
Vitreoretinal surgical training—assessment of simulation, models, and rubrics—a narrative review
Introduction
Vitreoretinal surgical training involves detailed development and refinement of unique surgical maneuvers in handling retina pathology. Ophthalmology residents and vitreoretinal surgical fellows are expected to perform a minimum number of retinal procedures for completion of training. While traditional training techniques have involved didactics and supervised surgical mentorship, there is a lack of standardized surgical curricula for attaining surgical milestones and feedback in vitreoretinal surgery among institutions. As a result, there has been an increased interest into utilizing novel training modalities for ophthalmological procedures like vitreoretinal surgery.
While several studies have been published documenting various surgical tools for cataract surgery training, there have been limited reviews into the efficacy of unique surgical training instruments and modalities for vitreoretinal surgery (1-5). We aim to present a comprehensive review of available training modules for vitreoretinal surgery and broaden understanding of the unique utility and practicality of these modalities in developing standardized ways to teach vitreoretinal surgery. We present the following article in accordance with the Narrative Review reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-21-43/rc).
Methods
A PubMed literature review was performed to search for relevant review articles ranging from January 1978–December 2020 for publications in English discussing surgical simulation, eye models, and rubrics for vitreoretinal surgery. The search strategy is presented in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search (specified to date, month and year) | May 21, 2021 |
| Databases and other sources searched | PubMed |
| Search terms used (including MeSH and free text search terms and filters) | Surgical simulation, eye models, surgical rubrics, Eyesi, vitreoretinal surgery training |
| Timeframe | January 1978–December 2020 |
| Inclusion and exclusion criteria (study type, language restrictions etc.) | Inclusion: |
| ● English publication, discusses vitreoretinal surgery in relation to either surgical simulation, eye models, or surgical rubrics | |
| Exclusion: | |
| ● Non-English publications, surgical training studies | |
| ● Not discussing vitreoretinal surgery | |
| Selection process (who conducted the selection, whether it was conducted independently, how consensus was obtained, etc.) | The authors reviewed the papers involved and agreed to review them based upon their role in surgical models, simulators and rubrics for vitreoretinal surgery |
Discussion
Simulators
Vitreoretinal surgical simulation training allows trainees to develop and hone surgical skillset outside of the operating room. Several studies have assessed the utility and practicality of surgical simulation in ophthalmological training. Of note, the Eyesi Surgical (VRmagic, Mannheim, Germany) simulation system is a virtual reality simulator developed for training intraocular procedures (1). This eye simulator model has been assessed and validated in numerous studies for various intraocular procedures. The simulator involves training modules for both anterior and posterior segment surgeries. It consists of a mannequin head with model eye with operating microscope.
The Eyesi vitreoretinal surgical model has been shown to be highly efficacious in numerous systematic review studies (1-5). These studies investigated specific micro-surgical skills, such as navigation, membrane peeling, forceps utilization, and laser coagulation. The Eyesi is noted to provide feedback and assessment for the surgeon. These studies highlighted the development of a learning curve for vitreoretinal surgical tasks with continued repetition on the device simulation.
These review studies suggest that the Eyesi simulator may assist in overall improvement of both basic and complex surgical skillets for vitreoretinal surgery (1-5). These studies were able to delineate skillset differences between novice and expert surgeons, including in areas of navigation and membrane peeling. Jonas et al. demonstrated that utilization of simulator by surgeon resulted in enhanced skillset than in the absence of simulation training (6). These suggest that continued use of surgical simulation for vitreoretinal surgery can improve in-simulation skillset, with presumed translation to the operating room by improving surgical exposure without compromising patient care. While cost and access to virtual simulators may limit their current impact on training programs, future studies could assess residents and fellows in their surgical objective skillset and subjective confidence after use of Eyesi vitreoretinal surgical training modules. These simulations may assist in providing standardized training avenues for residents and fellows during periods of decreased patient volume, such as during the COVID-19 pandemic.
Eye models
In addition to virtual simulators, eye models (animal, cadaveric, or artificial) have been noted to be of significant benefit towards ophthalmological surgical training. With regards specifically to vitreoretinal surgery, eye models have been utilized to simulate various steps of surgery. Rabbit eyes have been used to demonstrate practice with vitrectomy (7,8). Barth et al. developed treatment model of rhegmatogenous retinal detachments using rabbit model and utilization of vitreous-analog tamponades (9). Cadaveric eyes have been utilized for modeling vitrectomy, however their use is limited by corneal edema. This can be addressed in part by placement of keratoprosthesis (8,10).
While animal and cadaveric eye models have been shown to have value for ophthalmological training, handling, storage, and disposal of this tissue may present limitations. In recent years, the advent of novel artificial eye models has not only aided in simulating microsurgical techniques like membrane peeling, but also presented potentially cost-effective and reusable practice eye models. Examples of artificial eye models include Kitaro WetLab (Frontier Vision Co., Ltd., Hyogo, Japan), Phake-i (Eye Care and Cure, Tucson, AZ, USA), and BIONIKO models (BIONIKO, Aventura, FL, USA) (11-14).
These models aim to simulate various aspects of both anterior and posterior surgery outside of the operating room. However, they do have limitations in their efficacy. For example, while models like the Phake-i allow for simulation of ERM and ILM peeling using polydimethylsiloxane (PDMS) films, the eye model is not filled with fluid (11,13). It provides an opportunity to allow for simulation and practice of intraocular maneuvers with forceps, but hinders the simulation of operating in a fluidic environment. Other dry lab vitreoretinal eye models include RetiSurge, a 3D printed eye model (15).This eye model allows for simulation of instrumentation and endolaser using polyethylene terephthalate glycol (PETG) film in a dry environment. While these models allow for practice of dexterity and bimanual manipulation for trainee surgeons, the models should not be presumed to translate into direct experience of operating on true tissue. Currently, no studies exist to demonstrate the perceived effectiveness in improving skillset with these specific eye models.
To address the concerns of dry models, several artificial eyes have been developed to simulate a wet environment. Arai et al. created an artificial eye for ILM peeling under fluidic conditions (11). To improve the realistic sensory feedback of replicating the fundus and ILM (PVA hydrogel film), various thicknesses were tested for simulated ILM film to ascertain the most similar to reality.
Moreover, in a prospective study performed at Casey Eye Institute, the VitRet Eye Model (Phillips Studio, Bristol, UK) was utilized along with a designed vitreoretinal training module (16). This eye model was noted to have a vitreous-like fluid introduced, as well as presence of artificial epiretinal membrane for membrane peeling.
These ocular surgery simulators allow for additional training opportunities for novice surgeons to help enhance and fine-tune their vitreoretinal surgical skills. Hands-on training in an era of decreased surgical volume and limitations is salient to ensure future physicians are continuing to develop top surgical competency. Table 2 collectively reviews the benefits and drawbacks of various simulation and eye models discussed. Additional studies and surveys to assess trainee satisfaction and utility with various eye models and simulators would benefit to see which educational modalities would be most helpful for ophthalmology residents and fellows.
Table 2
| Training tool | Benefits | Limitations |
|---|---|---|
| Virtual simulator (Eyesi) | Multiple modules, feedback, learning curve tracking, repetitive use | Cost, access for programs |
| Eye model—animal | Allows tissue handling, navigation, maneuvering in actual eye | Difficulty with membrane peeling, requires proper handling, storage, disposal |
| Eye model—cadaver | Allows tissue handling, navigation, maneuvering in actual eye | Corneal edema, requires proper handling, storage, disposal |
| Eye model—artificial (Dry) | Allows work in 3D environment, replicates membrane peeling in part, repetitive use | Does not represent fluidic environment for procedures, cost |
| Eye model—artificial (Wet) | Allows work in fluidic, 3D environment, Replicates membrane peeling, repetitive use | Cost |
Assessment rubrics
Currently, there are limited vitreoretinal surgical assessment rubrics available for training programs to assess resident and fellow skillset. In contrast to vitreoretinal surgery, there are several cataract surgical assessment tools available. While typical feedback may be provided to trainees during or after surgical procedure, certain aspects that require additional practice may fail to be emphasized.
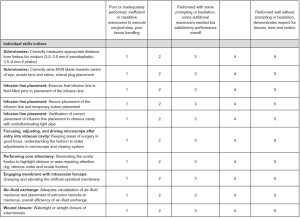
One example of vitreoretinal surgical training assessment rubric includes the Casey Eye Institute Vitrectomy Indices Tool for Skills Assessment (CEIVITS) (16). This five-point Likert scale provided a grading system to evaluate various facets of trainee’s skillset, including steps such as sclerotomy construction, infusion line placement, core vitrectomy, and even wound closure (Figure 1). This scoring system was used in the assessment of resident and fellow skillset utilizing the aforementioned VitRet Eye Model. The implementation of these types of scoring rubrics may allow for trainees to have feedback to improve upon the specific steps of vitreoretinal surgery, just as with cataract rubrics that breakdown the steps of cataract surgery for grading.
In addition to surgical feedback, rubrics have been developed to assess other aspects of managing posterior segment pathology. Ramasamy et al. developed the Ophthalmology Surgical Competency Assessment Rubric for Panretinal Photocoagulation (17). This rubric allows for a standardized method to teach, train, and assess panretinal photocoagulation. It has been utilized as a global rubric for teaching panretinal photocoagulation to trainees.
By developing these standardized rubrics, we may better provide a structured way to help train and focus dedicated time towards developing appropriate surgical habits and skillsets.
Conclusions
Novel modalities are continuing to develop for vitreoretinal surgical training. From virtual simulators to artificial eye models, trainees have access to unique educational tools that allow practice of complex microsurgical skills outside of the operating room. By utilizing simulators and rubrics, training programs may be able to provide a standardized curriculum to highlight the steps of vitrectomy and to provide adequate feedback. However, efficacy and improvement in surgical skillset that translates from training module to patient care remains to be established.
Prospective trials assessing resident and fellow skillset after utilization of specific models or simulators should be developed. Broadened development and use of vitreoretinal training rubrics will also aim to not only educate residents and fellows in surgical competency, but also provide a unique metric to track surgical growth and ultimately improve patient care.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ajay Singh and Jay M. Stewart) for the series “Medical and Surgical Challenges in Retina” published in Annals of Eye Science. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-21-43/rc
Peer Review File: Available at https://aes.amegroups.com/article/view/10.21037/aes-21-43/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-21-43/coif). The series “Medical and Surgical Challenges in Retina” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lee R, Raison N, Lau WY, et al. A systematic review of simulation-based training tools for technical and non-technical skills in ophthalmology. Eye (Lond) 2020;34:1737-59. [Crossref] [PubMed]
- Rasmussen RC, Grauslund J, Vergmann AS. Simulation training in vitreoretinal surgery: a systematic review. BMC Ophthalmol 2019;19:90. [Crossref] [PubMed]
- Koch F, Koss MJ, Singh P, et al. Virtual reality in ophthalmology. Klin Monbl Augenheilkd 2009;226:672-6. [Crossref] [PubMed]
- Park L, Song JJ, Dodick JM, et al. The EYESI 2.2 ophthalmosurgical simulator: is it a good teaching tool? Investig Ophthalmol Vis Sci 2006;47:4421.
- Rossi JV, Verma D, Fujii GY, et al. Virtual vitreoretinal surgical simulator as a training tool. Retina 2004;24:231-6. [Crossref] [PubMed]
- Jonas JB, Rabethge S, Bender HJ. Computer-assisted training system for pars plana vitrectomy. Acta Ophthalmol Scand 2003;81:600-4. [Crossref] [PubMed]
- Iyer MN, Han DP. An eye model for practicing vitreoretinal membrane peeling. Arch Ophthalmol 2006;124:108-10. [Crossref] [PubMed]
- Abrams GW, Topping T, Machemer R. An improved method for practice vitrectomy. Arch Ophthalmol 1978;96:521-5. [Crossref] [PubMed]
- Barth H, Crafoord S, Ghosh F. A New Retinal Detachment Treatment Model for Evaluation of Vitreous Tamponades. Curr Eye Res 2021;46:373-9. [Crossref] [PubMed]
- Borirak-chanyavat S, Lindquist TD, Kaplan HJ. A cadaveric eye model for practicing anterior and posterior segment surgeries. Ophthalmology 1995;102:1932-5. [Crossref] [PubMed]
- Omata S, Someya Y, Adachi S, et al. A surgical simulator for peeling the inner limiting membrane during wet conditions. PLoS One 2018;13:e0196131. [Crossref] [PubMed]
- Akura J, Pokharel K. Artificial lens for cataract surgery practice. 2011;WO Patent App. PCT/JP2010/ 002,630.
- Van Dalen JTW, Carda DD. Model human eye and face manikin for use therewith. 2012;US Patent App. 13/189,434.
- Bernal A. Ophthalmic surgical simulation system. 2016; US Patent App. 14/468,769.
- Chhabra K, Khanna V, Vedachalam R, et al. RetiSurge - Enabling "Dry Lab" vitreoretinal surgical training during COVID-19 pandemic. Indian J Ophthalmol 2021;69:982-4. [Crossref] [PubMed]
- Yeh S, Chan-Kai BT, Lauer AK. Basic training module for vitreoretinal surgery and the Casey Eye Institute Vitrectomy Indices Tool for Skills Assessment. Clin Ophthalmol 2011;5:1249-56. [PubMed]
- Law JC, Golnik KC, Cherney EF, et al. The Ophthalmology Surgical Competency Assessment Rubric for Panretinal Photocoagulation. Ophthalmol Retina 2018;2:162-7. [Crossref] [PubMed]
Cite this article as: Puri S, Mehta MC. Vitreoretinal surgical training—assessment of simulation, models, and rubrics—a narrative review. Ann Eye Sci 2022;7:13.


