary study. Pediatr Neurol 2014;51:721-5. [Crossref] [PubMed]
- Avery RA, Rajjoub RD, Trimboli-Heidler C, et al. Applications of optical coherence tomography in pediatric clinical neuroscience. Neuropediatrics 2015;46:88-97. [Crossref] [PubMed]
- Graves JS, Chohan H, Cedars B, et al. Sex differences and subclinical retinal injury in pediatric-onset MS. Mult Scler 2017;23:447-55. [Crossref] [PubMed]
- Yeh EA, Marrie RA, Reginald YA, et al. Functional-structural correlations in the afferent visual pathway in pediatric demyelination. Neurology 2014;83:2147-52. [Crossref] [PubMed]
- Ramanathan S, Dale RC, Brilot F. Anti-MOG antibody: The history, clinical phenotype, and pathogenicity of a serum biomarker for demyelination. Autoimmun Rev 2016;15:307-24. [Crossref] [PubMed]
- Hino-Fukuyo N, Haginoya K, Nakashima I, et al. Clinical features and long-term outcome of a group of Japanese children with inflammatory central nervous system disorders and seropositivity to myelin-oligodendrocyte glycoprotein antibodies. Brain Dev 2015;37:849-52. [Crossref] [PubMed]
- Thulasirajah S, Pohl D, Davila-Acosta J, et al. Myelin Oligodendrocyte Glycoprotein-Associated Pediatric Central Nervous System Demyelination: Clinical Course, Neuroimaging Findings, and Response to Therapy. Neuropediatrics 2016;47:245-52. [Crossref] [PubMed]
- Miller NR. Optic pathway gliomas are tumors! Ophthal Plast Reconstr Surg 2008;24:433. [Crossref] [PubMed]
- Liu GT, Katowitz JA, Rorke-Adams LB, et al. Optic pathway gliomas: neoplasms, not hamartomas. JAMA Ophthalmol 2013;131:646-50. [Crossref] [PubMed]
- Yeung SN, White VA, Nimmo M, et al. Optic nerve gliomas: role of Ki-67 staining of tumour and margins in predicting long-term outcome. Br J Ophthalmol 2011;95:1077-81. [Crossref] [PubMed]
- Miller NR. Optic Gliomas: Past, Present, and Future. J Neuroophthalmol 2016;36:460-73. [Crossref] [PubMed]
- Rasool N, Odel JG, Kazim M. Optic pathway glioma of childhood. Curr Opin Ophthalmol 2017;28:289-95. [Crossref] [PubMed]
- Dua S, Sharma K, Juneja R, et al. Unusual presentation of unilateral intra-orbital optic nerve pilocytic astrocytoma of the juvenile type in a geriatric patient. J Clin Neurosci 2016;25:143-4. [Crossref] [PubMed]
- Jamshidi S, Korengold M, Kobrine AI. Computed tomography of an optic chiasm glioma in an elderly patient. Surg Neurol 1984;21:83-7. [Crossref] [PubMed]
- Rush JA, Younge BR, Campbell RJ, et al. Optic glioma. Long-term follow-up of 85 histopathologically verified cases. Ophthalmology 1982;89:1213-9. [Crossref] [PubMed]
- DiMario FJ Jr, Ramsby G. Magnetic resonance imaging lesion analysis in neurofibromatosis type 1. Arch Neurol 1998;55:500-5. [Crossref] [PubMed]
- Balcer LJ, Liu GT, Heller G, et al. Visual loss in children with neurofibromatosis type 1 and optic pathway gliomas: relation to tumor location by magnetic resonance imaging. Am J Ophthalmol 2001;131:442-5. [Crossref] [PubMed]
- Listernick R, Ferner RE, Liu GT, et al. Optic pathway gliomas in neurofibromatosis-1: controversies and recommendations. Ann Neurol 2007;61:189-98. [Crossref] [PubMed]
- Listernick R, Charrow J, Greenwald M, et al. Natural history of optic pathway tumors in children with neurofibromatosis type 1: a longitudinal study. J Pediatr 1994;125:63-6. [Crossref] [PubMed]
- Thiagalingam S, Flaherty M, Billson F, et al. Neurofibromatosis type 1 and optic pathway gliomas: follow-up of 54 patients. Ophthalmology 2004;111:568-77. [Crossref] [PubMed]
- Singhal S, Birch JM, Kerr B, et al. Neurofibromatosis type 1 and sporadic optic gliomas. Arch Dis Child 2002;87:65-70. [Crossref] [PubMed]
- Czyzyk E, Jozwiak S, Roszkowski M, et al. Optic pathway gliomas in children with and without neurofibromatosis 1. J Child Neurol 2003;18:471-8. [Crossref] [PubMed]
- Wan MJ, Ullrich NJ, Manley PE, et al. Long-term visual outcomes of optic pathway gliomas in pediatric patients without neurofibromatosis type 1. J Neurooncol 2016;129:173-8. [Crossref] [PubMed]
- Spicer GJ, Kazim M, Glass LR, et al. Accuracy of MRI in defining tumor-free margin in optic nerve glioma surgery. Ophthal Plast Reconstr Surg 2013;29:277-80. [Crossref] [PubMed]
- . Tumor spread in unilateral optic glioma. Study report No. 2. North American Study Group for Optic Glioma. Neurofibromatosis 1989;2:195-203. [PubMed]
- Opocher E, Kremer LC, Da Dalt L, et al. Prognostic factors for progression of childhood optic pathway glioma: a systematic review. Eur J Cancer 2006;42:1807-16. [Crossref] [PubMed]
- Diggs-Andrews KA, Brown JA, Gianino SM, et al. Sex Is a major determinant of neuronal dysfunction in neurofibromatosis type 1. Ann Neurol 2014;75:309-16. [Crossref] [PubMed]
- Fisher MJ, Loguidice M, Gutmann DH, et al. Visual outcomes in children with neurofibromatosis type 1-associated optic pathway glioma following chemotherapy: a multicenter retrospective analysis. Neuro Oncol 2012;14:790-7. [Crossref] [PubMed]
- Tow SL, Chandela S, Miller NR, et al. Long-term outcome in children with gliomas of the anterior visual pathway. Pediatr Neurol 2003;28:262-70. [Crossref] [PubMed]
- Prada CE, Hufnagel RB, Hummel TR, et al. The Use of Magnetic Resonance Imaging Screening for Optic Pathway Gliomas in Children with Neurofibromatosis Type 1. J Pediatr 2015;167:851-6 e1.
- Dodgshun AJ, Elder JE, Hansford JR, et al. Long-term visual outcome after chemotherapy for optic pathway glioma in children: Site and age are strongly predictive. Cancer 2015;121:4190-6. [Crossref] [PubMed]
- Parsa CF, Hoyt CS, Lesser RL, et al. Spontaneous regression of optic gliomas: thirteen cases documented by serial neuroimaging. Arch Ophthalmol 2001;119:516-29. [Crossref] [PubMed]
- de Blank PMK, Fisher MJ, Liu GT, et al. Optic Pathway Gliomas in Neurofibromatosis Type 1: An Update: Surveillance, Treatment Indications, and Biomarkers of Vision. J Neuroophthalmol 2017;37:S23-S32. [Crossref] [PubMed]
- Avery RA, Hwang EI, Jakacki RI, et al. Marked recovery of vision in children with optic pathway gliomas treated with bevacizumab. JAMA Ophthalmol 2014;132:111-4. [Crossref] [PubMed]
- North K, Cochineas C, Tang E, et al. Optic gliomas in neurofibromatosis type 1: role of visual evoked potentials. Pediatr Neurol 1994;10:117-23. [Crossref] [PubMed]
- Jabbari B, Maitland CG, Morris LM, et al. The value of visual evoked potential as a screening test in neurofibromatosis. Arch Neurol 1985;42:1072-4. [Crossref] [PubMed]
- Lund AM, Skovby F. Optic gliomas in children with neurofibromatosis type 1. Eur J Pediatr 1991;150:835-8. [Crossref] [PubMed]
- Avery RA, Liu GT, Fisher MJ, et al. Retinal nerve fiber layer thickness in children with optic pathway gliomas. Am J Ophthalmol 2011;151:542-9.e2. [Crossref] [PubMed]
- Avery RA, Cnaan A, Schuman JS, et al. Longitudinal Change of Circumpapillary Retinal Nerve Fiber Layer Thickness in Children With Optic Pathway Gliomas. Am J Ophthalmol 2015;160:944-52.e1. [Crossref] [PubMed]
- Chang L, El-Dairi MA, Frempong TA, et al. Optical coherence tomography in the evaluation of neurofibromatosis type-1 subjects with optic pathway gliomas. J AAPOS 2010;14:511-7. [Crossref] [PubMed]
- Gu S, Glaug N, Cnaan A, et al. Ganglion cell layer-inner plexiform layer thickness and vision loss in young children with optic pathway gliomas. Invest Ophthalmol Vis Sci 2014;55:1402-8. [Crossref] [PubMed]
- Avery RA, Cnaan A, Schuman JS, et al. Reproducibility of circumpapillary retinal nerve fiber layer measurements using handheld optical coherence tomography in sedated children. Am J Ophthalmol 2014;158:780-7.e1. [Crossref] [PubMed]
- Lober RM, Guzman R, Cheshier SH, et al. Application of diffusion tensor tractography in pediatric optic pathway glioma. J Neurosurg Pediatr 2012;10:273-80. [Crossref] [PubMed]
- de Blank PM, Berman JI, Liu GT, et al. Fractional anisotropy of the optic radiations is associated with visual acuity loss in optic pathway gliomas of neurofibromatosis type 1. Neuro Oncol 2013;15:1088-95. [Crossref] [PubMed]
- Avery RA, Mansoor A, Idrees R, et al. Optic pathway glioma volume predicts retinal axon degeneration in neurofibromatosis type 1. Neurology 2016;87:2403-7. [Crossref] [PubMed]
- Bornhorst M, Frappaz D, Packer RJ. Pilocytic astrocytomas. Handb Clin Neurol 2016;134:329-44. [Crossref] [PubMed]
Cite this article as: Pineles SL. Pediatric neuro-ophthalmology: not simply neuro-ophthalmology for small adults. Ann Eye Sci 2018;3:15.