
Use of a handheld slit beam intraoperatively to assist in big bubble formation during deep anterior lamellar keratoplasty
Introduction
Deep anterior lamellar keratoplasty (DALK) is increasingly seen as a preferred surgical alternative to traditional penetrating keratoplasty (PKP) in patients with isolated corneal stromal scarring or ectasia with normal Descemet’s membrane (DM) and endothelium (1-3). In comparison to PKP, DALK preserves the patient’s own endothelium, thereby essentially eliminating the risk of endothelial immune rejection (4). However, optimal visual acuity is only achieved in DALK when DM is completely bared or only minimal host residual posterior stroma remains (5). In order to bare DM or achieve a clean excision of the majority of the host corneal stroma, multiple techniques have been proposed (1,6). To date, the most popular method for achieving this dissection is the big-bubble technique first described by Anwar et al. in 2002 (7).
The big-bubble technique involves injection of air into the deep posterior stroma of the cornea in order to create a pneumatic dissection plane between pre-Descemet’s layer (type 1 bubble) or DM (type 2 bubble) and the posterior stroma (8). Though effective, this technique is challenging with a steep learning curve (4,9). An adequate injection depth just above DM is required in order to achieve a consistent big-bubble (10). However, under the en face illumination of a surgical scope, the depth of a needle within the thin cornea stroma can often be difficult to assess. Overly aggressive needle placement can result in perforation of DM, which may necessitate conversion to PKP.
Intraoperative ocular coherence tomography (OCT) and femtosecond laser technology have been touted as solutions to this problem, by providing intraoperative confirmation of the depth of needle placement or by providing a pre-cut needle track to the appropriate depth, respectively (10-12). However, the technology is, as of yet, still unrefined. Currently, intraoperative OCT units lack true microscope integrated, real-time surgical scanning capabilities. And femtosecond lasers still lack standardized built-in software protocols for DALK needle-tracks (10-12). Furthermore, the technology remains expensive and most surgeon have limited access to these options.
To that end, we describe here a novel technique for reliably achieving a big-bubble in DALK by using a relatively inexpensive Eidolon model 510L handheld slit lamp (Eidolon Optical LLC, Natick, MA, USA) to guide needle placement.
Operative techniques
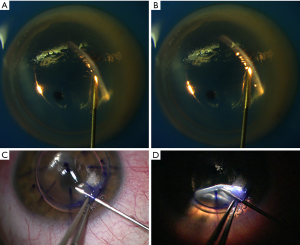
The host cornea is first trephinated to approximately 80% depth. Following trephination, a single paracentesis incision is created. Aqueous is burped from the AC and replacement with a single large air bubble. The use of an air fluid interface to improve visualization of DM was first described by Melles et al. and offers improved visualization even under en face illumination, but is even more effective with slit beam illumination (13). The presence of an air-fluid interface at DM creates bright specular reflection under appropriately positioned slit beam illumination (Figure 1). Care is taken during this step to maintain a low to normal intraocular pressure to ensured lower inflation pressures during big-bubble formation.
Next, using 0.12 forceps for stabilization, a bent 27-gauge needle on a 5 mL syringe is placed into the corneal stroma at the level of the trephination and advanced partially into the host corneal stroma. Alternatively, Fogla or other DALK instruments can be used to begin this initial stromal tunnel. The handheld slit beam is secured into the finger of a sterile surgical glove with a single small area cut at the tip of the finger to allow unimpeded illumination from the device. The slit beam is then positioned over the surgical field by an assistant, with the beam in focus on the cornea (working distance of approximately one inch) and set at its thinnest setting. The slit beam is then oriented 45 degrees to the tip of the needle with the slit beam at the tip or immediately in front of the needle tip to assist with guidance of the needle during advancement to the paracentral deep stroma. Care should be taken to illuminate the cornea obliquely from the periphery to maximize specular reflection. With dimming of the en face illumination of the surgical scope, the slit beam and depth of the needle tip within the cornea stroma is easily appreciated. Gentle sweeps of the slit beam across the needle tip at this point can further highlight the depth of the needle (Figures S1,S2).
DM should also be clearly visible at this point due to the bright reflection off of the air-DM interface. This bright reflection off DM allows clear visualization of a wave like distortion in DM when appropriate depth is achieved (Figure 1). This frequently correlates with a decreased resistance to needle advancement, which has previously been described (14). Once appropriate depth is achieved, air can be injected forcefully until creation of a type 1 big bubble is demonstrated. Alternatively, the needle can be retracted and a DALK cannula can be inserted into the needle track to complete the pneumo-dissection.
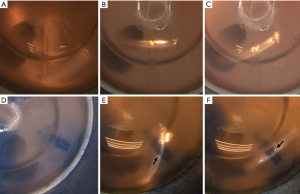
If depth of the needle or cannula is difficult to appreciate, a small amount of air or trypan blue can be injected to slightly pneumatize or stain the needle track, respectively (Figure 2). This further enhances the visualization of stromal depth under slit beam illumination.
Following completion of the big bubble and separation of posterior stroma from underlying Pre-Descemet’s membrane, removal of the overlying stroma can be performed as previously described by Anwar and Teichmann (7).
Comments
We describe here a novel technique for using a handheld slit lamp to assist in big bubble formation and demonstrate its use both in the lab with cadaveric donor corneas on a false anterior chamber (Figure S1), as well intraoperatively in a patient with keratoconus (Figure S2). Intraoperative use of a portable handheld slit lamp has previously been described in DM endothelial keratoplasty (DMEK) surgery as a reliable method for confirming DMEK graft orientation (15). It has further been described in DALK surgery a means of confirming big-bubble formation (15). However, to the best of our knowledge, use of a handheld slit lamp for real-time guidance of needle placement in order to consistently achieve a big-bubble during DALK surgery has never been described.
By using slit beam illumination, the surgeon is better able to assess his or her needle depth compared to the standard en face illumination of a surgical scope due to direct visualization of the full thickness of the cornea. Use of the slit beam also synergistically improves visualization of DM when combined with placement of a large intracameral air bubble, as described by Melles et al. (13). This, in turn, helps reduce the risk for DM perforation. This synergistic improvement in visualization of DM is achieved because specular reflection from the slit beam illumination off the air-DM interface highlights DM to a degree that is not achievable with standard en face illumination. Though we demonstrate use of the Eidolon slit lamp in DALK surgery using a 27-gauge needle, other DALK instruments or cannulas can just as easily be used with the handheld slit lamp.
DALK surgery remains a challenging procedure for corneal surgeons and creation of a big-bubble remains one of the most difficult steps. Success rates for big-bubble formation range from 65% to 85.3% even in the hands of experienced surgeons (3,16,17). Multiple studies have further acknowledged a steep learning curve with even lower success rates in the hands of inexperienced surgeons (4,9,16). Further studies to evaluate efficacy of this technique in the hands of experienced and inexperienced DALK surgeons will be important moving forward.
A handheld slit lamp has multiple advantages over microscope-mounted slit lamps, including being more flexible in terms of positioning and angling the light beam and being more cost-effective (15). Use of a handheld slit lamp is further advantageous over current intraoperative OCTs since it provides real-time visualization of needle insertion (10,11). Though future advancements in intraoperative OCT and femtosecond laser technology may ultimately lead to more widespread use of those technologies and even higher success rates with big-bubble DALK surgery, use of a handheld slit lamp technique will remain a cost-efficient, simple, and effective alternative.
One limitation to this technique is the need for an assistant to be present to position the slit lamp and intermittently sweep the beam across the needle tip. A possible modification to the technique that could address this issue is potentially using a fixed articulating stand to hold the slit beam in proper position for the unassisted surgeon. Alternatively, even without an assistant the handheld slit beam can still be used to confirm the depth of the needle after it has already been advanced.
In conclusion, the technique described here for use of a handheld slit lamp to assist in big-bubble formation in DALK surgery is an inexpensive and effective method for increasing the success rates for novice surgeons.
Acknowledgments
This study was supported by an unrestricted grant from the Minnesota Lions Vision Foundation.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Joann Kang, Viral Juthani and Roy S. Chuck) for the series “Refractive Surgery” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.10.01). The series “Refractive Surgery” was commissioned by the editorial office without any funding or sponsorship. JH Hou is consultant for AbbVie, Inc. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Anwar M, Teichmann KD. Deep lamellar keratoplasty: surgical techniques for anterior lamellar keratoplasty with and without baring of Descemet's membrane. Cornea 2002;21:374-83. [Crossref] [PubMed]
- Arslan OS, Ünal M, Tuncer I, et al. Deep anterior lamellar keratoplasty using big-bubble technique for treatment of corneal stromal scars. Cornea 2011;30:629-33. [Crossref] [PubMed]
- Fogla R. Deep anterior lamellar keratoplasty in the management of keratoconus. Indian J Ophthalmol 2013;61:465-8. [Crossref] [PubMed]
- Smadja D, Colin J, Krueger RR, et al. Outcomes of deep anterior lamellar keratoplasty for keratoconus: learning curve and advantages of the big bubble technique. Cornea 2012;31:859-63. [Crossref] [PubMed]
- Knutsson KA, Rama P, Paganoni G. Modified big-bubble technique compared to manual dissection deep anterior lamellar keratoplasty in the treatment of keratoconus. Acta Ophthalmol 2015;93:431-8. [Crossref] [PubMed]
- Parmar P, Salman A, Kalavathy CM, et al. Simplified technique for deep anterior lamellar keratoplasty. Cornea 2007;26:707-8. [Crossref] [PubMed]
- Anwar M, Teichmann KD. Big-bubble technique to bare Descemet's membrane in anterior lamellar keratoplasty. J Cataract Refract Surg 2002;28:398-403. [Crossref] [PubMed]
- Goweida MB. Intraoperative review of different bubble types formed during pneumodissection (big-bubble) deep anterior lamellar keratoplasty. Cornea 2015;34:621-4. [Crossref] [PubMed]
- Unal M, Bilgin B, Yucel I, et al. Conversion to deep anterior lamellar keratoplasty (DALK): learning curve with big-bubble technique. Ophthalmic Surg Lasers Imaging 2010;41:642-50. [Crossref] [PubMed]
- Scorcia V, Busin M, Lucisano A, et al. Anterior segment optical coherence tomography-guided big-bubble technique. Ophthalmology 2013;120:471-6. [Crossref] [PubMed]
- Au J, Goshe J, Dupps WJ Jr, et al. Intraoperative Optical Coherence Tomography for Enhanced Depth Visualization in Deep Anterior Lamellar Keratoplasty From the PIONEER Study. Cornea 2015;34:1039-43. [Crossref] [PubMed]
- Buzzonetti L, Petrocelli G, Valente P, et al. The Big-Bubble Full Femtosecond Laser-Assisted Technique in Deep Anterior Lamellar Keratoplasty. J Refract Surg 2015;31:830-4. [Crossref] [PubMed]
- Melles GR, Lander F, Rietveld FJ, et al. A new surgical technique for deep stromal, anterior lamellar keratoplasty. Br J Ophthalmol 1999;83:327-33. [Crossref] [PubMed]
- Sarnicola V, Toro P. Blunt cannula for descemetic deep anterior lamellar keratoplasty. Cornea 2011;30:895-8. [Crossref] [PubMed]
- Burkhart ZN, Feng MT, Price MO, Price FW. Handheld slit beam techniques to facilitate DMEK and DALK. Cornea 2013;32:722-4. [Crossref] [PubMed]
- Ghanem RC, Bogoni A, Ghanem VC. Pachymetry-guided intrastromal air injection ("pachy-bubble") for deep anterior lamellar keratoplasty: results of the first 110 cases. Cornea 2015;34:625-31. [Crossref] [PubMed]
- Muftuoglu O, Toro P, Hogan RN, et al. Sarnicola air-visco bubble technique in deep anterior lamellar keratoplasty. Cornea 2013;32:527-32. [Crossref] [PubMed]
- Davis AS, Bedard P, Hou JH. Demonstration showing use of a portable slit beam to visualize the depth of stromal needle placement in a donor cornea on a false anterior chamber. Asvide 2018;5:826. Available online: http://www.asvide.com/article/view/27991
- Davis AS, Bedard P, Hou JH. Intraoperative demonstration showing use of a portable slit beam to provide real-time guidance during needle placement in deep anterior lamellar keratoplasty surgery. Asvide 2018;5:827. Available online: http://www.asvide.com/article/view/27992
Cite this article as: Davis AS, Bedard P, Hou JH. Use of a handheld slit beam intraoperatively to assist in big bubble formation during deep anterior lamellar keratoplasty. Ann Eye Sci 2018;3:54.


