
胶原交联在儿童屈光矫正中的应用
引言
Wollensak等人于2003年首先提出应用角膜胶原交联(CXL)来治疗圆锥角膜[1]。同年晚些时候,Wollensak和他的团队描述了CXL对屈光的影响,屈光不正平均减少了 1.14 D[2]。从那时起,CXL治疗进展性圆锥角膜引起了广泛的关注,并于 2016 年,该方法被美国食品和药物管理局 (FDA) 批准用于治疗14岁以上人群。2011 年,CXL首次被报道用于治疗小儿进展性圆锥角膜,该报道中小儿患者的年龄范围为10至14岁[3]。另有报道,进展性圆锥角膜接受CXL治疗的最小患者年龄为4岁[4]。本文综述了对于小儿使用CXL治疗的文献,主要侧重于在屈光方面的作用、疗效和安全性。
CXL方案
CXL的作用机制是通过紫外线A (UVA)激活核黄素,增加角膜基质胶原束的强度。标准Dresden方案是Wollensak等人提出的首个CXL方案,并且是目前在美国获得FDA批准的唯一方案[2,5]。现已有多种其他CXL方案,包括快速CXL方案、跨上皮CXL方案和离子电渗疗法[6]。
标准Dresden方案
角膜上皮是核黄素能否完全渗透到角膜基质中的屏障。因此,在标准Dresden方案中,要求在局部麻醉下对角膜中央9mm范围的角膜上皮进行机械刮除。角膜刮除后,每2分钟滴1滴 0.1%核黄素溶液,持续30分钟;然后进行紫外线A光(370±5 nm波长,5.4 J/cm2辐照度)的持续照射,期间每2分钟滴1次核黄素溶液,持续30分钟[2]。迄今为止,标准Dresden方案仍然是成人和儿童人群中使用最广泛的CXL方案。
快速CXL方案
快速CXL方案最初源自本生-罗斯科光化学互易定律(Bunsen-Roscoe Law of Reciprocity of Photochemistry)。该定律认为,紫外线的光化学效应与传递的总能量成正比,并且与每个方案的总剂量有关,与相对强度和照射时间无关[7]。
Shetty等人于2014年首先发表了小儿快速CXL方案[8]。从那时起,快速CXL方案被其他几个团队应用和研究,从2014年到2018年共发表了8篇论文[9-15]。这些研究报告中的小儿患者采取的快速CXL方案有以下几种:UVA照射30 mW/cm2持续3分钟、10 mW/cm2持续9分钟,或9 mW/cm2持续10分钟。
跨上皮CXL方案
鉴于安全性的提高和术后不适的减少,跨上皮CXL已成为一种有吸引力的选择方案。改良的核黄素(Ricrolin TE,0.1%核黄素,SOOFT Italia SpA,Italy)被开发用于跨上皮传导,其添加了两种药物——氨丁三醇和乙二胺四乙酸钠,以增强对完整角膜上皮的渗透[6]。Buzzonetti等人、Salman等人、Eraslan等人分别于2012年、2016年、2017年[16-18]发表了3篇关于儿童跨上皮CXL方案的研究文章。跨上皮CXL方案和标准Dresden方案之间的唯一区别是角膜上皮的状态和核黄素溶液的构成。
Henriquez等人研究了快速跨上皮CXL方案对儿童进展性圆锥角膜的影响[19]。在这个特定的方案中,跨上皮核黄素溶液由0.25%核黄素、1.0%磷酸羟丙基甲基纤维素和0.007%苯扎氯铵组成。该溶液每5分钟给药一次,持续30分钟,然后用平衡盐溶液冲洗,然后进行18 mW/cm2的UVA照射5分钟。
离子电渗CXL方案
当于低强度电场使用离子电渗疗法时,其促进了分子穿透完整组织。Buzzonetti等人、Magli等人报道了离子电渗对儿童跨上皮CXL的辅助[20,21]。用于离子电渗CXL疗法的核黄素溶液由0.1%的核黄素组成,不含葡聚糖或氯化钠,并添加了两种增强剂——氨丁三醇和乙二胺四乙酸(Ricrolin+,SOOFT,Montegiorgio, Italy)。两项已发表的研究均采用相同的离子电渗系统(I-ON CXL;SOOFT Italia SpA,Italy),由一个电源、两个电极和一个连接电缆组成。在该方案中,离子电渗疗法进行5分钟,然后进行10 mW/cm2的UVA照射9分钟。
CXL对儿童的屈光作用
迄今为止, CXL仅被报道用于治疗小儿进展性圆锥角膜。圆锥角膜是一种发生于双眼角膜,通常不对称的非炎症性、进行性变性疾病[22]。角膜逐渐变薄导致生物力学减弱,表现为角膜变薄和突出。这种渐进的角膜变薄和突出导致不规则散光并引起中度至重度视力障碍。此外,角膜前弹力层和后弹力层均有可能破裂,从而导致各种各样的角膜瘢痕[6]。虽然圆锥角膜典型发病期是在青春期,但确实也会影响年幼的儿童。Léoni-Mesplié等人做了一项大型回顾性研究,评估了216名不同年龄组的圆锥角膜患者,发现儿童圆锥角膜在确诊时明显比成年人更严重,进展速度比成人更快[22]。鉴于小儿圆锥角膜的病情进展更加严重且具有侵袭性,迄今为止已经做了大量研究来评估CXL对阻止圆锥角膜进展及其随后对屈光状态的影响。
Padmanabhan等人发表了一篇关于CXL对儿童进展性圆锥角膜影响的文章,迄今为止是纳入研究眼睛数目最大的文献[23]。在这项研究中,336名进展性圆锥角膜小儿患者的377只眼接受了标准Dresden CXL方案,并在治疗后进行了2年至6.7年的随访。他们观察到,在CXL术后2年,采用Snellen视力表进行视力测试,最佳眼镜矫正远视力可完整的增加1行。
Mazzotta等人发表了一篇随访时间最长的文章,包括了小儿进展性圆锥角膜CXL术后10年的数据[24]。他们发现,在CXL术后10年,采用Snellen视力表,裸眼远用视力提高了0.21行,矫正远视力提高了0.03行。
对接受标准Dresden CXL治疗的进展性圆锥角膜儿童患者,随访时间从12个月到10年不等,有几项研究在后续不同的时间点分别报告了裸眼远用视力平均改善1到2行,矫正远用视力平均改善2到3行[23-37](表1)。
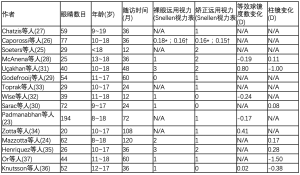
Full table
虽然更长时间的长波紫外线(UVA)照射(9至10分钟)似乎具有更大的效果,但与遵循标准Dresden方案观察到的屈光变化相比,快速CXL术后的屈光变化没有临床意义(表2)[8-15]。与采用标准Dresden CXL方案观察到的视力变化相比,采用和不采用经上皮离子渗透CXL术后的视力变化也没有临床意义(表3)[16-21]。
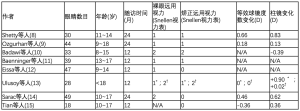
Full table
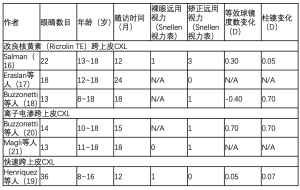
Full table
虽然CXL主要用于治疗成人和儿童进展性圆锥角膜,但CXL可能在小儿屈光矫正中对一小部分未能通过传统治疗方法(例如框架眼镜、隐形眼镜或贴片)的患者起作用。目前的小儿屈光手术包括准分子激光治疗,例如光屈光性角膜切除术 (PRK) 和激光辅助原位角膜磨镶术 (LASIK)、有晶状体人工晶状体 (pIOL)、晶状体切除术和屈光性晶状体置换术[38]。由于CXL可实现角膜压平效果,因此在矫正儿童散光和近视方面具有潜在作用。与目前的儿童屈光手术技术相比,CXL具有更好的安全性。
安全性
微生物角膜炎虽然不常见,但在采用标准和快速CXL方案术后的儿童中都有报道 [39,40]。在儿童人群中,没有关于跨上皮CXL术后微生物性角膜炎的报道。根据不同的CXL方案,也有报道称一些儿童出现短暂的轻度视物模糊[8,10-12,14,19,24,33,35-37]。Godefrooij等人报道了1例在CXL术后1年和2年持续性视物模糊、矫正远视力下降的病例[29]。Eissa等人发现儿童快速CXL术后内皮细胞计数减少,但这种变化没有统计学意义[12]。总体而言,儿童CXL具有良好的安全性,视力威胁并发症的发生率较低。
结论
儿童CXL术是一令人振奋且相对较新的领域,迄今为止在治疗儿童进展性圆锥角膜方面已展示出光明前景。该方案也已被证明具有相对较好的安全性。鉴于小儿圆锥角膜更严重及更具侵袭性,一旦发现进展,应考虑将CXL作为儿童的治疗方法。有些人甚至认为应该在确诊时即向父母推荐CXL作为治疗方法,而不是等到病情进展时[37]。CXL术后1年裸眼和矫正远视力的视力改善,具有屈光参差性弱视或有屈光参差性弱视风险经传统治疗失败的儿童群体,CXL为其散光和近视治疗打开了大门。为了更好地了解CXL对小儿屈光和角膜曲率的影响,阻止圆锥角膜进展的有效性以及CXL的安全性,需要进行更大规模、前瞻性、随机对照试验和更长随访期的基于儿童人群的进一步研究。
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Joann Kang, Viral Juthani and Roy S. Chuck) for the series “Refractive Surgery” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2018.12.02). The series “Refractive Surgery” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wollensak G, Spörl E, Seiler T. Treatment of keratoconus by collagen cross linking. Ophthalmologe 2003;100:44-9. [Crossref] [PubMed]
- Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 2003;135:620-7. [Crossref] [PubMed]
- Soeters N, Van der Lelij A, van der Valk R, et al. Corneal crosslinking for progressive keratoconus in four children. J Pediatr Ophthalmol Strabismus 2011;48 Online:e26-9.
- Sabti S, Tappeiner C, Frueh BE. Corneal Cross-Linking in a 4-Year-Old Child With Keratoconus and Down Syndrome. Cornea 2015;34:1157-60. [Crossref] [PubMed]
- Hersh PS, Stulting RD, Muller D, et al. United States Multicenter Clinical Trial of Corneal Collagen Crosslinking for Keratoconus Treatment. Ophthalmology 2017;124:1259-70. [Crossref] [PubMed]
- Perez-Straziota C, Gaster RN, Rabinowitz YS. Corneal Cross-Linking for Pediatric Keratcoconus Review. Cornea 2018;37:802-9. [Crossref] [PubMed]
- Schumacher S, Oeftiger L, Mrochen M. Equivalence of biomechanical changes induced by rapid and standard corneal cross-linking, using riboflavin and ultraviolet radiation. Invest Ophthalmol Vis Sci 2011;52:9048-52. [Crossref] [PubMed]
- Shetty R, Nagaraja H, Jayadev C, et al. Accelerated corneal collagen cross-linking in pediatric patients: two-year follow-up results. Biomed Res Int 2014;2014:894095 [Crossref] [PubMed]
- Ozgurhan EB, Kara N, Cankaya KI, et al. Accelerated corneal cross-linking in pediatric patients with keratoconus: 24-month outcomes. J Refract Surg 2014;30:843-9. [Crossref] [PubMed]
- Badawi AE. Accelerated corneal collagen cross-linking in pediatric keratoconus: One year study. Saudi J Ophthalmol 2017;31:11-8. [Crossref] [PubMed]
- Baenninger PB, Bachmann LM, Wienecke L, et al. Pediatric Corneal Cross-linking: Comparison of Visual and Topographic Outcomes Between Conventional and Accelerated Treatment. Am J Ophthalmol 2017;183:11-6. [Crossref] [PubMed]
- Eissa SA, Badr Eldin N, Nossair AA, et al. Primary Outcomes of Accelerated Epithelium-Off Corneal Cross-Linking in Progressive Keratoconus in Children: A 1-Year Prospective Study. J Ophthalmol 2017;2017:1923161 [Crossref] [PubMed]
- Ulusoy DM, Goktas E, Duru N, et al. Accelerated corneal crosslinking for treatment of progressive keratoconus in pediatric patients. Eur J Ophthalmol 2017;27:319-25. [Crossref] [PubMed]
- Sarac O, Caglayan M, Uysal BS, et al. Accelerated versus standard corneal collagen cross-linking in pediatric keratoconus patients: 24 months follow-up results. Cont Lens Anterior Eye 2018;41:442-7. [Crossref] [PubMed]
- Tian M, Jian W, Sun L, et al. One-year follow-up of accelerated transepithelial corneal collagen cross-linking for progressive pediatric keratoconus. BMC Ophthalmol 2018;18:75. [Crossref] [PubMed]
- Salman AG. Corneal Biomechanical and Anterior Chamber Parameters Variations after 1-year of Transepithelial Corneal Collagen Cross-linking in Eyes of Children with Keratoconus. Middle East Afr J Ophthalmol 2016;23:129-34. [Crossref] [PubMed]
- Eraslan M, Toker E, Cerman E, et al. Efficacy of Epithelium-Off and Epithelium-On Corneal Collagen Cross-Linking in Pediatric Keratoconus. Eye Contact Lens 2017;43:155-61. [Crossref] [PubMed]
- Buzzonetti L, Petrocelli G. Transepithelial corneal cross-linking in pediatric patients: early results. J Refract Surg 2012;28:763-7. [Crossref] [PubMed]
- Henriquez MA, Rodriguez AM, Izquierdo L Jr. Accelerated Epi-On Versus Standard Epi-Off Corneal Collagen Cross-Linking for Progressive Keratoconus in Pediatric Patients. Cornea 2017;36:1503-8. [Crossref] [PubMed]
- Buzzonetti L, Petrocelli G, Valente P, et al. Iontophoretic transepithelial corneal cross-linking to halt keratoconus in pediatric cases: 15-month follow-up. Cornea 2015;34:512-5. [Crossref] [PubMed]
- Magli A, Chiariello Vecchio E, Carelli R, et al. Pediatric keratoconus and iontophoretic corneal crosslinking: refractive and topographic evidence in patients underwent general and topical anesthesia, 18 months of follow-up. Int Ophthalmol 2016;36:585-90. [Crossref] [PubMed]
- Léoni-Mesplié S, Mortemousque B, Touboul D, et al. Scalability and severity of keratoconus in children. Am J Ophthalmol 2012;154:56-62.e1. [Crossref] [PubMed]
- Padmanabhan P, Rachapalle Reddi S, Rajagopal R, et al. Corneal Collagen Cross-Linking for Keratoconus in Pediatric Patients-Long-Term Results. Cornea 2017;36:138-43. [Crossref] [PubMed]
- Mazzotta C, Traversi C, Baiocchi S, et al. Corneal Collagen Cross-Linking With Riboflavin and Ultraviolet A Light for Pediatric Keratoconus: Ten-Year Results. Cornea 2018;37:560-6. [Crossref] [PubMed]
- Soeters N, van der Valk R, Tahzib NG. Corneal cross-linking for treatment of progressive keratoconus in various age groups. J Refract Surg 2014;30:454-60. [Crossref] [PubMed]
- Caporossi A, Mazzotta C, Baiocchi S, et al. Riboflavin-UVA-induced corneal collagen cross-linking in pediatric patients. Cornea 2012;31:227-31. [Crossref] [PubMed]
- Chatzis N, Hafezi F. Progression of keratoconus and efficacy of pediatric [corrected] corneal collagen cross-linking in children and adolescents. J Refract Surg 2012;28:753-8. Erratum in: J Refract Surg 2013;29:72. [Crossref] [PubMed]
- McAnena L, O'Keefe M. Corneal collagen crosslinking in children with keratoconus. J AAPOS 2015;19:228-32. [Crossref] [PubMed]
- Godefrooij DA, Soeters N, Imhof SM, et al. Corneal Cross-Linking for Pediatric Keratoconus: Long-Term Results. Cornea 2016;35:954-8. [Crossref] [PubMed]
- Sarac O, Caglayan M, Cakmak HB, et al. Factors Influencing Progression of Keratoconus 2 Years After Corneal Collagen Cross-Linking in Pediatric Patients. Cornea 2016;35:1503-7. [Crossref] [PubMed]
- Uçakhan ÖÖ, Bayraktutar BN, Saglik A. Pediatric Corneal Collagen Cross-Linking: Long-Term Follow-Up of Visual, Refractive, and Topographic Outcomes. Cornea 2016;35:162-8. [Crossref] [PubMed]
- Wise S, Diaz C, Termote K, et al. Corneal Cross-Linking in Pediatric Patients With Progressive Keratoconus. Cornea 2016;35:1441-3. [Crossref] [PubMed]
- Toprak I, Yaylali V, Yildirim C. Visual, Topographic, and Pachymetric Effects of Pediatric Corneal Collagen Cross-linking. J Pediatr Ophthalmol Strabismus 2017;54:84-9. [Crossref] [PubMed]
- Zotta PG, Diakonis VF, Kymionis GD, et al. Long-term outcomes of corneal cross-linking for keratoconus in pediatric patients. J AAPOS 2017;21:397-401. [Crossref] [PubMed]
- Henriquez MA, Villegas S, Rincon M, et al. Long-term efficacy and safety after corneal collagen crosslinking in pediatric patients: Three-year follow-up. Eur J Ophthalmol 2018;28:415-8. [Crossref] [PubMed]
- Knutsson KA, Paganoni G, Matuska S, et al. Corneal collagen cross-linking in paediatric patients affected by keratoconus. Br J Ophthalmol 2018;102:248-52. [Crossref] [PubMed]
- Or L, Rozenberg A, Abulafia A, et al. Corneal Cross-Linking in Pediatric Patients: Evaluating Treated and Untreated Eyes-5-Year Follow-Up Results. Cornea 2018;37:1013-7. [Crossref] [PubMed]
- Stahl ED. Pediatric refractive surgery. Curr Opin Ophthalmol 2017;28:305-9. [Crossref] [PubMed]
- Steinwender G, Pertl L, El-Shabrawi Y, et al. Complications From Corneal Cross-linking for Keratoconus in Pediatric Patients. J Refract Surg 2016;32:68-9. [Crossref] [PubMed]
- Kodavoor SK, Sarwate NJ, Ramamurhy D. Microbial keratitis following accelerated corneal collagen cross-linking. Oman J Ophthalmol 2015;8:111-3. [Crossref] [PubMed]

刘华
河南大学人民医院。医学硕士,河南大学人民医院眼科学研究生在读,本科毕业于长治医学院临床医学专业,2020年考入河南大学人民医院眼科学专业。研究方向及范围:眼表疾病与角膜病。(更新时间:2021/8/12)
(本译文仅供学术交流,实际内容请以英文原文为准。)
Cite this article as: Park S. Collagen cross-linking for pediatric refractive correction. Ann Eye Sci 2018;3:59.


