
Prolonged conjunctivitis mimicking nodular episcleritis as a manifestation of granulomatosis with polyangiitis—a case report
Introduction
Red eye is common in our daily practice. It ranges from non-inflammatory to inflammatory causes. Non-inflammatory such as subconjunctival hemorrhage, pannus etc. Inflammatory causes such as orbital cellulitis, dacryoadenitis, keratitis, scleritis, uveitis etc. (Table 1). As such, we present a case of a prolonged conjunctivitis mimicking nodular episcleritis, which is one of the possible presentations of granulomatosis with polyangiitis (GPA), in accordance with the CARE reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-21-32/rc).
Table 1
| Authors | Ocular manifestation |
|---|---|
| Cocho et al. (1) | Scleritis |
| Robinson et al. (2) | Tarsal-conjunctival disease |
| Messmer et al. (3) | Corneal involvement (interstitial keratitis or PUK) |
| Bullen et al. (4) | Uveitis, |
| Salam et al. (5) | EOM involvement |
| Wardyn et al. (6) | Orbital pseudotumour |
| Danda et al. (7) | Orbital cellulitis |
| Kiratli et al. (8) | Dacryoadenitis |
| Cheung et al. (9) | Subconjunctival hemorrhage |
| Specks et al. (10) | Episcleritis |
| Bullen et al. (4) | Pars planitis |
| Bullen et al. (4) | Pannus |
GPA, granulomatosis with polyangiitis; PUK, peripheral ulcerative keratitis; EOM, extraocular muscle.
Case presentation
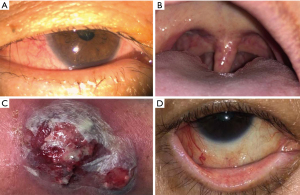
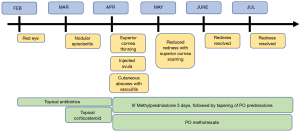
A 57-year-old woman presented with two weeks duration of discomfort, with generalized conjunctival redness and tearing in both eyes. She did not have any constitutional symptoms, rash or any systemic associations. She was a housewife and did not have any medical illnesses or allergies. She was treated for simple conjunctivitis with guttae chloramphenicol 0.5% four times a day for three weeks. Despite the symptomatic relief, the redness persisted. She was commenced on guttae olopatadine hydrochloride 0.2% once daily for two weeks. In the subsequent reviews, both eyes showed segmental redness on the superior bulbar conjunctiva (Figure 1A) which was partially blanched with phenylephrine 1%. She was started on guttae nepafenac 0.1% three times a day and oral celecoxib 200 mg twice a day. Two weeks later, she developed peripheral ulcerative keratitis (PUK) on both eyes. Her physical examination showed injected uvula (Figure 1B) with absence of upper respiratory tract infection. She was admitted for blood and imaging investigations. Her inflammatory markers were raised: ESR was 49 mm/Hr (normal <29) and CRP 13.65 mg/dL (normal <0.3), Antinuclear antibody and C-ANCA tests were positive. The immunology study of her proteinase 3 (PR3) was also positive. All other investigations such as renal profiles, urine full examination microscopic examination (UFEME), CT brain/orbit and chest X-ray were normal. She was diagnosed with GPA and commenced on three days of intensive intravenous methylprednisolone 750 mg once daily and followed by tapering dose of oral prednisolone 1 mg/kg/day. Microscopic polyangiitis was unlikely as her P-ANCA was negative. Giant cell arteritis was ruled out too as she did not have headache or temporal tenderness. In her hospital admission, she developed a vasculitic lesion with cutaneous abscess at the site of intravenous cannula insertion (Figure 1C). Our rheumatology team thereafter commenced on long-term oral methotrexate 10 mg once a week with folic acid 5 mg supplementation. On the subsequent visits, she showed good response to treatment with tapering regime of oral prednisolone. The conjunctiva and sclera remained white, and the areas of cornea thinning scarred up (Figure 1D). Her intraocular pressure, which was raised as a sequelae of corticosteroid, was well controlled with guttae timolol 0.5% twice a day. She was scheduled for regular follow-ups with her antiglaucoma and non-preserved artificial tears. The timeline of events was shown in Figure 2. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013), Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
There are many causes of red eye which associated with systemic disease, ranging from life-threatening to idiopathic. In a patient over 50 years old with raised ESR and vasculitis, giant cell arteritis is a possible cause. However, the lack of headache and temporal tenderness has reduced its possibility. In small vessels vasculitis, microscopic polyangiitis is a differential. However, her immunology results of positive C-ANCA and PR3 has showed a higher probability of GPA (11,12).
GPA or Wegener’s Granulomatosis can be found worldwide. The incidence and prevalence of the disease in Asia is not known. In Japan, it was estimated to be 2.1/million population (13). In Taiwan, Wu et al. estimated 0.37/million based on the National Health Insurance database (14). Cases of GPA have been reported in Malaysia, with involvement in oral cavity (15) and ocular (16). A unilateral eye redness presentation was also reported (17).
GPA is an autoimmune condition of unknown etiology which is characterized by the classic triad of necrotizing granulomatous vasculitis of the respiratory tract, focal segmental glomerulonephritis, and necrotizing vasculitis of small arteries and veins. It has a spectrum of presentation which include nonspecific constitutional symptoms, to ophthalmic, ear-nose-throat, pulmonary, musculoskeletal, renal, nervous system, cutaneous, cardiac and lastly gastrointestinal manifestations (18). Ocular involvement is reported ranging from 28% to 60%, commonly with scleritis. In orbital involvement, it was reported up to 10%, with involvement of orbital cellulitis, dacryocystitis, orbital pseudotumour or involvement of the paranasal sinuses extension, into the orbit (19). Scleritis of the necrotizing type is the most common ocular manifestation (20).
Treatment of the disease requires high doses of corticosteroid. The side effects of the treatment could lead to other complication such as electrolyte imbalance, uncontrolled blood pressure and blood sugar, acute psychosis and long-term side effects such as ocularly glaucoma, cataract, systemically osteoporosis, central abdominal obesity etc. Our reported patient has no co-morbid. The treatment plan is tolerable without adverse event, and she recovers well.
Our case shows a well-documented presentation of GPA: from a simple conjunctivitis to development of PUK and diagnosis of GPA. The subtle evolvement of the early presentation masked the possible underlying connective tissue disease. If resources allowed, it would be favorable for earlier investigation. Success in detecting early subtle systemic signs has succeeded in commencement of treatment, halting the progress of PUK and thus reducing ocular morbidity.
Conclusions
Presentation with red eye is frequent in our daily practice. However, a prolonged duration with incomplete resolution should prompt for suspicion. Diagnosis of GPA is not uncommon. Further investigation is required as the impact of GPA is detrimental, especially with the systemic involvement of the disease.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-21-32/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-21-32/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cocho L, Gonzalez-Gonzalez LA, Molina-Prat N, et al. Scleritis in patients with granulomatosis with polyangiitis (Wegener). Br J Ophthalmol 2016;100:1062-5. [Crossref] [PubMed]
- Robinson MR, Lee SS, Sneller MC, et al. Tarsal-conjunctival disease associated with Wegener's granulomatosis. Ophthalmology 2003;110:1770-80. [Crossref] [PubMed]
- Messmer EM, Foster CS. Vasculitic peripheral ulcerative keratitis. Surv Ophthalmol 1999;43:379-96. [Crossref] [PubMed]
- Bullen CL, Liesegang TJ, McDonald TJ, et al. Ocular complications of Wegener's granulomatosis. Ophthalmology 1983;90:279-90. [Crossref] [PubMed]
- Salam A, Meligonis G, Malhotra R. Superior oblique myositis as an early feature of orbital Wegener's granulomatosis. Orbit 2008;27:203-6. [Crossref] [PubMed]
- Wardyn KA, Ycińska K, Matuszkiewicz-Rowińska J, et al. Pseudotumour orbitae as the initial manifestation in Wegener's granulomatosis in a 7-year-old girl. Clin Rheumatol 2003;22:472-4. [Crossref] [PubMed]
- Danda D, Mathew AJ, Mathew J. Wegener's granulomatosis: a rare presentation. Clin Rheumatol 2008;27:273-5. [Crossref] [PubMed]
- Kiratli H, Sekeroğlu MA, Soylemezoğlu F. Unilateral dacryoadenitis as the sole presenting sign of Wegener's granulomatosis. Orbit 2008;27:157-60. [Crossref] [PubMed]
- Cheung CM, Murray PI, Savage CO. Successful treatment of Wegener's granulomatosis associated scleritis with rituximab. Br J Ophthalmol 2005;89:1542. [Crossref] [PubMed]
- Specks U, Fervenza FC, McDonald TJ, et al. Response of Wegener's granulomatosis to anti-CD20 chimeric monoclonal antibody therapy. Arthritis Rheum 2001;44:2836-40. [Crossref] [PubMed]
- Wiik A. What you should know about PR3-ANCA. An introduction. Arthritis Res 2000;2:252-4. [Crossref] [PubMed]
- Wiik A. Antineutrophil cytoplasmic antibodies in Wegener's granulomatosis. Clin Exp Rheumatol 1993;11:191-201. [PubMed]
- Fujimoto S, Watts RA, Kobayashi S, et al. Comparison of the epidemiology of anti-neutrophil cytoplasmic antibody-associated vasculitis between Japan and the U.K. Rheumatology (Oxford) 2011;50:1916-20.
- Wu CS, Hsieh CJ, Peng YS, et al. Antineutrophil cytoplasmic antibody-associated vasculitis in Taiwan: A hospital-based study with reference to the population-based National Health Insurance database. J Microbiol Immunol Infect 2015;48:477-82. [Crossref] [PubMed]
- Siar CH, Yeo KB, Nakano K, et al. Strawberry gingivitis as the first presenting sign of Wegener's granulomatosis: report of a case. Eur J Med Res 2011;16:331-4. [Crossref] [PubMed]
- Reddy SC, Tajunisah I, Rohana T. Bilateral scleromalacia perforans and peripheral corneal thinning in Wegener's granulomatosis. Int J Ophthalmol 2011;4:439-42. [PubMed]
- Ting DS, Anand S. Persistent Unilateral Conjunctival Inflammation as the First Sign of Granulomatosis with Polyangiitis. Ann Acad Med Singap 2016;45:477-8. [PubMed]
- Tracy CL, Papadopoulos PJ. Granulomatosis with Polyangiitis (GPA, formerly Wegener Granulomatosis) 2019. [updated Oct 09, 2019]. Available online: https://emedicine.medscape.com/article/332622-overview
- Hoffman GS, Kerr GS, Leavitt RY, et al. Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 1992;116:488-98. [Crossref] [PubMed]
- Pakrou N, Selva D, Leibovitch I. Wegener's granulomatosis: ophthalmic manifestations and management. Semin Arthritis Rheum 2006;35:284-92. [Crossref] [PubMed]
Cite this article as: Lee HN, Subrayan V. Prolonged conjunctivitis mimicking nodular episcleritis as a manifestation of granulomatosis with polyangiitis—a case report. Ann Eye Sci 2022;7:10.


