
A case of infectious endophthalmitis misdiagnosed as uveitis
Introduction
Intraocular foreign bodies may cause infectious or aseptic endophthalmitis (1) with ensuing progressive damage to the intraocular structure (2). Common foreign bodies requiring surgical removal include metal fragments, eyelashes, graphite, and glass (3). The location of such foreign bodies can be determined by CT scan, ultrasound biomicroscopy (UBM), anterior segment optical coherence tomography (AS-OCT), ultrasound, X-ray, and other imaging modalities (4), with UBM and AS-OCT particularly useful for accurately determining object size and location (3). Removal of intraocular foreign bodies can prevent progressive damage to the intraocular structure and reduce the risks of aseptic or infectious intraocular inflammation. Here we describe a case of delayed endophthalmitis after open eye trauma diagnosed and treated in our hospital. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/aes-20-138).
Case presentation
A 68-year-old female visited our hospital after sustaining a nail injury to the right eye when hitting a nail with a hammer on July 13, 2019. Computed tomography revealed injury to the right conjunctiva and cornea. CT scan shows no intraocular foreign body. On the same day, right eye corneal laceration suture, sclera exploration, and anterior chamber drug injection of cefuroxime sodium were performed in our hospital, but no foreign body was found during the operation.
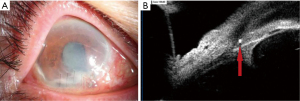
On July 24, follow-up ophthalmic examination results were as follows: right eye intraocular pressure, 7.7 mmHg; visual acuity, 0.05; correction, no improvement. A 3-mm spindle-shaped white granuloma was clearly apparent in the right corneal limbus at 7–8 o’clock, but there was no obvious inflammatory reaction in the anterior chamber (Figure 1A). Gonioscopic examination revealed a 2-mm rod-shaped translucent foreign body in the right eye at 1 o’clock (Figure 1B). UBM showed a speckled strong echo in the right iris at 7 o’clock (Figure 1C). However, the patient felt no discomfort. After the consultation, the patient was advised to return to the clinic for examination of anterior chamber inflammation.

On August 12, she underwent another corner angle examination, which revealed that the foreign body had moved to the corner around 10 o’clock and resembled a translucent oil drop. Due to the large range of movement and lighter weight compared to the aqueous humor, the possibility of eye ointment residue was considered. In addition, the foreign body at 7 o’clock manifested as a strong echo, and was identified tentatively as the rust remaining from the nail. Considering that the small size foreign bodies are moving, hiding and invisible under a microscope, it is difficult to remove during surgery. As well the operation may destruct structures of iris, corneal and anterior chamber without obvious inflammation, and even the risk of foreign body falling into vitreous. The clinical team thus decided to continue close observation after consultation.
On September 16, the patient presented with a red eye, eye pain, and vision loss for one day. On physical examination, right eye intraocular pressure could not be measured using a non-contact tonometer, but intraocular pressure of finger examination was Tn, while hand movement was detected only up to 40 cm (HM/40 cm) with no improvement on correction. The corneal wound suture was loose with hernia of the iris under the right eye, forming a staphyloma. The white scar at the corneal wound was enlarged and exhibited new infiltrating blood vessels, and the white granuloma was about 3 mm in length and clearly visible at 7–8 o’clock in the corneal limbus. These abnormalities were accompanied by conjunctival congestion, corneal misty edema, a shallow anterior chamber, visible fibrinous exudates in the anterior chamber, posterior iris adhesions, a pupil area of 4 mm × 5 mm, absence of light reflection, lens opacity, pigmented plaques on the capsule surface, and no fundus details were visible. (Figure 2A). Re-examination by UBM showed that the right angle of the whole corner of the right eye was closed and revealed a small foreign body at 6–7 o’clock (Figure 2B), while B-mode ultrasonography showed vitreous opacites in the right eye. On September 17, the intraocular pressure of the patient’s right eye was elevated from Tn to T+1, with severe corneal edema and no significant reduction in the inflammatory response of the anterior chamber. The patient was then admitted to the hospital, and administered dual antibiotics of Levofloxacin and Cefuroxime, systemic and local anti-inflammatory and anti-infection treatments, and intraocular pressure-lowering treatments. However, intraocular pressure continued to rise, reaching 45 mmHg on September 18. On September 19, she underwent combined therapies including lensectomy, vitrectomy, posterior iris adhesion release, iris segmentectomy (6–9 o’clock), removal of the anterior chamber foreign body, removal of corneal and scleral lesions, and vitreous gas-liquid exchange. Suspicious foreign bodies overflowed during iris segmentectomy (Figure 3A), but were not collected due to their small size and fragility. Uveitis was considered, so no intravitreal antibiotic injection was performed. Postoperative pathological examination showed anterior chamber exudates, purulent inflammation of the resected iris, and chronic inflammation of the corneal limbus tissue. Bacterial and fungal staining results of the pathological smears of the exudates, iris and corneal limbus tissue were negative. However, culture of the aqueous humor revealed filamentous fungus which reported on September 27.
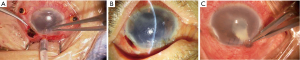
After the operation, the patient received systemic dual antibiotics and Methylprednisolone 80 mg intravenous drip for 6 days, and local anti-inflammatory and anti-infection treatments for six days, and then was discharged from hospital on September 24 (Figure 3B). Considering that the inflammatory reaction in the right eye was controlled and there was no sign of infection, no anti-fungal treatment was added when the culture of the aqueous humor reported on September 27 (Figure 4). By October 8, the corneal edema and the inflammatory response in the anterior chamber had abated. Right eye vision also increased to FC/5 cm, intraocular pressure was reduced to 8 mmHg, and UBM showed no foreign body residue in the right eye. The inflammatory response of the anterior chamber gradually subsided over subsequent reexaminations. The follow-up visit was good and the patient was satisfied with the doctor’s diagnosis and treatment. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
The cases patient was suspected of having uveitis in the right eye rather than infective endophthalmitis for three reasons. First, the intraocular inflammation appeared more than two months after surgery to repair foreign body injury and there was no empyema in the anterior chamber or proliferation of fungi or bacteria in the vitreous cavity. Second, UBM showed no obvious inflammatory exudation in the anterior chamber of the right eye at 7 o’clock, and the fibrous exudate in the anterior chamber was located at 4–5 o’clock, which suggested uveitis caused by eye ointment. Third, the eye ointment dissolved progressively, blocking the trabecular meshwork, resulting in aggravation of the chronic inflammatory response and progressively increasing intraocular pressure. Thus, infectious endophthalmitis was misdiagnosed as uveitis.
There is only one reported case of ophthalmic ointment entering the anterior chamber. That patient received cataract phacoemulsification combined with intraocular lens implantation due to blurred vision. Ten months after surgery, slit lamp examination revealed a 1-mm diameter oil droplet on the surface of the intraocular lens, which ultimately required another operation to remove (5). The foreign body in the upper corner of the right eye of our case was initially short and rod-shaped but changed in both shape and position with time. As the density was lower than the aqueous humor, we speculated that ointment entered the eye and gradually dissolved into translucent oil droplets at body temperature before eventually disappearing. Combined with the iris hernia from corneal wounds found at 5 o’clock during the foreign body removal operation (Figure 3C), we suspect that the primary wound repair was not tightly sealed, and delayed wound healing allowed for development of postoperative infectious endophthalmitis. The surgeon performing the initial procedure recalled that a pressure bandaging method was adopted in order to promote corneal closure, and antibiotic ointment was applied to the conjunctival sac before bandaging to prevent infection. In the future, we will further study the pathogenesis of intraocular inflammation in animal models with ocular ointment in the anterior chamber. This case indicates that eye surgeons should pay close attention to wound sealing and that the patient should be cautiously pressed and bandaged when applying eye ointment after surgery. The patient should also be instructed to avoid forcefully rubbing the eye post-treatment.
Most patients with postoperative infective endophthalmitis will have severe acute inflammatory reactions, but some patients will exhibit chronic intraocular inflammation resembling and often misdiagnosed as uveitis (6). Despite the low incidence of postoperative endophthalmitis (0.04–0.26%), it remains a major concern due to the potential risk of blindness (7). Causes of postoperative inflammation include new primary uveitis, such as sarcoidosis, tuberculosis, and multiple sclerosis, uveitis caused by lens rupture, and postoperative infective endophthalmitis (6). Risk factors for infective endophthalmitis include residual intraocular foreign bodies, injury in rural areas, lens rupture, delayed primary wound closure, and prolapsed eye tissue (8). Most cases of delayed fungal endophthalmitis develop following cataract surgery. One such case of filamentous fungal infection in the corneal scleral tunnel did not appear until one year after cataract surgery (9). The fungal focus was a white lesion on the iris that invaded the corneal limbus, and gradually expanded to the anterior chamber, similar to our case. Therefore, we suspect that the white granuloma at the 7 o’clock scleral limbus was a fungal focus caused by foreign bodies that spread from the site of injury.
It is important to distinguish between sterile postoperative inflammation and infectious endophthalmitis because they require different treatments to avoid recurrence and adverse consequences. Metallic foreign bodies such as iron, copper, and alloys, and non-metallic foreign bodies such as graphite and plant tissue can cause uveitis within a few months to more than one year after entering the eye (10,11). Uveitis manifested mainly as corneal edema, posterior corneal KP, iridocyclitis, or vitreitis (10,12,13). The seminal characteristic of infective endophthalmitis is vitreitis, which may be accompanied by ring corneal infiltration, anterior chamber inflammatory masses, and vitreous bead-like or snowball-like exudates (14,15,16,17). The gold standard for the diagnosis of infective endophthalmitis has always been culture and antibiotic sensitivity. In cases of suspected infection, clinicians can confirm and identify the pathogen by needle aspiration biopsy or vitrectomy to collect intraocular fluid (8). In addition to removing intraocular foreign bodies, vitrectomy can restore the transparency of the refractive medium, resolve vitreoretinopathy, and reduce bacterial inoculum and inflammatory toxins (15).
Conclusions
In cases of open ocular trauma, the treating ophthalmologist must guard against occult intraocular foreign bodies. The possibility of intraocular foreign bodies infected with weakly toxic pathogens should be considered in cases of atypical intraocular inflammation insensitive to antibiotics and steroids. Foreign bodies in the eye should be removed surgically as soon as possible, and the aqueous humor or vitreous humor should be collected for microbial culture in order to determine the need for antibiotic treatment. In addition, eye ointment should be used with care in cases with wounds in the anterior segment of the eye that are not completely closed.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/aes-20-138
Peer Review File: Available at http://dx.doi.org/10.21037/aes-20-138
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes-20-138). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hamanaka N, Ikeda T, Inokuchi N, et al. A case of an intraocular foreign body due to graphite pencil lead complicated by endophthalmitis. Ophthalmic Surg Lasers 1999;30:229-31. [Crossref] [PubMed]
- Amritanand A, John SS, Philip SS, et al. Unusual case of a graphite foreign body in the anterior chamber. Clin Pract 2011;1:e73 [Crossref] [PubMed]
- Graffi S, Tiosano B, Ben Cnaan R, et al. Foreign body embedded in anterior chamber angle. Case Rep Ophthalmol Med 2012;2012:631728 [Crossref] [PubMed]
- Stangos AN, Pournaras CJ, Petropoulos IK. Occult anterior-chamber metallic fragment post-phacoemulsification masquerading as chronic recalcitrant postoperative inflammation. Am J Ophthalmol 2005;139:541-2. [Crossref] [PubMed]
- Katabami Y, Sakata R, Honjo M, et al. Nippon Ganka Gakkai Zasshi 2016;120:310-5. [Foreign Body in the Anterior Chamber 10 Months after Uneventful Cataract Surgery]. [PubMed]
- Amin RM, Hamdy I, Osman IM. Chronic candida endophthalmitis as a cause of intermediate uveitis. BMJ Case Rep 2015;2015:bcr2014208847 [Crossref] [PubMed]
- Rossi EE, Pinheiro AL, Baltatu OC, et al. Differential diagnosis between experimental endophthalmitis and uveitis in vitreous with Raman spectroscopy and principal components analysis. J Photochem Photobiol B 2012;107:73-8. [Crossref] [PubMed]
- Kitahata M, Suzuki T, Oka N, et al. Anterior Segment Optical Coherence Tomography of Patients With Late-Onset Tunnel Fungal Infections With Endophthalmitis After Cataract Surgery. Cornea 2016;35:1138-40. [Crossref] [PubMed]
- Dehghani AR, Rezaei L, Salam H, et al. Post traumatic endophthalmitis: incidence and risk factors. Glob J Health Sci 2014;6:68-72. [Crossref] [PubMed]
- Politis M, Rosin B, Amer R. Ocular Siderosis Subsequent to a Missed Pars Plana Metallic Foreign Body that Masqueraded as Refractory Intermediate Uveitis. Ocul Immunol Inflamm 2018;26:598-600. [PubMed]
- Ugarte M, Nicol DA, Jones NP, et al. Chronic intraocular copper foreign body and candida: a unique combination. Ocul Immunol Inflamm 2009;17:356-60. [Crossref] [PubMed]
- Mete G, Turgut Y, Osman A, et al. Anterior segment intraocular metallic foreign body causing chronic hypopyon uveitis. J Ophthalmic Inflamm Infect 2011;1:85-7. [Crossref] [PubMed]
- Mahmoud A, Messaoud R, Abid F, et al. Anterior segment optical coherence tomography and retained vegetal intraocular foreign body masquerading as chronic anterior uveitis. J Ophthalmic Inflamm Infect 2017;7:13. [Crossref] [PubMed]
- Davis JL. Diagnostic dilemmas in retinitis and endophthalmitis. Eye (Lond) 2012;26:194-201. [Crossref] [PubMed]
- El Chehab H, Renard JP, Dot C. Les endophtalmies post-traumatiques J Fr Ophtalmol 2016;39:98-106. [Post-traumatic endophthalmitis]. [Crossref] [PubMed]
- Bhagat N, Nagori S, Zarbin M. Post-traumatic Infectious Endophthalmitis. Surv Ophthalmol 2011;56:214-251. [Crossref] [PubMed]
- Yildiran ST, Mutlu FM, Saracli MA, et al. Fungal endophthalmitis caused by Aspergillus ustus in a patient following cataract surgery. Med Mycol 2006;44:665-669. [Crossref] [PubMed]
Cite this article as: Zhong LX, Shen H, Shao W, Zheng Y. A case of infectious endophthalmitis misdiagnosed as uveitis. Ann Eye Sci 2021;6:30.



