
Orthokeratology for myopia control: an optometrist’s view
Orthokeratology (OK, ortho-K) is a clinical technique that utilises specially designed rigid contact lenses, called reverse geometry lenses, to reshape the cornea for refractive correction. The lenses are worn overnight only and removed on awakening. The cornea is subtly flattened during overnight OK lens wear, and this is finely tuned by the eye care practitioner to provide sufficient reduction in corneal power after lens removal to correct the patient’s myopic refractive error (1). The technique provides only temporary refractive correction, as the cornea slowly regains its original shape while the lens is not being worn. Even after fairly long periods of OK treatment, the corneal topography and refraction return completely to pre lens wear levels after 2–4 weeks of lens wear abstention (2-4). In modern OK practice, lenses are usually fitted to correct low to moderate degrees of myopic refractive error.
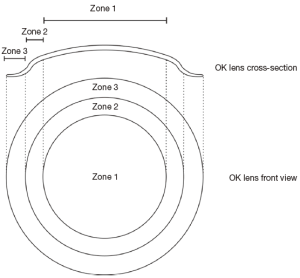
There are currently many OK lens designs on the market for correction of myopic refractive error, all broadly based on the reverse geometry design principle (Figure 1). The fundamental reverse geometry lens design incorporates three distinct zones. The central zone or base curve of the lens is fitted flatter than the central corneal curvature, and may comprise a spherical or aspheric curve or curves. The central zone serves to flatten the central cornea, reducing its power to correct myopia. Surrounding the central zone, a reverse curve zone comprising one or more curves steeper than the base curve gives this particular lens design its name. Spherical, aspheric or sigmoid curves have been used in this reverse curve zone, which acts to maintain lens centration and may also supplement the forces flattening the central cornea through negative pressure in the post-lens tear film. Finally, peripheral to the reverse curve zone is a zone of alignment to the underlying midperipheral cornea. The alignment curve zone bears the weight of the lens and aids in lens centration. Tangent or aspheric peripheral curves are often used for the alignment zone, which is surrounded by an edge lift to facilitate tear circulation. Different OK lens designs incorporate different numbers or types of curves in these three zones, and these curves can be modified to refine the lens fit and the sagittal height of the lens to control the degree of central corneal flattening and thus the myopia correction imparted by the lens through reshaping of the cornea (5).
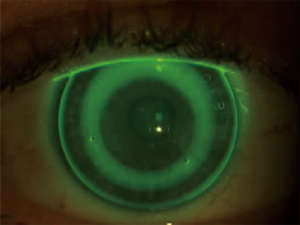
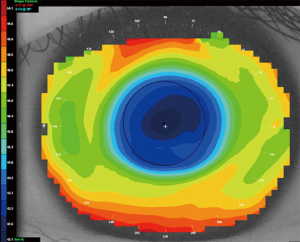
On the eye, a reverse geometry lens demonstrates an unusual and unique fluorescein pattern, revealing the characteristic back surface design features of this lens type (Figure 2). After overnight wear of a reverse geometry lens, corneal topographic change demonstrates a zone of central corneal flattening, surrounded by an annulus of relative corneal steepening in the midperiphery (Figure 3). Analysis of the corneal topographic changes induced after overnight lens wear allows the practitioner to refine lens parameters if necessary to optimise the fit of the lens and the refractive changes resulting from overnight corneal reshaping.
The original clinical application of OK lenses was for myopia correction, allowing clear device-free vision through the day for myopes, and thus providing an alternative to refractive correction with spectacles, contact lenses, or refractive surgery. More recently, OK lenses have been used increasingly for myopia control, to reduce or eliminate the progression of myopia in children developing myopic refractive error. This latter application of OK lenses now predominates in countries with a high prevalence of childhood myopia, in particular in East Asia.
OK for myopia correction
It is now well established that OK lenses effectively correct myopic refractive error during overnight wear (1,6). The greatest reduction in myopia, approximately 75%, occurs after the first night of overnight OK, and full correction of myopia can usually be achieved after 7–10 nights of overnight OK. There is slight regression of effect during the day while the lens is not worn. This is most pronounced on the first day after commencing OK treatment, but lessens with time and is rarely greater than 0.25–0.50 D. This is usually managed clinically by targeting a slight over-correction of myopia so that clear vision is maintained through waking hours despite this slight regression.
OK lens wear can reliably target correction of up to 4.00 D of myopia, but becomes less reliable for correcting higher myopia. In Asian countries where higher degrees of myopia are relatively common, practitioners routinely target up to 6.00 D of myopic correction, and may provide over-spectacles or daytime contact lenses to correct any residual myopia not corrected through corneal reshaping.
The corneal reshaping process has another minor advantage in that the cornea is mildly sphericalised by overnight wear of the OK lens, which normally has a spherical base curve. This may reduce corneal toricity slightly once the lens has been removed, providing a partial correction for low degrees of astigmatism (7). However, as OK technology has progressed, more complex corneal reshaping lens designs have been developed specifically to reshape the cornea for targeted correction of higher degrees of astigmatism, utilising toric back surface curves (8). Furthermore, OK lens designs are now available to steepen rather than flatten the central cornea, thus providing refractive correction for hyperopia and presbyopia (9,10). These more complex lens designs require advanced lens fitting skills and the ability to interpret and manipulate corneal topography to achieve the desired refractive effect through corneal reshaping.
Safety of overnight OK
Many studies, using a wide range of sophisticated technologies, have demonstrated that the corneal refractive reshaping in OK is achieved primarily through thinning of the central epithelium (11-15). There is no evidence to indicate that the corneal stroma undergoes any sustained bending during this procedure. This is reassuring as it implies little impact on the corneal endothelium. Indeed, no evidence suggests any significant endothelial morphological changes during OK lens wear beyond the normal contact lens-related effects one would expect to see in a long-term conventional contact lens wearer (16,17).
The understanding that OK works by thinning the central epithelium raises some concerns because of the importance of this corneal layer as a barrier protecting against the invasion of pathogens. The question has been raised, and continues to be asked, whether OK lens wear in some way may compromise this most important epithelial barrier against infection.
The issue of microbial keratitis (MK) in overnight OK lens wear first came to attention in the early 2000’s, with a growing number of reports in the literature and at scientific conferences of serious cases of MK in OK lens wearers. In 2007, Watt and Swarbrick published a retrospective analysis of 129 cases of MK in OK, analysing the demographics of the patients affected, clinical features of the infection, and trends over time since the first case report in 2001 (18,19).
Three important findings from this analysis helped us to understand the cause of this MK epidemic, and allowed measures to be put in place to reduce the risk of MK in OK.
- Firstly, of the 129 cases of MK in OK in this analysis, over 75% of the cases had occurred in East Asian countries, predominantly in China (38%) and Taiwan (28%). This pointed to a distinctly regional problem, indicating that measures to reduce risk needed to be targeted to these countries.
- The second major finding of the analysis was that of the 126 patients affected, most were children (8–15 years; 56%) or young adults (16–25 years; 39%). Clearly, the emotions stirred by this epidemic were exacerbated by the very young ages of affected patients, but also suggested that OK was being used predominantly in this age group for myopia control rather than simple refractive correction. It also raised concerns that children may be more susceptible than adults to infections during contact lens wear.
- The third important finding arose from an analysis of the microorganisms implicated as causative factors in the infections. Although 17% of cases were culture-negative or did not report on causative organisms, it came as no surprise that the most common organism implicated in these infections was Pseudomonas aeruginosa (38%). But an unexpected finding was that Acanthamoeba infection had occurred in 33% of cases. This is a very high proportion given that in other forms of contact lens wear Acanthamoeba is a rare infection. This discovery led the authors to conclude that exposure of OK lenses to contaminated or tap water during care and wear may be an important modifiable risk factor in these infections. This has resulted in a strong recommendation that tap water must be strictly avoided in the care and storage of OK lenses, and indeed in all forms of contact lens wear.
Further analysis of trends over time in rates of MK in OK over the period of the analysis [2001–2007] revealed that over half of the reported cases of MK in OK (51%) occurred in 2001, and all of these cases were reported from East Asian countries. In retrospect we now understand that OK lenses were being sold for myopia control use in children in an unregulated market, with little attention to choice of appropriate lens materials and designs or accurate lens fitting, minimal patient education in appropriate lens wear and care, and limited emphasis on the need for aftercare and follow-up (20). Once the scale of the problem became apparent, there was a significant drop in the number of cases reported in subsequent years. This was largely due to the imposition of regulations in China, Taiwan and Hong Kong in particular, restricting the prescription of OK lenses and introducing strict training and licensing requirements for OK practitioners, which still apply today.
Since the publication of Watt and Swarbrick’s paper, there have been fewer reports of MK in OK in the literature. Although this could be interpreted as a reduction in the number of cases of MK in this modality, it also may reflect a reluctance by practitioners to report such cases. For those cases that are still reported, the features of MK in OK remain largely unchanged. Most cases arise in the East Asian region and involve children wearing OK lenses for myopia control. Causative organisms remain predominantly Pseudomonas aeruginosa and Acanthamoeba spp., and exposure to tap water continues to be a common identifiable risk factor in many cases. Unfortunately, outcomes from these infections are often poor, especially if Acanthamoeba infection is involved.
The question therefore remains about the safety of OK relative to other modalities of contact lens wear. This is a difficult question to answer because ultimately the number of OK wearers is small, and varies between countries and over time. Furthermore, little reliable data are available about the frequency of MK in OK, making it impossible to simply calculate the overall incidence of MK in OK. Prospective controlled studies may be necessary to answer this question but would be prohibitively expensive given the low overall frequency of MK in a contact lens wearing population.
In 2013, Bullimore and colleagues (21) published a retrospective study which attempted to determine the relative risk of MK in overnight OK based on reports from OK practitioners in the US over a 3-year period [2005–2007]. All reports of a painful red eye amongst OK wearers were scrutinised by an independent expert panel to decide if the case was in fact MK, based on well-established criteria. Data were gathered from almost 2,600 patient years of overnight OK lens wear, split fairly evenly between adult and child patients. A total of 8 cases of painful red eye with infiltrates were reported to the study team, of which 2 were determined by the expert panel to be cases of MK, both of which occurred in children. Thus the authors were able to calculate an overall estimated incidence of MK in OK of 7.7 per 10,000 patient-years of lens wear, but with very wide confidence intervals. This estimate compares closely with estimates for the incidence of MK in other forms of conventional contact lens wear published by Stapleton et al. (22). Her group quoted estimates of 1.2 per 10,000 patient-years for rigid daily wear, 11.9 per 10,000 patient years for silicone hydrogel daily wear, and 19.5 per 10,000 patient years for hydrogel extended wear.
The findings from Bullimore’s group provided some confidence amongst OK practitioners that OK did not in itself present an inappropriate risk for patients prescribed this modality, provided that good practice was followed in fitting and managing these patients, and good compliance was maintained by the OK lens wearers. Nevertheless, MK remains a risk during overnight OK and vigilance is necessary to ensure that this modality is used wisely and safely by well-educated practitioners following accepted international standards for safe contact lens wear.
OK for myopia control
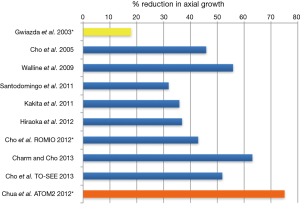
The growing clinical use of overnight OK over recent years has undoubtedly been stimulated by increasing anecdotal reports and clinical studies reporting the efficacy of this modality in slowing or eliminating axial eye growth in young progressive myopes (23-30). Although an increasing number of studies have been published in the scientific literature demonstrating this efficacy (Figure 4), it is important to point out that few of these studies have been randomised prospective clinical trials, and all studies but one (26) have been limited to 2 years duration. Nevertheless, the results from published studies have been consistently impressive, with a myopia control efficacy averaging approximately 45%, ranging from 32% to 63% efficacy. This clearly exceeds the efficacy of bifocal or progressive addition spectacle lens treatment as reported in the COMET studies (31,32), but does not reach the reported efficacy for 1% atropine reported in the ATOM study (33). Interestingly the efficacy of OK for myopia control is close to that of low dose (0.01%) atropine, an increasingly common treatment for myopia control in East Asian countries (34).
Recent meta-analyses of the efficacy of OK for myopia control (35,36), including comparisons with other interventions for myopia control (37), have confirmed the efficacy of this modality in inhibiting the axial elongation that underlies progression of myopia in children.
Although there is still some dispute about the exact mechanism whereby OK lenses achieve their myopia control effect, the most compelling hypothesis involves the concept of manipulating peripheral refraction (38). It is well established that myopes typically exhibit peripheral hyperopic defocus—that is, peripheral rays of light come to a focus behind the peripheral retina when spectacle lenses or conventional contact lenses are used to correct the central refractive error (Figure 5A). This effect arises primarily because the myopic eye takes on an elongated egg-like prolate shape as it grows. It has been hypothesised that this peripheral hyperopic defocus acts as a stimulus for continuing axial elongation even when the central image on the fovea is in focus.
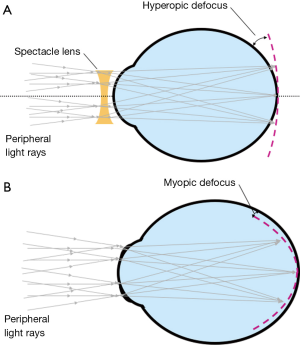
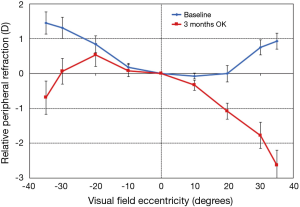
The corollary to this theory is that if these peripheral rays can instead be brought to a focus either on the peripheral retina or in front of the peripheral retina (peripheral myopic defocus), this may act as a brake on the continuing elongation of the eye (38). Such an optical manipulation occurs (by chance) with corneal reshaping in OK, which creates an annulus of positive power at the edge of the central flattened treatment zone. While the central OK treatment zone places central rays in focus on the fovea, correcting the central myopic refractive error, the peripheral plus-power annulus acts to refocus the peripheral rays in front of the retina to achieve peripheral myopic defocus (Figure 5B). The induction of relative peripheral myopic defocus by OK corneal reshaping (Figure 6) has been demonstrated in many studies (39,40), and it is this effect that is believed to underlie the myopia control effects of OK.
In 2015, the ROK (Research in OK) Group at the School of Optometry and Vision Science at UNSW Sydney published the results of a 1-year prospective randomised contralateral eye clinical trial comparing the myopia control effects of overnight OK and conventional rigid gas-permeable (GP) lens daily wear (41). Young East Asian progressive myopes were enrolled in the study to wear an OK lens in one eye overnight and a GP lens in the other eye during the day for a 6-month period. Then the lens-eye combinations were reversed for another 6 months. Axial length was monitored in both eyes over the 12-month study.
The results demonstrated significant inhibition in axial eye growth in the OK lens-wearing eye in both phases of the study, whereas the eye wearing the GP lens showed significant axial growth and myopia progression (Figure 7). The cross-over in effect after 6 months was particularly striking, and confirmed the different impacts of these two modalities on myopia progression. But an important outcome of this study was the large individual variation in the effects of both lens types on axial growth. In particular in the OK lens-wearing eye, some subjects showed complete inhibition of eye growth, whereas other subjects showed similar eye growth and myopia progression as in the GP lens-wearing eye.
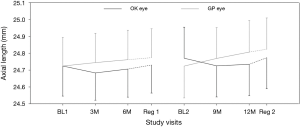
This variability in response to OK lenses for myopia control now stands as a major challenge for the future application of this modality to manage myopic eye growth. At this stage of our knowledge we cannot identify which children are likely to benefit from OK lens wear for control of their myopic progression, and which children might be more suited to alternative approaches such as low dose atropine or soft multifocal contact lenses (42), both of which have demonstrated efficacy in myopia control.
This finding also emphasises the need for caution in interpreting efficacy figures, which are frequently used to compare different myopia control treatments. When a treatment modality is quoted as having a “45%” efficacy, this does not mean that all children in this modality will show a 45% reduction in eye growth. This figure is an averaged efficacy; some children may show a much greater treatment effect whereas others may show no treatment effect. Unfortunately we currently are not able to predict whether an individual child will gain treatment benefits from OK (or any other myopia control modality). This understanding is an important aspect of counselling parents in relation to myopia control for their particular child.
The challenges for the future of OK in myopia control therefore revolve around the quest for strategies to identify which children will benefit from this treatment modality. Are some OK lens designs better than others in terms of myopia control efficacy (5)? Is it possible for us to customise OK lens designs, and thus the corneal reshaping outcomes, to target improved efficacy for individual children (43)? And is there a role for combination or sequential therapies utilising OK, low dose atropine and soft multifocal lens modalities to optimise the effects on myopia progression of these different modalities?
In summary, overnight OK provides a temporary correction for low to moderate myopic refractive error through corneal reshaping. Because lenses are only worn at night, the successful OK patient is able to benefit from device-free clear vision during waking hours. The safety of this modality compares favourably with other conventional modalities of contact lens wear, as long as the lenses are fitted appropriately by suitably educated practitioners, and that patients are compliant with safe lens wear and care practices.
Overnight OK is also effective in slowing eye growth in young progressive myopes, with an average myopia control efficacy of approximately 45% over 2 years. Questions relating to accrual of effect over longer treatment periods, and the potential for rebound of effect on discontinuing OK lens wear are beyond the scope of this paper and require further research. A major challenge for this modality is to determine ways in which treatment efficacy can be optimised for individual children, and to investigate the role of combination and sequential therapies in the management of myopic progression in children.
Acknowledgments
The author acknowledges the considerable contributions of her colleagues Dr. Pauline Kang, Dr. Vinod Maseedupally, Dr. Edward Lum, Ms Kathleen Watt, Dr. Ahmed Alharbi and Dr. Paul Gifford to the work reviewed in this paper. Research conducted by the author that is reviewed in this paper was supported under the Australian Research Council Linkage Project scheme, with industry collaborators Bausch + Lomb, Capricornia Contact Lens, and BE Enterprises.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ian G. Morgan, Xiaohu Ding and Xinxing Guo) for the series “Managing Myopia in East Asia Myopia Crisis” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.02.01). The series “Managing Myopia in East Asia Myopia Crisis” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Swarbrick HA. Invited Review: orthokeratology review and update. Clin Exp Optom 2006;89:124-43. [Crossref] [PubMed]
- Soni PS, Nguyen TT, Bonanno JA. Overnight orthokeratology: refractive and corneal recovery after discontinuation of reverse-geometry lenses. Eye Contact Lens 2004;30:254-62. [Crossref] [PubMed]
- Barr JT, Rah MJ, Meyers W, et al. Recovery of refractive error after Corneal Refractive Therapy. Eye Contact Lens 2004;30:247-51. [Crossref] [PubMed]
- Kobayashi Y, Yanai R, Chikamoto N, et al. Reversibility of effects of orthokeratology on visual acuity, refractive error, corneal topography, and contrast sensitivity. Eye Contact Lens 2008;34:224-8. [Crossref] [PubMed]
- Kang P, Swarbrick HA. The influence of different OK lens designs on peripheral refraction. Optom Vis Sci 2016;93:1112-9. [Crossref] [PubMed]
- Alharbi A, Swarbrick HA. The effects of overnight orthokeratology lens wear on corneal thickness. Invest Ophthalmol Vis Sci 2003;44:2518-23. [Crossref] [PubMed]
- Mountford J, Pesudovs K. An analysis of the astigmatic changes induced by accelerated orthokeratology. Clin Exp Optom 2002;85:284-93. [Crossref] [PubMed]
- Chen CC, Cheung SW, Cho P. Toric orthokeratology for highly astigmatic children. Optom Vis Sci 2012;89:849-55. [Crossref] [PubMed]
- Gifford P, Swarbrick HA. Time course of corneal changes in overnight hyperopic orthokeratology. Optom Vis Sci 2008;85:1165-71. [Crossref] [PubMed]
- Gifford P, Swarbrick HA. Refractive changes from hyperopic orthokeratology monovision in presbyopes. Optom Vis Sci 2013;90:306-13. [Crossref] [PubMed]
- Swarbrick HA, Wong G, O’Leary DJ. Corneal response to orthokeratology. Optom Vis Sci 1998;75:791-9. [Crossref] [PubMed]
- Choo JD, Caroline PJ, Harlin DD, et al. Morphologic changes in cat epithelium following continuous wear of orthokeratology lenses: a pilot study. Cont Lens Anterior Eye 2008;31:29-37. [Crossref] [PubMed]
- Reinstein DZ, Gobbe M, Archer TJ, et al. Epithelial, stromal, and corneal pachymetry changes during orthokeratology. Optom Vis Sci 2009;86:E1006-14. [Crossref] [PubMed]
- Nieto-Bona A, Gonzalez-Mesa A, Nieto-Bona MP, et al. Long-term changes in corneal morphology induced by overnight orthokeratology. Curr Eye Res 2011;36:895-904. [Crossref] [PubMed]
- Lian Y, Shen M, Jiang J, et al. Vertical and horizontal thickness profiles of the corneal epithelium and Bowman’s layer after orthokeratology. Invest Ophthalmol Vis Sci 2013;54:691-6. [Crossref] [PubMed]
- Hiraoka T, Furuya A, Matsumoto Y, et al. Influence of overnight orthokeratology on corneal endothelium. Cornea 2004;23:S82-6. [Crossref] [PubMed]
- Liu YM, Xie P. The safety of orthokeratology – a systematic review. Eye Contact Lens 2016;42:35-42. [Crossref] [PubMed]
- Watt K, Swarbrick HA. Microbial keratitis in overnight orthokeratology. Eye Contact Lens 2005;31:201-8. [Crossref] [PubMed]
- Watt KG, Swarbrick HA. Trends in microbial keratitis associated with orthokeratology. Eye Contact Lens 2007;33:373-7. [Crossref] [PubMed]
- DeWoolfson BH. Orthokeratology lens-related ulcers in children – letter to the editor. Ophthalmology 2005;112:167. [Crossref] [PubMed]
- Bullimore MA, Sinnott LT, Jones-Jordan LA. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci 2013;90:937-44. [Crossref] [PubMed]
- Stapleton F, Keay L, Edwards K, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology 2008;115:1655-62. [Crossref] [PubMed]
- Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res 2005;30:71-80. [Crossref] [PubMed]
- Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol 2009;93:1181-5. [Crossref] [PubMed]
- Kakita T, Hiraoka T, Oshika T. Influence of overnight orthokeratology on axial alongation in childhood myopia. Invest Ophthalmol Vis Sci 2011;52:2170-4. [Crossref] [PubMed]
- Hiraoka T, Kakita T, Okamoto F, et al. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci 2012;53:3913-9. [Crossref] [PubMed]
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Myopia control with orthokeratology contact lenses in Spain (MCOS): refractive and biometric changes. Invest Ophthalmol Vis Sci 2012;53:5060-5. [Crossref] [PubMed]
- Cho P, Chung SW. Retardation of myopia in orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci 2012;53:7077-85. [Crossref] [PubMed]
- Charm J, Cho P. high myopia-partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci 2013;90:530-9. [Crossref] [PubMed]
- Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE study). Invest Ophthalmol Vis Sci 2013;54:6510-7. [Crossref] [PubMed]
- Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci 2003;44:1492-500. [Crossref] [PubMed]
- . Correction of Myopia Evaluation Trial (COMET) 2 Study Group for the Pediatric Eye Disease Investigator Group. Progressive-addition lenses versus single-vision lenses for slowing progression of myopia in children with high accommodative lag and near esophoria. Invest Ophthalmol Vis Sci 2011;52:2749-57. [Crossref] [PubMed]
- Chua WH, Balakrishnan V, Chan YH, et al. Atropine for the treatment of childhood myopia. Ophthalmology 2006;113:2285-91. [Crossref] [PubMed]
- Chia A, Chua WH, Cheung YB, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology 2012;119:347-54. [Crossref] [PubMed]
- Si JK, Tang K, Bi HS, et al. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci 2015;92:252-7. [Crossref] [PubMed]
- Wen D, Huang J, Chen H, et al. Efficacy and acceptability of orthokeratology for slowing myopic progression in children: a systematic review and meta-analysis. J Ophthalmol 2015;2015:360806.
- Huang J, Wen D, Wang Q, et al. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology 2016;123:697-708. [Crossref] [PubMed]
- Smith EL 3rd. Prentice Award Lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci 2011;88:1029-44. [Crossref] [PubMed]
- Kang P, Swarbrick H. Peripheral refraction in myopic children wearing OK and GP lenses. Optom Vis Sci 2011;88:476-82. [Crossref] [PubMed]
- Queirós A, Gonzalez-Meijome JM, Jorge J, et al. Peripheral refraction in myopic patients after orthokeratology. Optom Vis Sci 2010;87:323-9. [PubMed]
- Swarbrick HA, Alharbi A, Watt K, et al. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology 2015;122:620-30. [Crossref] [PubMed]
- Walline JJ, Greiner KL, McVey ME, et al. Multifocal contact lens myopia control. Optom Vis Sci 2013;90:1207-14. [Crossref] [PubMed]
- Kang P, Gifford P, Swarbrick H. Can manipulation of OK lens parameters modify peripheral refraction? Optom Vis Sci 2013;90:1237-48. [Crossref] [PubMed]
Cite this article as: Swarbrick HA. Orthokeratology for myopia control: an optometrist’s view. Ann Eye Sci 2018;3:17.


