Experimental model of photo-oxidative damage
Introduction
Light represents a double-edged sword in the retina, since it is fundamental for visual perception but results in harmful effects on retinal cells under excessive exposure (1). Indeed, intense light exposure to the retina could contribute to the rapid increase in reactive oxygen species (ROS), thus promoting the onset of oxidative stress if ROS overproduction exceeds the endogenous antioxidant capacity (2,3). The ROS-mediated oxidation of cell biochemicals, such as lipids, proteins, and DNA, might result in the alteration of cell viability, further compromised by oxidative stress-induced inflammation, gliosis, and microglial activation (4). These mechanisms ultimately influence the activation of apoptosis in retinal cells, leading further to functional loss (5). In this respect, photoreceptors have been demonstrated to be the first cell type to show the signs of damage associated to prolonged intense light exposures (6). Since photoreceptor degeneration characterizes several retinal diseases, experimental models of photo-oxidative damage, or retinal light damage (LD), have been used to mimic human retinal degenerations arising from environmental and genetic insults, which are based primarily on similar morphological and molecular outcomes. For example, the degeneration of photoreceptors observed in LD models results in the functional loss observed in many retinal disorders, including retinitis pigmentosa and age-related macular degeneration (AMD) (7). Furthermore, oxidative stress and chronic inflammation are also pathophysiological events involved in these diseases (8,9). The advantage of these models in studying photoreceptor degeneration is that light exposure can be regulated according to experimenter necessities, to control the induction, timing, and extent of photoreceptor death. Indeed, the exposure to intense visible light simultaneously triggers cell death mechanisms in a large number of photoreceptors, leading to the synchronization of photoreceptor degeneration facilitating the detection and the analysis (10). Therefore, the use of LD models instead of models of inherited retinal degeneration, where cell death proceeds rather slowly and progressively, could be functional to study minimal changes in levels, localization, modifications and activity of factors involved in the regulation of photoreceptor damage (10). Moreover, the effects of a putative either preventive or curative treatment could be easily assessed in a relatively short time frame, given the large-scale degeneration and the possibility to modulate the severity of damage. In this section, an exemplificative protocol of exposure to high levels of white light in albino rats is described. Then, the description of some main exemplificative outcomes deriving from the application of this protocol is provided, as well as practical suggestions used to assess the described topics.
Experimental protocol
Required material
- A room or box for dark adaptation. Any light-tight room or box sufficiently large to contain at least one normal animal cage with appropriate ventilation could be used.
- 1% tropicamide eye drops (Atropine; Allergan S.p.A., Rome, Italy).
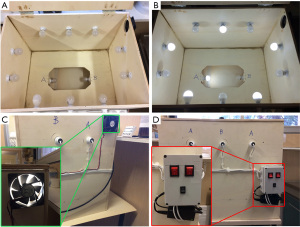
- Light exposure apparatus (an example of our custom-made device is shown in Figure 1). The light exposure device shown here is custom-made, but any apparatus provided with light bulbs might work if sufficient high levels of light can be reached. The light exposure device here consists of a wooded box (dimensions 72 cm × 61 cm × 52 cm) provided with twelve light LED bulbs, ten of them placed on the lateral walls and two at the cage bottom (Figure 1A,1B). Our apparatus is also provided with a cooling aeration system composed by a small air fan to keep the temperature constantly at (25±1.5 °C) (Figure 1C). The switching of both light bulbs and cooling system is controlled through a button system (Figure 1D). The animal cages could be placed in the middle of the apparatus, and up to two small cages could be inserted at the same time.
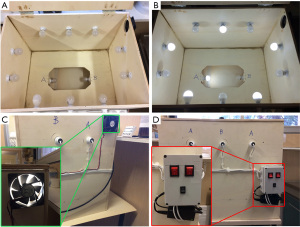 Figure 1 An example of custom-made light apparatus for the light exposure protocol. (A,B) Images showing the disposition of the twelve light bulbs, ten on the lateral walls of the box and two at the bottom, when the bulbs are all turned off (A) or (B) on in half, to reach a light intensity of 1,000 lux. (C) Representative photograph of the external lateral view of the light box apparatus showing connections between the bulbs and the interruptor, as well as the small fan composing the cooling system. A detailed magnification of the small fan is shown in the green square. (D) Representative photograph of the external frontal view of the light box apparatus showing connections between the bulbs and the interruptor, as well as the switching system composed of three buttons. A detailed magnification of the switching system is shown in the red square. The red buttons on the upper side control the switching of a group of six bulbs each. The small black button on the lower side controls the air fan activity.
Figure 1 An example of custom-made light apparatus for the light exposure protocol. (A,B) Images showing the disposition of the twelve light bulbs, ten on the lateral walls of the box and two at the bottom, when the bulbs are all turned off (A) or (B) on in half, to reach a light intensity of 1,000 lux. (C) Representative photograph of the external lateral view of the light box apparatus showing connections between the bulbs and the interruptor, as well as the small fan composing the cooling system. A detailed magnification of the small fan is shown in the green square. (D) Representative photograph of the external frontal view of the light box apparatus showing connections between the bulbs and the interruptor, as well as the switching system composed of three buttons. A detailed magnification of the switching system is shown in the red square. The red buttons on the upper side control the switching of a group of six bulbs each. The small black button on the lower side controls the air fan activity. - Light LED bulbs.
- A digital illuminance meter (Dr.Meter, Ahern Ave, Union City, CA, USA).
- Sodium pentobarbital (30 mg/kg) for euthanasia.
Light exposure protocol
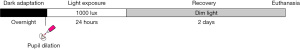
A schematic representation of this protocol is reported in Figure 2.
- Keep the animals in cages with food and water ad libitum in a normal 12 h/12 h light-dark cycle environment. Preliminary check the light intensity reached by light bulbs through the illuminance meter to assure the correct intensity. Establish the number of light bulbs that needs to be turned on to reach the right intensity. Measure light levels by placing the light-sensitive head of the illuminance meter face-up into the middle of one exposure cage provided with grid and water to count any possible interference. Then, adjust the distance between light bulbs and cages to reach the proper light intensity.
- Note 1: always use the same illuminance meter. Measurements may vary considerably depending on the shape of the light-sensitive head of the instrument. Do not dim the light bulbs to reduce intensity, since dimming may alter the wavelength of the emitted light. Change the distance between exposure cages and light bulbs instead.
- Dark adapted the animals for 16 h overnight. Start approximately at 6 pm.
- Note 2: to minimize the transport before the exposure, it is advisable to house and dark adapt the animals close to the room with the light apparatus (if the room was the same, it would be better). Try not to mix the animals during dark adaptation since it might cause stress.
- Dilate pupils by the application of 1% tropicamide eye drops before starting the light exposure. After the application of the drug, replace the animals in their cages and keep them in dark adaptation for other 30 min. Before placing the animals in a small cage and putting them in the light box, assure that dilation of pupils correctly occurred.
- Note 3: the procedure should be performed in dim red light. The animals should not be stressed as much as possible.
- Place the animals in a small chamber into the light apparatus. Switch the light bulbs and the cooling system on. Start at 10 am. Turn the proper number of light bulbs on to reach the light intensity of 1,000 lux. Check if the adequate light intensity is reached at cage level. If not, change the distance between cage and light source until the required intensity is achieved.
- Note 4: it is advisable to leave only one animal in each small cage, without any lid or food which could influence light intensity at cage level. Leave at least a small transparent bottle with water to avoid animal dehydration. One animal per cage should be placed since animals tend to stick together if they are more than one in the cage. To guarantee the highest reproducibility, start the protocol during the same time of the day. Circadian variations in LD susceptibility should be considered (11).
- Leave the animals in the light box with the lights on for 24 h. Control the animals frequently to check their health status.
- Note 5: this procedure could be applied for other light exposure paradigms, changing either the time of exposure or the intensity of light, as well as the wavelength of the incident light changing the type of emitted bulbs. In deciding each parameter, consider the factors which could influence the severity of damage. Indeed, the susceptibility to LD is reported to be influenced by several factors, such as pigmentation, genetic background, age, and specific wavelength of the exposed light (10). Moreover, different time exposures or light intensities could result in diverse severity of photoreceptor damage and loss (10). Therefore, adjust the light exposure paradigm based on the experimental needs.
- After 24 h of exposure, remove the animals from the light apparatus and keep them in normal cages with food and water ad libitum in dim light, until the rats are euthanized through a lethal injection of sodium pentobarbital for the analysis.
- Note 6: possible treatment protocols using this model could be performed either before or after the light exposure, based on the intention of the experimenter to test preventive or curative effects, respectively. Several modalities could be followed to administer the substance of interest. For example, intravitreal or intraperitoneal injections could be used, as well as oral supplementation by gavage. Treatment strategies, doses and modalities should be considered according to the experimental needs.
Examples of outcomes from the LD model in the rat
Retinal dysfunction
Retinal functional alterations following the experimental light paradigm can be evaluated by electroretinogram (ERG) from two days after light exposure. For instance, a full-field ERG can be performed to assess the activity of the entire retina in animals exposed to the intense light (12). The analysis could be performed non-invasively placing electrodes pairs on the corneal surface. Following a given light stimulus, positive and negative components of the recorded ERG wave indicate the summed activity of the potentials arising from different phases of retinal processing (12). ERG analyses should be performed under systemic anesthesia, although even a local anesthesia with eye drops, such as lidocaine, is advisable to prevent the animals from blinking. The dark-adapted scotopic ERG is one of the most widely used ERG analyses to evaluate retinal function (12). The recorded scotopic ERG wave comprises two main components. Indeed, after the light onset, an initial negative component (a-wave), corresponding to the photoreceptor contribution, is followed by a second positive-going b-wave from post-receptor retina (12). The considered light exposure protocol has been observed to reduce the amplitude of scotopic a- and b-waves of about 85–90% after LD (13-15). Moreover, longitudinal evaluation of LD-driven functional impairment during time revealed a partial recovery, maximal at 45 days, underlining a further deterioration after this time point, with no other recovery events (13,14).
Photoreceptor damage and degeneration
The exposure to intense light induces biochemical changes in photoreceptors, resulting in cell damage and, consequently, death (16). The evaluation of photoreceptor death is one of the key features to analyze after a light exposure protocol, especially if a neuroprotective strategy is tested on these models. Such an evaluation could be performed at the molecular level, through the assessment of apoptotic markers’, upregulation, as well as by histological analyses which allow the quantification of dying cells among retinal layers. For example, the increase in pro-apoptotic molecules, as well as the activation of apoptotic-promoting caspases, could be measured by Western blot. The light exposure protocol has been reported to result in an increased pro-apoptotic Bax and cleaved caspase-3 levels even after 2 days of recovery in dim light (15). Then, the molecular analyses could be supported by immunohistochemical approaches, evaluating apoptotic-mediated DNA fragmentation by terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay (14,15,17). In this respect, the increase in TUNEL positive cells could be detected even after 24 h of light exposure, then declining progressively within the first week of recovery in dim light, probably due to the progressive loss of cells (18,19). Photoreceptor degeneration occurring in this model is underlined ultimately by the thinning of outer nuclear layer (ONL) (16). Histological alterations in retinal layers after light exposure could be assessed by the labeling of retinal cell nuclei with 4',6-diamidino-2-phenylindole (DAPI) and the further quantification of ONL thickness on cross sections (15). Alternatively, the number of photoreceptor nuclei rows could be used as a measure of variations in ONL thickness (14). When evaluating the ONL thickness, the measure could be also expressed as the ratio between ONL to total retinal thickness, in order to account for putative oblique sectioning. In addition, the assessment of the thickness could be performed across either the entire retina or hemiretina (superior or inferior retina) by measuring across different eccentricities from the optic nerve (ON) and reporting the values as a function of the distance from ON (14). The light exposure protocol has been reported to induce the thinning of ONL, demonstrating a region-dependent loss of photoreceptors. Indeed, the most susceptible retinal region to LD is placed at the dorsal retina, in proximity of the so-called “hot-spot” (14,16). Unlike functional recovery, morphological alterations persisted during time (14).
Retinal oxidative stress
One of the most important pathophysiological mechanisms determining photoreceptor death in LD is oxidative stress. Indeed, the excessive light exposure promotes a series of biochemical changes leading to the overproduction of ROS, which in turn can impair cell structure and function (4). In this context, ROS overproduction drives the activation of an endogenous antioxidant response, mediated by ROS-sensitive transcription factors, such as nuclear factor erythroid 2-related factor 2 (Nrf2), which in turn increase the production of antioxidant enzymes, such as heme oxygenase-1 (HO-1) (20,21). This occurs as a homeostatic response to counteract overproduction of ROS in the retina following light exposure. Therefore, to assess retinal oxidative stress it could be possible to either measure directly ROS levels through dedicated assays or, alternatively, evaluate putative changes in the levels of antioxidant markers as a response to increased ROS. In this respect, molecular analyses either at transcriptional or protein level could be useful to assess increments in antioxidant markers following LD. In the LD rats, protein levels of Nrf2, as well as HO-1, have been observed to increase even after 2 days of recovery in dim light after excessive light exposure (15).
Retinal gliosis and inflammation
LD protocol results in retinal gliosis and inflammation. The activation of retinal gliosis could be assessed through immunohistochemical analyses labeling retinal cross sections for reactive Müller cells [e.g., glial fibrillary acidic protein (GFAP)] and active microglial [e.g., ionized calcium-binding adapter molecule 1 (Iba1)] markers (15). Strong retinal upregulation of GFAP could be observed in LD model after 2 days of recovery in dim light, especially in Müller cells processes among retinal layers (15), further amplified during the first week of recovery (14,17). Moreover, the increase in GFAP fluorescence intensity was still observed even at later stages of recovery (14). Likewise, microglial activation, indicated by the increase in Iba1 positive cells, as well as the changed cell shape into active ameboid and the cell migration towards injured sites, was evidently detectable after 2 days of recovery and persisted until 60 days especially in dorsal retina (14,15). In addition, the activation of inflammatory processes, suggested by retinal gliosis and microglial activation, could be supported with molecular analysis of pro- and anti-inflammatory cytokines at transcriptional and protein levels. For example, qPCR, Western blot, and ELISA analyses suggested an upregulation of pro-inflammatory cytokines, such as interleukin 1 beta (IL-1β), interleukin 6 (IL-6) and tumor necrosis α (TNF-α), as well as a downregulation of anti-inflammatory molecules [e.g., interleukin 10 (IL-10)] after light exposure (15,18,19).
Discussion and conclusions
Retinal photoreceptor death is a feature common to different retinal diseases, such as retinitis pigmentosa and AMD (22). Therefore, the use of animal models mimicking photoreceptor degeneration could be fundamental to study the pathophysiological events and test the efficacy of neuroprotective treatments useful for both the diseases. The existence of many animal models of inherited retinal degeneration allows the study of cellular, biochemical, and molecular mechanisms responsible for photoreceptor death (7). However, the degeneration is rather slowly in these models and completes after several weeks to months. Thus, only a small number of cells are in the same dying stage throughout the degeneration, making the detection of subtle changes in levels, localization, and activity of involved molecules difficult (10).
It was demonstrated that an intense exposure to light can trigger oxidative stress, resulting in biochemical changes and ultimately leading to photoreceptor death (16). Therefore, it is possible to reproduce photoreceptor degeneration in animal models through the exposure of bright intense light. The pathophysiological processes observed in these models faithfully resemble the features of human retinal degenerations, making them a useful tool in studying disease mechanisms and treatments (8). The possibility to manipulate and control the severity of damage and the degeneration of photoreceptors, provides an advantage of LD lesions compared to genetical models. Indeed, the exposure to intense bright light can induce the synchronized activation of apoptosis in photoreceptors in a large area, which allows the evaluation of cellular and molecular events in a controlled fashion, facilitating the detection and the analysis (10). Moreover, protocols with various time exposures or light intensities can result in different severity of photoreceptor degeneration, possibly allowing a controlled gradeability of cell death (10). By varying the exposure parameters, such as the intensity of exposed light and the duration of the exposure, it is possible to obtain a certain degree of damage allowing the study of different features of the disease. For example, the exposure to different intensities of cold white light from 500 to 1,500 lux for 24 h has been observed to result in a dose-dependent loss of photoreceptors, with the superior retina displaying the most susceptibility to damage (23). Thus, the more intense the exposed light, the more severe the damage and the loss of photoreceptors might be. Furthermore, also modifying the time of exposure to a fixed light intensity might regulate the severity of damage. In this respect, an exposure to 1,000 lux of white light for 12 h has been observed to result in functional impairment and retinal gliosis, without any evident morphological changes and microglial activation. On the other hand, a longer exposure for 24 h at the same intensity has been demonstrated to induce even morphological alterations and microglial activation (14). Therefore, it is possible to adapt the exposure paradigm to the experimental needs, and the researcher has to evaluate what degree of damage should be obtained in order to study different mechanisms.
Despite their advantages, limitations of LD models which could influence the severity of damage should be considered. A series of variables must be carefully checked to establish the appropriate exposure paradigm able to reproduce the right intensity of damage. For instance, a higher susceptibility to LD was reported in older animals, demonstrating an age-dependent relationship (24). Moreover, also genetic background, strain differences and ocular pigmentation could influence the animal susceptibility to LD (10,24). Finally, an important attention should be paid on possible circadian variations in LD response. Indeed, LD susceptibility has been reported to depend on circadian variations (11). Thus, it is recommended to consider all of these variables in choosing the correct exposure paradigm, in order to have a protocol able to induce the needed effects without a high variability.
In conclusion, despite the variability introduced by these factors, LD models represent a useful tool to study the mechanisms responsible for photoreceptor degeneration. Thanks to the possibility to regulate the severity of damage and burst a synchronized apoptosis of photoreceptors, LD models are suitable to study degenerative mechanisms in a short time frame, in contrast to the longer times given by the slow-rated degenerative models. Nonetheless, it is still possible to adjust the exposure paradigm to obtain functional impairments without morphological outcomes, allowing the study of the early mechanisms behind LD-induced degeneration. Thus, it is important to choose the protocol according to the experimental needs, and the wide range of variables and limitations influencing the final outcomes should be taken into account to achieve proper results. In this respect, this study protocol seeks to provide basic guidelines of how a photo-oxidative damage is performed, using the described protocol as an example from the literature, and introduce the variables and limitations to give a critical overview of the factors to consider when choosing the right protocol. Thus, this study protocol should be considered as a starting tool for a critical beginning to the colleagues who want to approach with LD models, whose further details will be deepened by the literature of the chosen topic.
Acknowledgments
I thank Dr. Alberto Melecchi for the critical reading and the important suggestions for this manuscript.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Dario Rusciano) for the series “Preclinical Models in Ophthalmic Research” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (https://aes.amegroups.com/article/view/10.21037/aes-21-50/coif). The series “Preclinical Models in Ophthalmic Research” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wenzel A, Grimm C, Samardzija M, et al. Molecular mechanisms of light-induced photoreceptor apoptosis and neuroprotection for retinal degeneration. Prog Retin Eye Res 2005;24:275-306. [Crossref] [PubMed]
- Maeda T, Maeda A, Matosky M, et al. Evaluation of potential therapies for a mouse model of human age-related macular degeneration caused by delayed all-trans-retinal clearance. Invest Ophthalmol Vis Sci 2009;50:4917-25. [Crossref] [PubMed]
- B Domènech E. Marfany G. The Relevance of Oxidative Stress in the Pathogenesis and Therapy of Retinal Dystrophies. Antioxidants (Basel) 2020;9:347. [Crossref]
- Hunter JJ, Morgan JI, Merigan WH, et al. The susceptibility of the retina to photochemical damage from visible light. Prog Retin Eye Res 2012;31:28-42. [Crossref] [PubMed]
- Ouyang X, Yang J, Hong Z, et al. Mechanisms of blue light-induced eye hazard and protective measures: a review. Biomed Pharmacother 2020;130:110577. [Crossref] [PubMed]
- Rózanowska M, Sarna T. Light-induced damage to the retina: role of rhodopsin chromophore revisited. Photochem Photobiol 2005;81:1305-30. [Crossref] [PubMed]
- Samardzija M, Neuhauss SCF, Joly S, et al. Animal models for retinal degeneration. In: Pang IH, Clark AF. editors. Advances in experimental medicine and biology, Retinal degenerative diseases. New York: Humana, 2010:52-80.
- Rozanowska MB. Light-induced damage to the retina: current understanding of the mechanisms and unresolved questions: a symposium-in-print. Photochem Photobiol 2012;88:1303-8. [Crossref] [PubMed]
- Newton F, Megaw R. Mechanisms of Photoreceptor Death in Retinitis Pigmentosa. Genes (Basel) 2020;11:1120. [Crossref] [PubMed]
- Grimm C, Remé CE. Light damage as a model of retinal degeneration. Methods Mol Biol 2013;935:87-97. [Crossref] [PubMed]
- Organisciak DT, Darrow RM, Barsalou L, et al. Circadian-dependent retinal light damage in rats. Invest Ophthalmol Vis Sci 2000;41:3694-701. [PubMed]
- Frishman L, Wang MH. Electroretinogram of Human, Monkey and Mouse. In: Kaufman PL, Alm A. editors. Adler’s physiology of the eye. Edinburgh: Elsevier, 2011:480-501.
- Tisi A, Parete G, Flati V, et al. Up-regulation of pro-angiogenic pathways and induction of neovascularization by an acute retinal light damage. Sci Rep 2020;10:6376. [Crossref] [PubMed]
- Riccitelli S, Di Paolo M, Ashley J, et al. The Timecourses of Functional, Morphological, and Molecular Changes Triggered by Light Exposure in Sprague-Dawley Rat Retinas. Cells 2021;10:1561. [Crossref] [PubMed]
- Amato R, Canovai A, Melecchi A, et al. Dietary Supplementation of Antioxidant Compounds Prevents Light-Induced Retinal Damage in a Rat Model. Biomedicines 2021;9:1177. [Crossref] [PubMed]
- Organisciak DT, Vaughan DK. Retinal light damage: mechanisms and protection. Prog Retin Eye Res 2010;29:113-34. [Crossref] [PubMed]
- Di Marco F, Di Paolo M, Romeo S, et al. Combining neuroprotectants in a model of retinal degeneration: no additive benefit. PLoS One 2014;9:e100389. [Crossref] [PubMed]
- Jiao H, Natoli R, Valter K, et al. Spatiotemporal Cadence of Macrophage Polarisation in a Model of Light-Induced Retinal Degeneration. PLoS One 2015;10:e0143952. [Crossref] [PubMed]
- Rutar M, Natoli R, Chia RX, et al. Chemokine-mediated inflammation in the degenerating retina is coordinated by Müller cells, activated microglia, and retinal pigment epithelium. J Neuroinflammation 2015;12:8. [Crossref] [PubMed]
- Wang Y, Huo Y, Zhao L, et al. Cyanidin-3-glucoside and its phenolic acid metabolites attenuate visible light-induced retinal degeneration in vivo via activation of Nrf2/HO-1 pathway and NF-κB suppression. Mol Nutr Food Res 2016;60:1564-77. [Crossref] [PubMed]
- Okamoto T, Kawashima H, Osada H, et al. Dietary Spirulina Supplementation Protects Visual Function From Photostress by Suppressing Retinal Neurodegeneration in Mice. Transl Vis Sci Technol 2019;8:20. [Crossref] [PubMed]
- Remé CE, Grimm C, Hafezi F, et al. Why study rod cell death in retinal degenerations and how? Doc Ophthalmol 2003;106:25-9. [Crossref] [PubMed]
- Krigel A, Berdugo M, Picard E, et al. Light-induced retinal damage using different light sources, protocols and rat strains reveals LED phototoxicity. Neuroscience 2016;339:296-307. [Crossref] [PubMed]
- Polosa A, Bessaklia H, Lachapelle P. Strain Differences in Light-Induced Retinopathy. PLoS One 2016;11:e0158082. [Crossref] [PubMed]
Cite this article as: Canovai A. Experimental model of photo-oxidative damage. Ann Eye Sci 2022;7:19.