
Navigation technology/eye-tracking in ophthalmology: principles, applications and benefits—a narrative review
Introduction
The increasing capabilities of technological inventions have significantly broadened their applications in medicine and ophthalmology. Smartphones and multipurpose devices are now being increasingly used for diagnostics, telemedicine applications, and self-monitoring of eye diseases (1). Software technology has been impactful in ophthalmic informatics, examples being deep learning and pattern recognition, to differentiate abnormal images or outcomes from normative databases (2).
Another stunning example is motion-based navigation technology in both ophthalmic imaging and treatment. Several imaging instruments use a real-time eye-tracking system, which helps to reduce motion artefacts and increase signal-to-noise ratio in imaging acquisition such as optical coherence tomography (OCT), microperimetry, and fluorescence and color imaging (3,4). Navigation in ophthalmic surgery has been firstly applied in laser vision corrective surgery (5,6), navigated retinal photocoagulation (7), and positioning guidance of intraocular lenses (IOL) during cataract surgery (8). It has emerged as one of the most reliable representatives of technology as it continues to transform surgical interventions into safer, more standardized, and more predictable procedures with better outcomes.
The meaning of navigation in surgery is conceptualized into “location of target”, “safe reach of the target”, “current anatomic location”, or “evaluation of treatment accuracy”. Apart from these important orientation questions, surgical navigation is also used as a measurement tool and an information center for providing surgeons with the right information at the right time.
In this review, we summarise the basic principles and applications of navigation technology in modern ophthalmology. We will review contributions in ophthalmic imaging, anterior and posterior segment laser treatments, and surgery. We present the following article in accordance with Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/aes-20-127).
Eye-tracking in ophthalmic imaging
When following the task of precisely measuring a particular structure of the eye, eye movements induce an artefact, which is difficult to “recalculate”. Therefore, compensation for eye movements was implemented to make these measurements more reproducible.
One of the first applications was using eye-tracking for laser Doppler velocimetry to measure ocular hemodynamics where an eye-tracking device compensated the eye movements and ensured an artefact-free image. This tracker was based on Purkinje images, which are reflections of infrared light on different surfaces of the eye. These reflection changes upon movements are evaluated and recalculated into eye movements (9). An image-based eye tracker was later implemented into Heidelberg retinal angiography to compensate for eye movements and improve the image quality. According to the manufacturer website, the TruTrack® Active Eye Tracking (Spectralis, Heidelberg Engineering, Heidelberg, Germany) is a “patented technology that uses a second laser beam to actively track the eye during scanning to avoid motion artefact” (3,4).
However, for OCT a different kind of compensation is needed to allow high-resolution and motion artefact-free images in depth. In 2004, Ferguson et al. presented the first prototype of an eye tracker that compensated eye movements for enhanced OCT imaging on the retina. Using this tracker, which was based on the detection of natural structures of the retina, the image quality could be improved, and the deviation in the measurement position was reduced from 3.4 to 0.45 pixels (10).
OCT tracking devices are separated into hardware and software-based systems. Hardware-based systems use an additional hardware implemented into the optical design of an instrument that captures additional data to calculate eye motion online or offline. In software-based systems the motion patterns are approximated either by comparing the acquired data to a reference (OCT) image or by considering some prior assumptions about the nature of the eye motion. Hardware-based systems by nature also require software to calculate eye motions from the obtained data. Most of these utilized software are variations of cross-correlation-based image registration techniques (3). Commercially available OCT systems and their eye-trackers will be briefly described in the following chapters.
Heidelberg engineering (TruTrack Active Eye Tracking) uses a real-time eye-motion system to track eye movements and guide OCT to the proper location for repeating the B-scans if there was eye movement during scanning. The tracking system is an effective solution for transverse movements, while axial correction still requires a software correction (11). Vienola et al. describe this eye tracker to be an image-based eye tracker obtained from 1,000 points in the infrared imaging channel (12). The tracking accuracy in the Heidelberg Engineering System in a model eye was measured to be a mean maximal error of 15 µm in the lateral and horizontal position. The axial resolution of the OCT in depth is 5 to 7 µm (13). It was also shown to reduce the percentage of motion artefacts when compared to a system without eye-tracking.
The Zeiss Cirrus device, in addition to 3-D raster scans, acquires two diagonal B-scans with different wavelengths mainly for axial motion correction (3).
The RTVue system uses an image-based tracker from an infrared full-field fundus camera with a 20 to 30 Hz refreshment rate (3,14).
The Canon OCT-HS100 uses both automatic anterior eye alignment (pupil tracking) and fundus tracking for better compensation of involuntary eye motions. The detailed principle is described in a report by Carrasco et al. where a pupil-based tracker was used, and simulations revealed the ability to track lateral movements of ±3.5 mm or rotational eye movements of ±1.2 ° with an accuracy of approximately 49 µm (without combination of the fundus tracking) (15).
The Physical Sciences Inc. (PSI) OCT system is based on a dithering beam that is locked on reflectance changes from single retinal features within the optic nerve head or blood vessels. The eye motion signal is used to control the OCT scanning mirrors to maintain the scanning grid on its retinal target, except in the PSI system where the beam is controlled with additional tracking mirrors (14).
Another advanced eye-tracking principle for OCT is image distortion-based tracking. With devices using this principle, a scanning laser ophthalmoscope (SLO) images the eye with a frame rate of 30 Hz, but extracts eye motion at much higher rates by analyzing distortions within sections of each captured frame. These extracted eye motion signals are transformed into tracking signals and combined with the signals that drive the OCT galvo mirrors (14).
Sugita et al. described an eye tracker in polarization-sensitive OCT (PS-OCT). To extract the retinal position shift information, first, a template (typically consisting of 64×64 pixels) with a fiducial marker such as a thick vessel branch (of the subject retina) is chosen and extracted from the SLO images recorded as a pre-processing step. During the sequence of the data acquisition of the PS-OCT sub-system, the SLO images taken in parallel are analyzed so that the cross-correlation between the template image and each SLO image is calculated. From the cross-correlation values, the best-matched location is found, and the two-dimensional shift information is obtained. This template matching calculation is done immediately after the data acquisition and image construction for each SLO frame (16).
OCT angiography (OCTA) is a new technology for imaging retinochoroidal vasculature, and reduction of motion artefacts using eye-tracking technology is of utmost importance to assure reproducible image analysis (17). The benefit of using an eye-tracking device in OCTA has been demonstrated previously. The use of eye-tracking systems results in higher reproducibility and repeatability in the measurement of vascular flow (18) and a significantly reduced amount of motion artefacts in conjunction with significantly stronger signal strength as well as a lower variability in vessel density (19). Although the acquisition time with active eye-tracking was significantly longer than without the authors concluded that eye-tracking provides superior image quality (19).
Intraocular lens placement in cataract surgery using eye-tracking
Cataract surgery is one of the most common procedures in ophthalmology. If, after cataract surgery, astigmatism of more than 1.25 dioptres remains uncorrected, the patient will still need spectacles postoperatively. This is the case in 20% to 30% of patients (20). With the advent of toric IOLs an option became available to correct this astigmatism in patients who desire to remain spectacle free. However, the accuracy of positioning these lenses is important to ensure the highest effectivity in astigmatism compensation. Every 5 degrees of misalignment will decrease the anticipated effect by 17% (12,21). For correctly centered and rotated implantation with optimal incision location, surgeons use a three-step process (marking of horizontal axis with ink on slit lamp; alignment of line mark; intraoperative alignment of IOL and axis). Visser et al. showed that a commonly used three-step ink marker process leads to a mean error in IOL placement of approximately 5 degrees. In cases with higher astigmatism, this leads to the need for retreatment (22).
With the ongoing development of navigation and eye-tracking, computer-assisted systems for optimized toric IOL implantation have become available. The two most common systems are the Zeiss Callisto® and Verion® from Alcon originally developed as the SG3000 by SensoMotoric Instruments, GmbH in 2010. The first step includes a diagnostic image on a unit that does keratometry and acquires a high-resolution reference image in which the limbal vessels, scleral vessels, and iris characteristics are visible. Based on these extracted “landmarks”, the diagnostic image (including landmarks such as the center of the pupil, steep and flat axis) is registered automatically onto the live image of a microscope during lens implantation.
Several peer-reviewed publications have investigated computer/eye-tracking guided IOL implantation. Most of them report significantly better results when using an eye-tracking and computer-guided system with regards to mean toric misalignment of residual astigmatism. The mean toric misalignment ranges from 2.0°±1.86° (standard deviation) (23) to 2.96°±2.54° (24) with a computer-guided system as compared to a mean range of toric misalignment from 2.88°±2.18° (25) to 4.33°± 2.72° (26) for manual ink marker implantation. The mean residual astigmatism is published to range from −0.29±0.22 D (27) to 0.10 ± 0.08 D (26) in computer-guided treatments versus a range from −0.46±0.25 D (27) to 0.22±0.14 D (23). Mayer et al., in addition, analyzed the required time for toric IOL alignment to be significantly faster in computer-guided systems as compared to the time the alignment requires when using manual markers (37.2±11.9 vs. 59.4±15.3 s; P=0.003) (23). One publication compared the Zeiss Callisto and the Alcon Verion systems without identifying the superiority of either. The authors found that the systems are not interchangeable as there was a relatively large proportion of cases where a difference in axis rotation between each system was >3°. The authors also state that it was rare to identify a large deviation between both systems (28).
Navigation in refractive laser surgery
Myopia and hyperopia are the most frequent eye disorders across the world (29). In North America, nearly 9% of children aged 5–17 years reported myopia of at least −0.75 dioptres, and an additional 13% had at least +1.25 dioptres hyperopia (29,30). The interest of the ophthalmic community in the surgical treatment of refractive disorders has been long-standing. Most surgical procedures in the past, such as radial keratotomy and keratomileusis, represented breakthroughs in surgical developments (31-33), but in reality suffered from some degree of imprecision.
With the advent of excimers lasers, the procedure became less invasive. It led to the first photorefractive keratectomy (PRK) or keratomileusis in situ (without separation of the corneal layer) conducted by Trokel in 1983 in animal studies and human trials in 1987 (14,34). The FDA approved PRK in 1995 and laser-in-situ keratomileusis (LASIK) in 2002. The flying-spot scanning technology used worldwide for customized LASIK procedure was invented by Dr. Lin (5,6). With the advent of this relatively precise “knife” the need for a supported application arose. In the following years, the lasers were improved to small scanning beams to allow a smooth ablation bed and less energy per spot (35).
Originally the laser beam was placed manually to the correct ablation zone. With the increasingly small laser beam, the desire rose for assisted laser positioning that could compensate eye movements to avoid the decentration of the laser from the correct ablation zone. However, when no paralyzing is available, the whole treatment is dependent on passive fixation of the patient. Even when perfect fixation of the patient takes place, the eye is subject to uncontrollable saccadic eye movements of up to 170 mm/s (25,36,37). A misplacement of the excimer laser beam can lead to serious side effects such as halos, glare, and diplopia (38), but also a higher number of higher-order aberrations (39,40).
The first method to compensate and control these eye movements for refractive laser was described by Preussner et al. in 1990 for compensating eye movements in laser keratotomy (41). This prototype consisted of a light-emitting land marker fixed by 3 mm deep hooks to the limbus of the patients’ eye. These land markers were tracked and checked for an alignment accuracy of the laser beam and target of 5 µm. The laser was blocked in cases of deviations larger than 5 µm (40). The key drawback of this solution was its invasive nature.
In 1992, Phoenix Laser System Inc. was granted the first patent describing a “system (that) also includes tracking system for following the movements of the subject tissue, for example an eye during surgery. The tracking system is fast enough to track such movement, preferably at the maximum repetition rate of the laser plus a sufficient margin for safety” (42). This system was the first using a camera image and image processing techniques to analyze and compensate eye movements. Several patents with the same goal and different approaches were submitted in the following years (43-45). Shortly thereafter, further improvements and inventions on eye-tracking technologies were introduced, such as an increased tracking rate (nowadays reaching up to 4 kHz) and recognition of cyclorotation as well as compensating for parallax error when analyzing a 2D image of a 3D elevated structure (16).
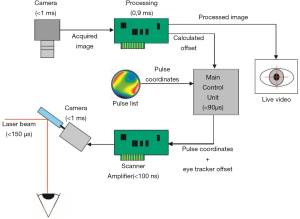
The key set-up of all eye-trackers in refractive laser is basically the same and is well illustrated in Figure 1. It consists of one or more cameras observing the patient’s eye, an image processing unit analyzing the features of the image(s) and providing position information that finally is processed by the main control unit of the refractive laser to either block the laser from further release or reposition the actual ablation pattern (23).
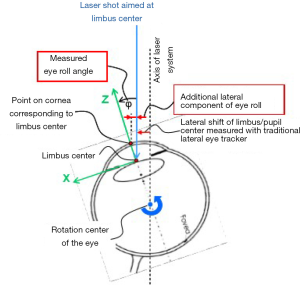
The first eye-tracking devices used a black and white charge-coupled device image sensor with an acquisition rate of 50 Hz (46) using the pupil border to calculate and track the pupil center. The offset of the actual pupil center with the pupil center of the initially acquired reference image (which contains the information of the desired laser locations) leads to the position information of the next laser spot. There are different modalities available to image the pupil. Either imaging based on a “photographic” image where structures are extracted from infrared light, coaxially positioned to the eye, which is reflected by the retina and then imaged as a bright circle on dark background (8). Over the course of the time, other image features for tracking were either alternatively or in conjunction with pupil tracking added to the tracking method (limbus, iris structures, and limbal vessel tracking). This allowed firstly to be independent of pupil size and to work with either a non-dilated or dilated pupil, but also allowed detection of cyclorotational movements (47,48). The recent technological advancement is 6D (six-degrees) tracking, which compensates the parallactic error created by the curvature of the cornea. While pure limbal and pupil-based tracking calculates a translational movement of a 2D plane (iris), the eye actually rotates with a curved cornea. This leads to a deviation between the desired spot (center of the pupil) and the applied spot (Figure 2) (37,49). This becomes especially relevant if a wavefront-guided refractive correction is used. In wavefront-guided treatments, the higher-order aberrations are measured, and a laser ablation profile is calculated to compensate for these higher-order aberrations. However, without using 6D tracking compensation, the success in eliminating higher-order aberrations was limited in clinical studies (50-54).
While the quality of the tracking can be influenced by various factors, such as pupil size, the most commonly stated influence factors are the image acquisition speed and the latency of the laser positioning. The pulse positioning accuracy increases with a decrease in laser positioning latency. A latency of 15 ms usually corresponds to a positioning error of 3.5 mm, eye tracker latencies of below 1.5 ms result in accuracy below 0.5 mm (37).
With increasing tracking frequency, the pulse positioning error reduces. A tracking frequency of below 100 Hz usually relates to inaccuracy of 1.5 mm, while an increased tracking frequency of 1,000 Hz reduces this value to below 0.5 mm. Therefore, it is important to observe frequency and latency together to minimize positioning error (37).
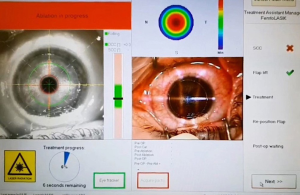
The initial eye-tracking systems with 50 Hz image acquisition were analyzed in a real clinical setting and did not lead to a significant increase in accuracy when compared to a manual positioning technique. Both methods showed an average deviation of planned to actual accuracy of 0.55±0.30 mm (range, 0.10 to 1.4 mm), and in the manual centration group, 0.43±0.23 mm (range, 0.10 to 1.0 mm) (55). The currently available tracking rate reaches 4 kHz. The latency is reported to be between 10 and 3 ms (56,57). Qazi et al. analyzed the impact of using an eye tracker on patient’s visual quality. They concluded that the use of infrared pupil tracking improved uncorrected visual acuity, produced more predictive refractive outcomes, and fewer large centration outliers (57). Eye-tracking in refractive laser surgery became the gold standard and accepted to be superior to manual spots, especially when using small spot sizes (Figure 3).
Navigation in posterior segment treatments
The most frequent non-surgical treatment on the retina is photocoagulation, which is indicated in numerous conditions. It was introduced as early as 1945 by Meyer-Schwickerath using sunlight and then further improved by the use of Xenon light followed by the use of laser light to deliver energy for photocoagulation (58,59). Until approximately 2010, laser systems included a slit lamp-based delivery able to apply photocoagulation even in a fixed pattern style rapidly. While the speed of application and pain experience are the biggest challenges in peripheral treatment, in focal application, the challenge is to deliver a treatment avoiding sensitive areas such as the macula and the optic disc. Often, pathologic areas that need to be targeted (such as leakage sources or ischemic areas) cannot be identified easily in ophthalmoscopic images from the slit lamp. Generally, a fluorescein image is obtained and placed aside the slit lamp like a road map to help locate the needed areas.
Combining a fluorescein angiography image display with laser treatment has been successfully applied previously. For instance, Jean and Kreissig described such a display, which has been used for several years. Usage was successful and aimed to improve therapeutic precision in hitting lesions. At the same time, the procedure was relatively complicated and the fluorescein angiography images had to be mounted in a special device (60). Other groups have used similar devices, for example, Mainster et al. reported more than 200 photocoagulations and found the setup to be useful (61).
The idea of applying retinal tracking to enhance laser treatment by a navigating system has been investigated for some time. In parallel to the previously mentioned angio-mounted slit lamp systems, several groups investigated a computerized laser system to compensate for eye movements. Naess et al. reported the development of a computerized laser system to compensate for eye movements based on a digital image processing unit (62). Jean et al. were able to reposition the aiming beam based on fundus structure recognition in real-time and achieved robustness of 90% in laboratory settings (63). In 1991, Yu et al. presented a further tracking-assisted system based on fundus structure correlation and used scanning mirrors to compensate movements. This system did not achieve clinical relevance as the repetition rate was only 1 to 2 Hz (64). In 1999, Berger and Shin presented their computer-based system, highlighting how such image-guided macular laser therapy should facilitate accurate targeting of treatable lesions and less unintentional retinal injury when compared with standard techniques (65).
Starting in the late 1980s, Markov et al. presented the first hybrid retinal tracking, which was considerably improved by the US Air Force Academy, University of Texas, and University of Wyoming over the next two decades (66). Wright et al. published initial in vivo results in rabbits in 2000 (67). While tracking speed was found to be slower in vivo than in vitro, the system overall performed well and exceeded requirements for clinical application. The requirements for this system have evolved to retinal tracking rates equal to or better than 10 deg/s, laser pointing accuracy better than 100 µm at the retinal surface, uniform lesion formation within 5% of apparent size and depth, and system reaction time of no more than 5 milliseconds (62). However, retinal photocoagulation was not a finally realized application. While the system was tested successfully in animals for this purpose, in practice, it was applied to eye movement measurements and tattoo removal in humans in vivo (68).
In 2009, the Navilas (OD-OS, Teltow, Germany) system was described by Liesfeld et al. consisting of a digital imaging system with a reflex-free color or infrared image in combination with an eye-tracking system compensating for eye movements during retinal laser photocoagulation or thermal stimulation (7,69,70).
Navilas includes a unique pre-planning capability that allows users to outline and review the treatment strategy before execution of the therapy. With Navilas, users can plan caution zones where the laser must not fire while planning the points of interest where the laser shall fire. Either the images obtained from the Navilas system or from other diagnostic devices showing retinal vessel structures, such as OCT, indocyanine green angiography, fluorescein angiography, and OCTA can be imported and registered. Having a set of retinal images is helpful for a better understanding of the pathology and especially in deciding the positioning of the optimal treatment locations. The user is then annotating the images with the desired treatment locations. Options include either single spots or several spot patterns, such as a hexagonally oriented pattern. The locations are drawn via the graphical user interface directly onto the digital diagnostic images of the retina. The spacing between spots and the spot size can be individually defined. After treatment, Navilas stores the treatment plan in a digital report that can be exported and shared. The user can execute the treatment plan with the help of computerized image guidance (Figure 4).
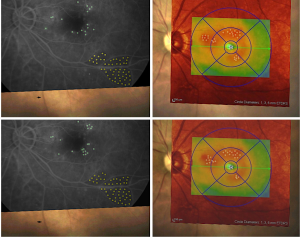
During the actual treatment, the image acquired with Navilas, together with the related treatment locations (reference image), is automatically registered onto the live image obtained from the retina by localization of retinal structures, including vessels and other prominent structures. Each image from the live stream is registered to its preceding image for tracking the retina in subsequent steps. The difference in the position of the extracted retinal structures is recalculated into an eye movement. Scanners then reposition the laser beam according to the calculated positioning difference.
Unlike all other eye-tracking systems for retinal laser, the Navilas is the only system that has been shown to be robust in vivo as early as 2011 (71,72). The group at the University of California San Diego first published results regarding the clinical accuracy of the system in diabetic macular edema (DME), which outperformed manual laser treatment by an increased microaneurysm hit rate with navigated photocoagulation (72). Such a high treatment accuracy with Navilas appears to correspond to favorable clinical outcomes (73). Superior accuracy was reconfirmed by Kernt et al., showing that 95% of the spots are within a 100 µm radius of the target (74). Regarding pain perception during treatment, several comparison studies reported a more favorable outcome with navigated laser than conventional laser treatment for both central and peripheral applications (75-80).
The introduction of anti-VEGF has shifted the standard treatment paradigm to the use of monthly anti-vascular endothelial growth factor (VEGF) injections due to the favorable results in visual acuity compared to macular laser photocoagulation in DME (81). Although studies did not show a benefit of conventional laser further improving the visual acuity gain or the number of required anti-VEGF injections (82,83), laser was used as a rescue option in almost 50% of cases (14). Other studies using navigated laser instead of conventional have demonstrated a reduction in the need for anti-VEGF with stable visual acuity (84-86). Furthermore, by using navigation, a more advanced treatment to the periphery is feasible, which allows for more targeted treatments. Singer et al. used navigation with imported angiographic images to locate peripheral ischemia as the basis of their treatment approach of rebound macular edema (87). Navigated photocoagulation due to its image-based principle has been conceptually introduced in remote treatments as part of teleophthalmology (88).
Narrative
This search has drawn historical facts and recent knowledge from ophthalmic and optics literature and, therefore, covers a very broad spectrum. It is possible that some information has not been included. As this area is subject to ongoing research, updates to this topic will be essential with new developments.
Summary
Ophthalmology is traditionally a technological leader among medical and surgical specialties. Early adoption of the principles of navigation technology is an example of why this is so. Navigation in ophthalmology spans from imaging diagnostics to most advanced laser and surgical procedures, such as the treatment of refractive errors, accurate placement of artificial IOLs, or most selective laser treatment of retinal diseases such as diabetic retinopathy. Navigation has made our decision making more detailed and our treatments more accurate and safer. The natural results of this are more standardized and predictable procedures with better treatment outcomes and increased patient satisfaction.
Literature search
We used all available public domains to search for scientific literature published in English, German, French, Russian, and Spanish languages. The key words included: eye tracking, optics, navigated surgery, imaging, refractive and surgery, excimer laser. There was no time limitation for published reports.
Highlights
- Diagnostic ophthalmic imaging uses features of eye-tracking.
- Practically all excimer lasers use eye-tracking technology to ensure accurate execution of corneal tissue ablation.
- Modern cataract surgery includes eye-tracking assisted implantation of IOLs.
- Navigated retinal laser represents a new generation system with increased accuracy of treatment.
Acknowledgments
We wish to thank Kay-Uwe Amthor, PhD, and Stefanie Gehrke from OD-OS, Inc. for assistance with preparing this manuscript and to Dr. Hamed Anwar from Moorfields Eye Hospital Abu Dhabi for providing intraoperative images.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/aes-20-127
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes-20-127). UR is an employee of OD-OS, Inc. IK serves as an unpaid editorial member of Annals of Eyes Science from May 2020 to Apr 2022.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hogarty DT, Hogarty JP, Hewitt AW. Smartphone use in ophthalmology: What is their place in clinical practice? Surv Ophthalmol 2020;65:250-62. [Crossref] [PubMed]
- Grzybowski A, Brona P, Lim G, et al. Artificial intelligence for diabetic retinopthy screening: a review. Eye (Lond) 2020;34:451-60. [Crossref] [PubMed]
- Baghaie A, Yu Z, D’Souza RM. Involuntary eye motion correction in retinal optical coherence tomography: Hardware or Software Solution? Med Image Anal 2017;37:129-45. [Crossref] [PubMed]
- Solomon JD, Ladas J. Toric outcomes: computer-assisted registration versus intraoperative aberrometry. J Cataract Refract Surg 2017;43:498-504. [Crossref] [PubMed]
- Lin JT. Mini-excimer laser corneal reshaping using a scanning device. Proc SPIE 1994;2131:228-36. [Crossref]
- Ober MD, Kernt M, Cortes MA, et al. Time required for navigated macular laser photocoagulation treatment with the Navilas®. Graefes Arch Clin Exp Ophthalmol 2013;251:1049-53. [Crossref] [PubMed]
- Liesfeld B, Teiwes W, Huppertz M, Amthor K-U, “Ophthalmoscope Including Therapy Beam Targeting,” US8545020 (B2), issued Oct. 01, 2013.
- Swinger CA, Lai ST. Ophthalmic surgical laser and method. United States US6325792B1, filed August 8, 1994, and issued December 4, 2001.
- Lischka T. Untersuchung eines Eye Tracker Prototypen zur automatischen Operationsmikroskopsteuerung - Klinik und Poliklinik für Augenheilkunde Universitätsklinikum Hamburg-Eppendorf (Dissertation). Hamburg 2007 - Crane HD, Steele CM (1985) Generation-V dual-Purkinje eyetracker. Applied Optics 24:527-537.
- Ferguson RD, Hammer DX, Paunescu LA, et al. Tracking optical coherence tomography. Opt Lett 2004;29:2139-41. [Crossref] [PubMed]
- SPECTRALIS SPIRIT - Confocal Fundus Image | Heidelberg Engineering. Available online: https://business-lounge.heidelbergengineering.com/gb/en/products/spectralis-spirit/spectralis-spirit/trutrack-active-eye-tracking/. Accessed September 1, 2020.
- Vienola KV, Braaf B, Sheehy CK, et al. Real-time eye motion compensation for OCT imaging with tracking SLO. Biomed Opt Express 2012;3:2950-63. [Crossref] [PubMed]
- Barteselli G, Bartsch DU, Viola F, et al. Accuracy of the Heidelberg Spectralis in the alignment between near-infrared image and tomographic scan in a model eye: a multicenter Study. Am J Ophthalmol 2013;156:588-92. [Crossref] [PubMed]
- Trokel SL, Srinivasan R, Braren B. Excimer laser surgery of the cornea. Am J Ophthalmol 1983;96:710-5. [Crossref] [PubMed]
- Carrasco-Zevallos O, Nankivil D, Keller B, et al. Pupil tracking optical coherence tomography for precise control of pupil entry position. Biomed Opt Express 2015;6:3405-19. [Crossref] [PubMed]
- Sugita M, Zotter S, Pircher M, et al. Motion artifact and speckle noise reduction in polarization sensitive optical coherence tomography by retinal tracking. Biomed Opt Express 2013;5:106-22. [Crossref] [PubMed]
- Mihailovic N, Lauermann JL, Schubert F, et al. Expression of motion artifacts in OCT-Angiography imaging in healthy subjects using two different devices. Klin Monbl Augenheilkd 2019;236:1115-21. [PubMed]
- Alnawaiseh M, Brand C, Bormann E, et al. Quantification of macular perfusion using optical coherence tomography angiography: repeatability and impact of an eye-tracking system. BMC Ophthalmol 2018;18:123. [Crossref] [PubMed]
- Lauermann JL, Treder M, Heiduschka P, et al. Impact of eye-tracking technology on OCT-Angiography imaging quality in age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2017;255:1535-42. [Crossref] [PubMed]
- Visser N, Berendschot TT, Bauer NJ, et al. Accuracy of toric intraocular lens implantation in cataract and refractive surgery. J Cataract Refract Surg 2011;37:1394-402. [Crossref] [PubMed]
- Webers VSC, Bauer NJC, Visser N, et al. Image-guided system versus manual marking for toric intraocular lens alignment in cataract surgery. J Cataract Refract Surg 2017;43:781-8. [Crossref] [PubMed]
- Visser N, Bauer NJ, Nuijts RM. Toric intraocular lenses: historical overview, patient selection, IOL calculation, surgical techniques, clinical outcomes, and complications. J Cataract Refract Surg 2013;39:624-37. [Crossref] [PubMed]
- Mayer WJ, Kreutzer T, Dirisamer M, et al. Comparison of visual outcomes, alignment accuracy, and surgical time between 2 methods of corneal marking for toric intraocular lens implantation. J Cataract Refract Surg 2017;43:1281-6. [Crossref] [PubMed]
- Montes de Oca I, Kim EJ, Wang L, et al. Accuracy of toric intraocular lens axis alignment using a 3-dimensional computer-guided visualization system. J Cataract Refract Surg 2016;42:550-5. [Crossref] [PubMed]
- Bueeler M, Mrochen M, Seilet T. Effects of eye movements during refractive surgery with a scanning spot laser Proc SPIE 2003;150:4951. [Crossref]
- Elhofi AH, Helaly HA. Comparison between digital and manual marking for toric intraocular lenses: A randomized trial. Medicine (Baltimore) 2015;94:e1618. [Crossref] [PubMed]
- Sklar HA, Frank AM, Ferrer OM, et al. Method and apparatus for precision laser surgery. United States US5098426A, filed February 6, 1989, and issued March 24, 1992.
- Hura AS, Osher RH. Comparing the Zeiss Callisto Eye and the Alcon Verion image guided system toric lens alignment technologies. J Refract Surg 2017;33:482-7. [Crossref] [PubMed]
- Hashemi H, Fotouhi A, Yekta A, et al. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J Curr Ophthalmol 2017;30:3-22. [Crossref] [PubMed]
- Kleinstein RN, Jones LA, Hullett S, et al. Refractive error and ethnicity in children. Arch Ophthalmol 2003;121:1141-7. [Crossref] [PubMed]
- Barraquer JI. Keratomileusis. Int Surg 1967;48:103-17. [PubMed]
- Barraquer JI. Lamellar keratoplasty. (Special techniques). Ann Ophthalmol 1972;4:437-69. [PubMed]
- Fyodorov SN, Sarkizova MB, Kurasova TP. Corneal biomicroscopy following repeated radial keratotomy. Ann Ophthalmol 1983;15:403-7. [PubMed]
- Krueger RR, Rabinowitz YS, Binder PS. The 25th anniversary of excimer lasers in refractive surgery: historical review. J Refract Surg 2010;26:749-60. [Crossref] [PubMed]
- Palanker D. Evolution of concepts and technologies in ophthalmic laser therapy. Annu Rev Vis Sci 2016;2:295-319. [Crossref] [PubMed]
- Arba Mosquera S, Arbelaez MC. Use of a six-dimensional eye-tracker in corneal laser refractive surgery with the SCHWIND AMARIS TotalTech laser. J Refract Surg 2011;27:582-90. [Crossref] [PubMed]
- Arba-Mosquera S, Aslanides IM. Analysis of the effects of Eye-Tracker performance on the pulse positioning errors during refractive surgery. J Optom 2012;5:31-7. [Crossref]
- Mrochen M, Kaemmerer M, Mierdel P, et al. Increased higher-order optical aberrations after laser refractive surgery: a problem of subclinical decentration. J Cataract Refract Surg 2001;27:362-9. [Crossref] [PubMed]
- Bueeler M, Mrochen M. Simulation of eye-tracker latency, spot size, and ablation pulse depth on the correction of higher order wavefront aberrations with scanning spot laser systems. J Refract Surg 2005;21:28-36. [Crossref] [PubMed]
- Prakash G, Agarwal A, Ashok Kumar D, et al. Comparison of laser in situ keratomileusis for myopic astigmatism without iris registration, with iris registration, and with iris registration-assisted dynamic rotational eye tracking. J Cataract Refract Surg 2011;37:574-81. [Crossref] [PubMed]
- Preussner PR, Richard G. Automatic compensation for the effect of eye movements in laser keratotomy. Fortschr Ophthalmol 1990;87:302-4. [PubMed]
- Singer MA, Tan CS, Surapaneni KR, et al. Targeted photocoagulation of peripheral ischemia to treat rebound edema. Clin Ophthalmol 2015;9:337-41. [Crossref] [PubMed]
- Burkhalter JH, Downes GR, Frey RW, et al. Laser beam delivery and eye tracking system. European Union EP1147753A3, filed April 18, 1995, and issued November 26, 2003.
- Frey RW, Burkhalter JH, Gray GP, et al. Laser beam delivery and eye tracking system. European Union EP0757579A4, filed April 18, 1995, and issued August 5, 1998.
- Muller DF, Sacharoff AC. Method and system for laser thermokeratoplasty. World Intellectual Property Organization WO1994007424A1, filed October 7, 1993, and issued April 14, 1994.
- Gobbi PG, Carones F, Brancato R, et al. Automatic eye tracker for excimer laser photorefractive keratectomy. J Refract Surg 1995;11:S337-42. [PubMed]
- Bueeler M, Mrochen M. Limitations of pupil tracking in refractive surgery-systematic error in the determination of corneal locations. J Refract Surg 2004;20:371-8. [Crossref] [PubMed]
- Polat O, Inan S, Baysal Z, et al. Comparison of navigated laser and conventional single-spot laser system for induced pain during panretinal photocoagulation. Lasers Med Sci 2020;35:687-93. [Crossref] [PubMed]
- Bueeler M, Mrochen M, Grunding M, et al. 6-D eye tracking. Cataract & Refract Surgery Today 2008 January:30-33.
- Huppertz M, Schmidt E, Teiwes W. Eye tracking and refractive surgery. In: MacRae S, Krueger R, Applegate R. editors. Customized Corneal Ablation: The Quest for Supervision. SLACK Inc.; Thorofare, NJ: 2001. Pp.149-160.
- Kohnen T, Bühren J, Kühne C, et al. Wavefront-guided LASIK with the Zyoptix 3.1 system for the correction of myopia and compound myopic astigmatism with 1-year follow-up: Clinical outcome and change in higher order aberrations. Ophthalmology 2004;111:2175-85. [Crossref] [PubMed]
- Moshirfar M, Espandar L, Meyer JL, et al. Prospective randomized trial of wavefront-guided laser in situ keratomileusis with the CustomCornea and CustomVue laser systems. J Cataract Refract Surg 2007;33:1727-33. [Crossref] [PubMed]
- Mrochen M., Kaemmerer M, Seiler T. Clinical results of wavefront-guided laser in situ keratomileusis 3 months after surgery. J Cataract Refract Surg 2001;27:201-7. [Crossref] [PubMed]
- Taylor NM, Eikelboom RH, van Sarloos PP, et al. Determining the accuracy of an eye tracking system for laser refractive surgery. J Refract Surg 2000;16:S643-6. [PubMed]
- Pallikaris I, McDonald MB, Siganos D, et al. Tracker-assisted photorefractive keratectomy for myopia of -1 to -6 diopters. J Refract Surg 1996;12:240-7. [PubMed]
- Krueger RR. In perspective: eye tracking and autonomous laser radar. J Refract Surg 1999;15:145-9. [PubMed]
- Qazi MA, Pepose JS, Sanderson JP, et al. Novel objective method for comparing ablation centration with and without pupil tracking following myopic laser in situ keratomileusis using the Bausch & Lomb Technolas 217A. Cornea 2009;28:616-625. [Crossref] [PubMed]
- Meyer-Schwickerath G. Further progress in the field of light coagulation. Trans Ophthalmol Soc U K 1957;77:421-37. [PubMed]
- Ophthalmic surgery method using non-contact scanning laser. United States US5520679A, filed March 25, 1994, and issued May 28, 1996.
- Jean B, Kreissig I. Das Simultan-Fluo-Angioskop: Eine Methode Zur Makulanahen Laserbehandlung. Klin Monbl Augenheilkd 1986;189:258-9. [Crossref] [PubMed]
- Mainster MA, Yannuzzi LA, Heacock G, et al. A slitlamp comparator system for macular photocoagulation. Retina (Philadelphia, PA) 1990;10:57-9. [Crossref] [PubMed]
- Naess E, Molvik T, Ludwig DA, et al. Computer-assisted laser photocoagulation of the retina: A hybrid tracking approach. J Biomed Opt 2002;7:179-89. [Crossref] [PubMed]
- Jean B, Kazmierczak H, Grunert T, et al. Real time eye tracking - principles and quantification. Klin Monatsbl Augenheilkd 1991;198:538-43. [Crossref] [PubMed]
- Yu JJ, Ho YT, Ko LS, et al. Eye-tracking system for computer-assisted photocoagulation. Ophthalmic Surg 1991;22:260-5. [PubMed]
- Berger JW, Shin DS. Computer-vision-enabled augmented reality fundus biomicroscopy. Ophthalmology 1999;106:1935-41. [Crossref] [PubMed]
- Markov MS, Rylander HG, Welch AJ. Real-time algorithm for retinal tracking. IEEE Transactions on Bio-Medical Engineering 1993;40:1269-81. [Crossref] [PubMed]
- Wright CH, Barrett SF, Ferguson RD, et al. Initial in vivo results of a hybrid retinal photocoagulation system. J Biomed Opt 2000;5:56-61. [Crossref] [PubMed]
- Wright CH, Barrett SF, Welch AJ. Design and development of a computer-assisted retinal laser surgery system. J Biomed Opt 2006;11:041127. [Crossref] [PubMed]
- Gologorsky D, Rosen RB, Giovinazzo J, et al. Navigated Retina Laser Therapy as a Novel Method for Laser Retinopexy of Retinal Tears. Ophthalmic Surgery, Lasers and Imaging Retina 2018;49:e206-9. [Crossref] [PubMed]
- Liesfeld B, Amthor KU, Dowell D, et al. Navigating comfortably across the retina.” In World Congress on Medical Physics and Biomedical Engineering, September 7 - 12, 2009, Munich, Germany, 243-46. Springer, Berlin, Heidelberg, 2009.
- Kernt M, Cheuteu R, Vounotrypidis E, et al. Focal and panretinal photocoagulation with a navigated laser (NAVILAS®). Acta Ophthalmol 2011;89:e662-4. [Crossref] [PubMed]
- Kozak I, Oster SF, Cortes MA, et al. Clinical evaluation and treatment accuracy in diabetic macular edema using navigated laser photocoagulator NAVILAS. Ophthalmology 2011;118:1119-24. [Crossref] [PubMed]
- Kozak I, Kim JS, Oster SF, et al. Focal navigated laser photocoagulation in retinovascular disease: Clinical results in initial case series. Retina (Philadelphia, Pa.) 2012;32:930-5. [Crossref] [PubMed]
- Kernt M, Cheuteu RE, Cserhati S, et al. Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas). Clin Ophthalmol 2012;6:289-96. [Crossref] [PubMed]
- Amoroso F, Pedinielli A, Astroz P, et al. Comparison of pain experience and time required for pre-planned navigated peripheral laser versus conventional multispot laser in the treatment of diabetic retinopathy. Acta Diabetol 2020;57:535-41. [Crossref] [PubMed]
- Chalam KV, Murthy RK, Brar V, et al. Evaluation of a novel, non-contact, automated focal laser with integrated (NAVILAS®) fluorescein angiography for diabetic macular edema. Middle East Afr J Ophthalmol 2012;19:158-62. [Crossref] [PubMed]
- Chhablani J, Mathai A, Rani P, et al. Comparison of conventional pattern and novel navigated panretinal photocoagulation in proliferative diabetic retinopathy. Invest Ophthalmol Vis Sci 2014;55:3432-8. [Crossref] [PubMed]
- Inan UU, Polat O, Inan S, et al. Comparison of pain scores between patients undergoing panretinal photocoagulation using navigated or pattern scan laser systems. Arq Bras Oftalmol 2016;79:15-8. [Crossref] [PubMed]
- Neubauer AS, Langer J, Liegl R, et al. Navigated macular laser decreases retreatment rate for diabetic macular edema: A comparison with conventional macular laser. Clin Ophthalmol 2013;7:121-8. [PubMed]
- Pineros OE. Tracker-assisted versus manual ablation zone centration in laser in situ keratomileusis for myopia and astigmatism. J Refract Surg 2002;18:37-42. [PubMed]
- Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med 2015;372:1193-203. [Crossref] [PubMed]
- Baker CW, Glassman AR, Beaulieu T, et al. Effect of initial management with aflibercept vs laser photocoagulation vs observation on vision loss among patients with diabetic macular edema involving the center of the macula and good visual acuity: A randomized clinical trial. JAMA 2019;321:1880-94. [Crossref] [PubMed]
- Elman MJ, Bressler NM, Qin H, et al. Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2011;118:609-14. [Crossref] [PubMed]
- Barteselli G, Kozak I, El-Emam S, et al. 12-month results of the standardised combination therapy for diabetic macular oedema: intravitreal bevacizumab and navigated retinal photocoagulation. Br J Ophthalmol 2014;98:1036-41. [Crossref] [PubMed]
- Herold TR, Langer J, Vounotrypidis E, et al. 3-year-data of combined navigated laser photocoagulation (Navilas) and intravitreal ranibizumab compared to ranibizumab monotherapy in DME patients. PLoS One 2018;13:e0202483. [Crossref] [PubMed]
- Liegl R, Langer J, Seidensticker F, et al. Comparative evaluation of combined navigated laser photocoagulation and intravitreal ranibizumab in the treatment of diabetic macular edema. PLoS One 2014;9:e113981. [Crossref] [PubMed]
- Salz JJ, Stevens CA. LADARVision LASIK Hyperopia Study Group. LASIK correction of spherical hyperopia, hyperopic astigmatism, and mixed astigmatism with the LADARVision excimer laser system. Ophthalmology 2002;109:1647-56; discussion 1657-8. [Crossref] [PubMed]
- Kozak I, Payne JF, Schatz P, et al. Teleophthalmology image-based navigated retinal laser therapy for diabetic macular edema: a concept of retinal telephotocoagulation. Graefes Arch Clin Exp Ophthalmol 2017;255:1509-13. [Crossref] [PubMed]
Cite this article as: Kozak I, Rahn U. Navigation technology/eye-tracking in ophthalmology: principles, applications and benefits—a narrative review. Ann Eye Sci 2021;6:6.


