
Transnasal endoscopic approach for orbital apical cavernous hemangiomas: a case report
Introduction
Cavernous hemangioma is the most common primary benign orbital tumor in adults, which constitutes 6% of all orbital tumors (1). Female patients were obviously more than male ones, and recent study seems to indicate the levels of circulating estrogen/progesterone influence these lesions (2). The orbital cavernous hemangioma usually appears as a solitary, unilateral, well-circumscribed, round-to-oval condition, with preferential involvement of the middle third of the orbit, in the intraconal space lateral to the optic nerve (3). The most common symptom and sign of orbital cavernous hemangioma was proptosis and can be accompanied by dislocation of the globe (4). However, some cavernous hemangioma lodged deep in the orbital apex may cause minimal proptosis but progressive visual impairment. Modern imaging techniques usually improve the accuracy of diagnosis and help to differentiate from other orbital tumors mimic cavernous hemangioma, such as schwannoma, meningioma and neurofibroma. The typical appearance of cavernous hemangioma located in the lateral part of the middle third of the orbit on CT is an apple shape configuration. In contrast, the cavernous hemangioma occupied the orbital apex, having characteristic pear-shaped aspect (5). A typical orbital cavernous hemangioma presents as a homogeneous mass showing in MRI scans [isointense to muscle in T1-weighted images; hyperintense in T2-weighted images (6)]. In dynamic MRI scans, the contrast enhancement is progressive overtime, starting from one point or portion, rather than a wide area (7). The cavernous hemangioma consists of interconnected, endothelially lined vascular channels and abundant stroma (8). Local hemodynamic shift could open and promote “budding” of the vascular channels into interstitial substance. During the neovascular network extends into surrounding tissue, it induces a fibrous capsule at the interface, and finally forms a well-defined and compact capsule. The extent of critical structures has been expropriated by tumor growth may be more clinically relevant in the crowed orbital apex. This pathophysiological characteristic of orbital cavernous hemangioma can be crucial in surgical decision and affect surgical outcomes (9).
A wide variety of therapies have been used for orbital cavernous hemangioma. Observation is suggested in asymptomatic patients. The patients should be followed with continuous visual functional tests and imaging examinations. Surgical treatment should be considered if the patients present apparent visual field progression, or minor deficits but evidence for active growth of the tumor (9). The location of orbital cavernous hemangioma acts as a crucial factor when selecting the surgical approach. If the tumor laid extraconal or intraconal, not involving the orbital apex, an anterior approach is indicated (10,11). In case where the tumor located above or lateral to the optic nerve, lateral orbitotomy should be considered as a valid option (12). Several neurosurgical approaches were also applied remove the lesions located in the posterior third of the orbit (13,14). The transnasal endoscopic approach has been invaluable in treating extraconal or intraconal cavernous hemangiomas located medial or inferomedial to the optic nerve (15).
However, removal of cavernous hemangiomas located in the orbital apex remained a challenge. These cases can cause progressive functional deficits, and even minor incremental growth can have major impact in the densely packed region. On the other hand, because of often tenacious attachments to fixed apical structures, even careful surgical removal can imperil vision. Herein, the authors described a fully endoscopic approach to an intraconal cavernous hemangioma wedged between the optic nerve, the medial and inferior rectus muscles of the orbital apex. And the patient had a good vision when she come to our hospital. Although the tumor could be effectively managed by surgery, the complex anatomical structures of orbital apex and the grave concerns about operated risks and complications of the patient become a trouble during this operation. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/aes-20-92).
Case presentation
This study was approved by the Ethics Committee of Peoples’ Hospital of Ningxia Hui Autonomous Region and conducted in accordance with the Declaration of Helsinki.
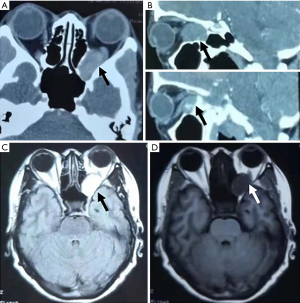
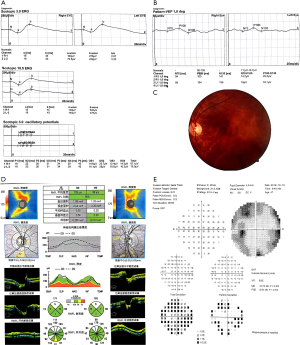
A 47-year-old female was admitted to our hospital on October 22nd, 2018, complaining of dizziness for 2 months. The patient had no pertinent medical or ocular history, and she denied visual loss, proptosis or pain. Best-corrected vision was 20/20 OD and 20/30 OS, with a left relative afferent pupillary defect (RAPD). Intraocular pressures were 16 mmHg OD and 15 mmHg OS. The left globe was relatively proptotic by 2 mm and fully mobile. Slit lamp biomicroscopy showed lens opacity for both eyes. The dilated funduscopic examination, visual evoked potential and electroretinography were normal OU. Goldman visual field testing showed superonasal and inferotemporal peripheral vision defect OS. Orbital imaging demonstrated a large lesion wedged between the optic nerve and the medial and inferior rectus muscles of her left eye (Figure 1). Figure 2 displayed the VEP, OCT, photograph of fundus and perimetry of the patient before surgery. The patient was diagnosed as cavernous hemangioma for left eye and cataract for both eyes.
The patient received orbital surgery under general anesthesia on October 24th, 2018. An endoscopic unilateral anterior and posterior ethmoidectomy, and sphenoidotomy were carried out using a 4.0 mm and 45° endoscope. The medial wall of orbit was exposed to the orbital apex until the junction between the small wing of sphenoid bone and optical canal was visualized. The posterior bone of orbital medial wall was removed, and orbital fasciae was incised in order to fully expose the tumor. At this point, the adhesion between tumor and medial rectus was separated by a careful endoscopic-assisted dissection. Then the tumor was grasped with Alice tissue forcep and removed with gentle steady traction after the majority of tumor was released from its attachments (Figure 3A,B,C). The hemostatic sponge with diluted epinephrine hydrochloride (<1:100,000) was placed into the nasal cavity to prevent bleeding. A piece of esterified hyaluronic sponge fulfilled with dexamethasone was then overlaid on the surgical wound.
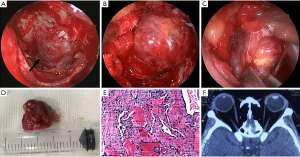
Of this case, a 2 cm × 1.5 cm vascular appearing lesion (Figure 3D) was successfully removed from the left orbital apex without perioperative complications. Histopathology confirmed the diagnosis of cavernous hemangioma (Figure 3E). Intravenous broad-spectrum antibiotics and betamethasone was given daily for 5 days after surgery. The patient was discharged on October 31st, 2018 and ophthalmic examinations revealed BCVA of 20/20 OS and extraocular motility remained full OU with no diplopia. The afferent pupillary defect had resolved. Hertel exophthalmometry revealed no exophthalmos OS, and postoperative orbital CT confirmed complete resection of the tumor (Figure 3F). The patient was advised to avoid nose-blowing and strenuous activity for 2 weeks.
Reviews were carried out at 2 weeks, 1 month, 3 months. The patient completed her last follow-up visit on January 3rd, 2019 (Figure 4). Goldman visual field testing showed no visual defect progression during follow-up. The treatment results were satisfactory, with no after-effects and adverse reactions during follow-up. The patient expressed her deep gratitude for our treatment.
Discussion
The surgical outcome may be closely related to the microanatomic relations between tumor and orbital structures. Furthermore, because of the crowding of critical visual structures into orbital apex, the management of cavernous hemangiomas of this location is more complex. Managements for apical lesions medial to the optic nerve include transcaruncular (16) and transcranial (17) approaches, with or without medial rectus muscle detachment. However, these traditional surgical approaches provide limited space for surgical manipulation. And these approaches may pose a high risk of injury to the optic nerve and significant visual loss.
Herman et al. (18) first reported a transnasal endoscopic approach for removing orbital hemangioma in 1999. Since then, several authors have described their experience with removing orbital apex cavernous via an endoscopic-assisted endonasal approach (19-21). The recent introduction of transnasal endoscopic surgery offers a direct pathway to the inferomedial aspect of orbital apex without crossing the optic canal. In addition, the endoscope provides a wider view of the operative field, a high resolution of visualization and illumination which facilitate the surgery.
Considering the risk of unchecked tumor growth into orbital apical structures, and the risk of tumor removal from them, each case requires thoughtful analysis. The continued observation of visual field testing and serial imaging are indicated for those patients with normal ophthalmic findings. But the preoperative examinations revealed our patient had appeared superonasal and inferotemporal peripheral vision defect. Therefore, we decided to operate at once because an earlier intervention may stave off more intimate fusion between the tumor and critical structures.
In accordance with several reported surgeries, we began with an ethmoidotomy and a sphenoidotomy to easily access to the medial and inferior wall of the orbit and completely expose the tumor and optic canal. The removal of posterior orbital medial wall and orbital fasciae were added for enhanced exposure of the tumor. Some authors advocate to detach the medial rectus muscle from the globe to enable better manipulation of the medial rectus muscle at the orbital apex (22). In our case, because the tumor was located at the orbital entrance of the optic canal and behind the annulus of Zinn, we reached the tumor without medial rectus muscle detachment. We found there was an adherence between the inferior rectus medial rectus and the capsule of the tumor. Thus, we dissected the adhesion with suction apparatus and directly incised the medial fascia around the tumor. Simultaneously, we kept pulling out the tumor with a gentle steady strength and completely remove the tumor at last. Generally, some surgeons used portion of the perpendicular plate of the ethmoid harvested from the septum or a thin Medpor sheet to reconstruct the medial wall (22). However, because the bony defect was smaller than half the medial wall in our case, we had not implemented this reconstructed step. Postsurgical diplopia or enophthalmos were not observed during follow-up.
There are some disadvantages to the endonasal endoscopic approach. The first disadvantage is related to the use of only two visual dimensions. However, a third visual dimension can be simulated by moving the endoscope actively, thereby providing some sense of depth. Furthermore, the use of endoscopic sinus surgery involves a limited degree of space for movement of instruments. Another limitation of this approach is reflected in dealing with hemorrhage during operation. But we found it will be helpful to control bleeding with gentle steady pulling the tumor while dissecting adhesion after the majority of tumor was released from its attachments.
Conclusions
In conclusion, we believe the transnasal endoscopic surgery to be a promising technique for cavernous hemangiomas that are located deep in orbital apex. This approach provides direct pathway to tumor with limiting morbidity, maximal surgical field and ample illumination. Thus, the procedure represents a safe and less invasive management.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (81960184), Ningxia Key Research and Development Program (Special Talents) (2018beb04023) and Ningxia Key Research and Development Program (General Subject) (2018YBZD1445).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Xiulan Zhang) for the series “Ophthalmology Clinical Research” published in Annals of Eye Science. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/aes-20-92
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes-20-92). The series “Ophthalmology Clinical Research” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:997-1008. [Crossref] [PubMed]
- Jayaram A, Lissner GS, Cohen LM, et al. Potential correlation between menopausal status and the clinical course of orbital cavernous hemangiomas. Ophthalmic Plast Reconstr Surg 2015;31:187-90. [Crossref] [PubMed]
- McNab AA, Selva D, Hardy TG, et al. The anatomical location and laterality of orbital cavernous haemangiomas. Orbit 2014;33:359-62. [Crossref] [PubMed]
- McNab AA, Wright JE. Cavernous haemangiomas of the orbit. Aust N Z J Ophthalmol 1989;17:337-45. [Crossref] [PubMed]
- Kloos R, Mourits D, Saeed P, et al. Orbital apex cavernous hemangioma--beware of the pear! Acta Ophthalmol 2013;91:e328-9. [Crossref] [PubMed]
- Ansari SA, Mafee MF. Orbital cavernous hemangioma: role of imaging. Neuroimaging Clin N Am 2005;15:137-58. [Crossref] [PubMed]
- Dallaudiere B, Benayoun Y, Boncoeur-Martel M, et al. Imaging features of cavernous hemangiomas of the orbit. J Radiol 2009;90:1039-45. [Crossref] [PubMed]
- Rootman DB, Heran MK, Rootman J, et al. Cavernous venous malformations of the orbit (so-called cavernous haemangioma): a comprehensive evaluation of their clinical, imaging and histologic nature. Br J Ophthalmol 2014;98:880-8. [Crossref] [PubMed]
- Harris GJ. Cavernous hemangioma of the orbital apex: pathogenetic considerations in surgical management. Am J Ophthalmol 2010;150:764-73. [Crossref] [PubMed]
- Aymard PA, Langlois B, Putterman M, et al. Management of orbital cavernous hemangioma-evaluation of surgical approaches: report of 43 cases. J Fr Ophtalmol 2013;36:820-9. [Crossref] [PubMed]
- Rosen N, Priel A, Simon GJ, et al. Cryo-assisted anterior approach for surgery of retroocular orbital tumours avoids the need for lateral or transcranial orbitotomy in most cases. Acta Ophthalmol 2010;88:675-80. [Crossref] [PubMed]
- Moufarreh M, Benbouzid MA, Ghailan MR, et al. Removal of lateral orbital wall for management of orbital cavernous hemangioma. J Fr Ophtalmol 2014;37:18-22. [Crossref] [PubMed]
- Lazar M, Rothkoff L, Drey JP. Treatment and long-term outcome of patients with orbital cavernomas. Am J Ophthalmol 2005;139:753-author reply 753. [Crossref] [PubMed]
- Schick U, Dott U, Hassler W. Surgical treatment of orbital cavernomas. Surg Neurol 2003;60:234-44; discussion 244. [Crossref] [PubMed]
- Bleier BS, Castelnuovo P, Battaglia P, et al. Endoscopic endonasal orbital cavernous hemangioma resection: global experience in techniques and outcomes. Int Forum Allergy Rhinol 2016;6:156-61. [Crossref] [PubMed]
- Goldberg RA, Mancini R, Demer JL. The transcaruncular approach: surgical anatomy and technique. Arch Facial Plast Surg 2007;9:443-7. [Crossref] [PubMed]
- Scheuerle AF, Steiner HH, Kolling G, et al. Treatment and long-term outcome of patients with orbital cavernomas. Am J Ophthalmol 2004;138:237-44. [Crossref] [PubMed]
- Herman P, Lot G, Silhouette B, et al. Transnasal endoscopic removal of an orbital cavernoma. Ann Otol Rhinol Laryngol 1999;108:147-50. [Crossref] [PubMed]
- McKinney KA, Snyderman CH, Carrau RL, et al. Seeing the light: endoscopic endonasal intraconal orbital tumor surgery. Otolaryngol Head Neck Surg 2010;143:699-701. [Crossref] [PubMed]
- Locatelli M, Carrabba G, Guastella C, et al. Endoscopic endonasal removal of a cavernous hemangioma of the orbital apex. Surg Neurol Int 2011;2:58. [Crossref] [PubMed]
- Castelnuovo P, Dallan I, Locatelli D, et al. Endoscopic transnasal intraorbital surgery: our experience with 16 cases. Eur Arch Otorhinolaryngol 2012;269:1929-35. [Crossref] [PubMed]
- Wu W, Selva D, Jiang F, et al. Endoscopic transethmoidal approach with or without medial rectus detachment for orbital apical cavernous hemangiomas. Am J Ophthalmol 2013;156:593-9. [Crossref] [PubMed]
Cite this article as: An N, Piao J, Yang W, Zhu J, Liu J, Li Q. Transnasal endoscopic approach for orbital apical cavernous hemangiomas: a case report. Ann Eye Sci 2020;5:29.



